Bartonella Henselae Detected in Malignant Melanoma, a Preliminary Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Diversity of Bartonella Species in Small Mammals in the Qaidam
www.nature.com/scientificreports OPEN Genetic diversity of Bartonella species in small mammals in the Qaidam Basin, western China Huaxiang Rao1, Shoujiang Li3, Liang Lu4, Rong Wang3, Xiuping Song4, Kai Sun5, Yan Shi3, Dongmei Li4* & Juan Yu2* Investigation of the prevalence and diversity of Bartonella infections in small mammals in the Qaidam Basin, western China, could provide a scientifc basis for the control and prevention of Bartonella infections in humans. Accordingly, in this study, small mammals were captured using snap traps in Wulan County and Ge’ermu City, Qaidam Basin, China. Spleen and brain tissues were collected and cultured to isolate Bartonella strains. The suspected positive colonies were detected with polymerase chain reaction amplifcation and sequencing of gltA, ftsZ, RNA polymerase beta subunit (rpoB) and ribC genes. Among 101 small mammals, 39 were positive for Bartonella, with the infection rate of 38.61%. The infection rate in diferent tissues (spleens and brains) (χ2 = 0.112, P = 0.738) and gender (χ2 = 1.927, P = 0.165) of small mammals did not have statistical diference, but that in diferent habitats had statistical diference (χ2 = 10.361, P = 0.016). Through genetic evolution analysis, 40 Bartonella strains were identifed (two diferent Bartonella species were detected in one small mammal), including B. grahamii (30), B. jaculi (3), B. krasnovii (3) and Candidatus B. gerbillinarum (4), which showed rodent-specifc characteristics. B. grahamii was the dominant epidemic strain (accounted for 75.0%). Furthermore, phylogenetic analysis showed that B. grahamii in the Qaidam Basin, might be close to the strains isolated from Japan and China. -

Novel Small Rnas Expressed by Bartonella Bacilliformis Under Multiple Conditions 2 Reveal Potential Mechanisms for Persistence in the Sand Fly Vector and Human 3 Host
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.04.235903; this version posted August 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Novel small RNAs expressed by Bartonella bacilliformis under multiple conditions 2 reveal potential mechanisms for persistence in the sand fly vector and human 3 host 4 5 6 Shaun Wachter1, Linda D. Hicks1, Rahul Raghavan2 and Michael F. Minnick1* 7 8 9 10 1 Program in Cellular, Molecular & Microbial Biology, Division of Biological Sciences, 11 University of Montana, Missoula, Montana, United States of America 12 2 Department of Biology and Center for Life in Extreme Environments, Portland State 13 University, Portland, Oregon, United States of America 14 15 16 17 * Corresponding author 18 E-mail: [email protected] (MFM) 19 20 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.04.235903; this version posted August 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 21 Abstract 22 Bartonella bacilliformis, the etiological agent of Carrión’s disease, is a Gram-negative, 23 facultative intracellular alphaproteobacterium. Carrión’s disease is an emerging but neglected 24 tropical illness endemic to Peru, Colombia, and Ecuador. B. bacilliformis is spread between 25 humans through the bite of female phlebotomine sand flies. -

09 Piqueras.Qxp
PERSPECTIVES INTERNATIONAL MICROBIOLOGY (2007) 10:217-226 DOI: 10.2436/20.1501.01.30 ISSN: 1139-6709 www.im.microbios.org Microbiology: a dangerous profession? Mercè Piqueras President, Catalan Association for Science Communication (ACCC), Barcelona, Spain The history of science contains many cases of researchers eases in Minorca from the year 1744 to 1749 to which is pre- who have died because of their professional activity. In the fixed, a short account of the climate, productions, inhabi- field of microbiology, some have died or have come close to tants, and endemical distempers of that island (T. Cadell, D. death from infection by agents that were the subject of their Wilson and G. Nicol, London, 1751), which he dedicated to research (Table 1). Infections that had a lethal outcome were the Society of Surgeons of His Majesty’s Royal Navy. usually accidental. Sometimes, however, researchers inocu- Minorcan historian of science Josep M. Vidal Hernández has lated themselves with the pathogen or did not take preventive described and carefully analyzed Cleghorn’s work in measures against the potential pathogen because they wanted Minorca and his report [43]. According to Vidal, what to prove their hypotheses—or disprove someone else’s— Cleghorn describes is “tertian” fever, which was the name regarding the origin of the infection. Here is an overview of given at the time to fever caused by malaria parasites with a several episodes in the history of microbiology since the mid periodicity of 48 hours. In fact, Cleghorn used quinine to nineteenth century involving researchers or workers in fields treat tertian fever (i.e, malaria), which was not eradicated related to microbiology who have become infected. -

Bartonella Henselae • Fleas and Black-Legged Ticks (Also Called Deer Ticks) of the Genus Ixodes May Serve As Vectors, but This Has Not Disease Agent: Been Proven
APPENDIX 2 Bartonella henselae • Fleas and black-legged ticks (also called deer ticks) of the genus Ixodes may serve as vectors, but this has not Disease Agent: been proven. • Bartonella henselae Blood Phase: Disease Agent Characteristics: • Agent found in endothelial cells and associated with RBCs in symptomatic cases • Gram-negative bacillus or coccobacillus, aerobic, • Occult bacteremia sometimes occurs in the absence nonmotile, nonspore-forming, facultatively intracel- of specific antibodies. lular bacterium • Order: Rhizobiales; Family: Bartonellaceae Survival/Persistence in Blood Products: • Size: 0.3-0.6 ¥ 0.3-1.0 mm • Nucleic acid: Approximately 1900 kb of DNA • A spiking study suggests that B. henselae added to RBCs can be recovered on solid media through 35 Disease Name: days of storage at 4°C. • Cat scratch disease • Cat scratch fever Transmission by Blood Transfusion: • Bacillary angiomatosis • Theoretical • Bacillary peliosis Cases/Frequency in Population: Priority Level: • 22,000 cases per year estimated in the US • Scientific/Epidemiologic evidence regarding blood • 2-6% in US blood donors safety: Theoretical • Cumulative seroprevalence of 7.1% to B. henselae and • Public perception and/or regulatory concern regard- B. quintana in US veterinary professionals ing blood safety: Absent • Public concern regarding disease agent: Very low Incubation Period: Background: • 3-10 days to appearance of papule at inoculation site; regional adenopathy may follow after a few weeks • In 1909,ALBartondescribed organisms that adhered to RBCs. Likelihood of Clinical Disease: • The name Bartonella bacilliformis was used for the • Relatively benign and self-limiting, lasting 6-12 weeks only member of the group identified before 1993. in the absence of antibiotic therapy • Several other species of Bartonella are known to infect humans, but at present, B. -

Table S5. the Information of the Bacteria Annotated in the Soil Community at Species Level
Table S5. The information of the bacteria annotated in the soil community at species level No. Phylum Class Order Family Genus Species The number of contigs Abundance(%) 1 Firmicutes Bacilli Bacillales Bacillaceae Bacillus Bacillus cereus 1749 5.145782459 2 Bacteroidetes Cytophagia Cytophagales Hymenobacteraceae Hymenobacter Hymenobacter sedentarius 1538 4.52499338 3 Gemmatimonadetes Gemmatimonadetes Gemmatimonadales Gemmatimonadaceae Gemmatirosa Gemmatirosa kalamazoonesis 1020 3.000970902 4 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas indica 797 2.344876284 5 Firmicutes Bacilli Lactobacillales Streptococcaceae Lactococcus Lactococcus piscium 542 1.594633558 6 Actinobacteria Thermoleophilia Solirubrobacterales Conexibacteraceae Conexibacter Conexibacter woesei 471 1.385742446 7 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas taxi 430 1.265115184 8 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas wittichii 388 1.141545794 9 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas sp. FARSPH 298 0.876754244 10 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sorangium cellulosum 260 0.764953367 11 Proteobacteria Deltaproteobacteria Myxococcales Polyangiaceae Sorangium Sphingomonas sp. Cra20 260 0.764953367 12 Proteobacteria Alphaproteobacteria Sphingomonadales Sphingomonadaceae Sphingomonas Sphingomonas panacis 252 0.741416341 -
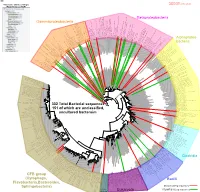
Bacteria Clostridia Bacilli Eukaryota CFB Group
AM935842.1.1361 uncultured Burkholderiales bacterium Class Betaproteobacteria AY283260.1.1552 Alcaligenes sp. PCNB−2 Class Betaproteobacteria AM934953.1.1374 uncultured Burkholderiales bacterium Class Betaproteobacteria AJ581593.1.1460 uncultured betaAM936569.1.1351 proteobacterium uncultured Class Betaproteobacteria Derxia sp. Class Betaproteobacteria AJ581621.1.1418 uncultured beta proteobacterium Class Betaproteobacteria DQ248272.1.1498 uncultured soil bacterium soil uncultured DQ248272.1.1498 DQ248235.1.1498 uncultured soil bacterium RS49 DQ248270.1.1496 uncultured soil bacterium DQ256489.1.1211 Variovorax paradoxus Class Betaproteobacteria Class paradoxus Variovorax DQ256489.1.1211 AF523053.1.1486 uncultured Comamonadaceae bacterium Class Betaproteobacteria AY706442.1.1396 uncultured bacterium uncultured AY706442.1.1396 AJ536763.1.1422 uncultured bacterium CS000359.1.1530 Variovorax paradoxus Class Betaproteobacteria Class paradoxus Variovorax CS000359.1.1530 AY168733.1.1411 uncultured bacterium AJ009470.1.1526 uncultured bacterium SJA−62 Class Betaproteobacteria Class SJA−62 bacterium uncultured AJ009470.1.1526 AY212561.1.1433 uncultured bacterium D16212.1.1457 Rhodoferax fermentans Class Betaproteobacteria Class fermentans Rhodoferax D16212.1.1457 AY957894.1.1546 uncultured bacterium AJ581620.1.1452 uncultured beta proteobacterium Class Betaproteobacteria RS76 AY625146.1.1498 uncultured bacterium RS65 DQ316832.1.1269 uncultured beta proteobacterium Class Betaproteobacteria DQ404909.1.1513 uncultured bacterium uncultured DQ404909.1.1513 AB021341.1.1466 bacterium rM6 AJ487020.1.1500 uncultured bacterium uncultured AJ487020.1.1500 RS7 RS86RC AF364862.1.1425 bacterium BA128 Class Betaproteobacteria AY957931.1.1529 uncultured bacterium uncultured AY957931.1.1529 CP000884.723807.725332 Delftia acidovorans SPH−1 Class Betaproteobacteria AY957923.1.1520 uncultured bacterium uncultured AY957923.1.1520 RS18 AY957918.1.1527 uncultured bacterium uncultured AY957918.1.1527 AY945883.1.1500 uncultured bacterium AF526940.1.1489 uncultured Ralstonia sp. -

Isolation of Francisella Tularensis from Skin Ulcer After a Tick Bite, Austria, 2020
microorganisms Case Report Isolation of Francisella tularensis from Skin Ulcer after a Tick Bite, Austria, 2020 Mateusz Markowicz 1,*, Anna-Margarita Schötta 1 , Freya Penatzer 2, Christoph Matscheko 2, Gerold Stanek 1, Hannes Stockinger 1 and Josef Riedler 2 1 Center for Pathophysiology, Infectiology and Immunology, Institute for Hygiene and Applied Immunology, Medical University of Vienna, Kinderspitalgasse 15, A-1090 Vienna, Austria; [email protected] (A.-M.S.); [email protected] (G.S.); [email protected] (H.S.) 2 Kardinal Schwarzenberg Klinikum, Kardinal Schwarzenbergplatz 1, A-5620 Schwarzach, Austria; [email protected] (F.P.); [email protected] (C.M.); [email protected] (J.R.) * Correspondence: [email protected]; Tel.: +43-1-40160-33023 Abstract: Ulceroglandular tularemia is caused by the transmission of Francisella tularensis by arthro- pods to a human host. We report a case of tick-borne tularemia in Austria which was followed by an abscess formation in a lymph node, making drainage necessary. F. tularensis subsp. holarctica was identified by PCR and multilocus sequence typing. Keywords: tularemia; Francisella tularensis; tick; multi locus sequence typing Depending on the transmission route of Francisella tularensis, tularemia can present Citation: Markowicz, M.; Schötta, as a local infection or a systemic disease [1]. Transmission of the pathogen takes place A.-M.; Penatzer, F.; Matscheko, C.; by contact with infected animals, by bites of arthropods or through contaminated water Stanek, G.; Stockinger, H.; Riedler, J. and soil. Hares and wild rabbits are the main reservoirs of the pathogen in Austria [2]. -

Rickettsia Felis, Bartonella Henselae, and B. Clarridgeiae, New Zealand
LETTERS Richard Reithinger,*† domestic and wild animals that also products obtained by PCR with Khoksar Aadil,† Samad Hami,† feeds readily on people. Recent stud- primers for the 17-kDa protein (4), and Jan Kolaczinski*† ies have implicated the cat flea as a citrate synthase (4), and PS 120 pro- *London School of Hygiene and Tropical vector of new and emerging infectious tein (5) genes. R. felis has been estab- Medicine, London, United Kingdom; and diseases (1). To determine the lished in tissue culture (XTC-2 and †HealthNet International, Peshawar, pathogens in C. felis in New Zealand, Vero cells) (6), and serologic testing Pakistan we collected 3 cat fleas from each of has been used to diagnose infections 11 dogs and 21 cats at the Massey (5). Reports indicate that patients References University Veterinary Teaching respond rapidly to doxycycline thera- 1. Ashford R, Kohestany K, Karimzad M. Hospital from May to June 2003. The py (5), and in vitro studies have Cutaneous leishmaniasis in Kabul: observa- fleas were stored in 95% alcohol until shown the organism is susceptible to tions on a prolonged epidemic. Ann Trop Med Parasitol 1992;86:361–71. they were identified by using morpho- rifampin, thiamphenicol, and fluoro- 2. Griffiths WDA. Old World cutaneous leish- logic criteria and washed in sterile quinolones. maniasis. In: Peters W, Killick-Kendrick R, phosphate-buffered saline. The DNA B. henselae is an agent of cat- editors. The leishmaniases in biology and from each flea was extracted individ- scratch disease, bacillary angiomato- medicine. London: Academic Press; 1987. p. 617–43. ually by using the QiaAmp Tissue Kit sis, bacillary peliosis, endocarditis, 3. -

Emerging Bartonellosis Christoph Dehio & Anna Sander
Emerging bartonellosis Christoph Dehio & Anna Sander Bartonellae are arthropod-borne pathogens of they cause a long-lasting infection within the red blood Ggrowing medical importance. Until the early cells (intraerythrocytic bacteraemia). Blood-sucking 1990s, only two species of this bacterial genus, arthropod vectors transmit the bacteria from this reservoir B. bacilliformis and B. quintana, were recognized as caus- to new hosts. Incidental infection of non-reservoir hosts ing disease in humans. In addition to re-emergence of the (e.g. humans by the zoonotic species) may cause disease, human-specific B. quintana, a number of zoonotic but does not result in intraerythrocytic infection. Bartonella species have now been recognized as causative agents for a broadening spectrum of diseases that can be Natural history and epidemiology transmitted to humans from their animal hosts. Most Humans are the only known reservoir for two Bartonella prominently, B. henselae is an important zoonotic species, B. bacilliformis and B. quintana. pathogen that is frequently passed from its feline B. quintana was a leading cause of infectious morbidity reservoir to humans. among soldiers during World War I, and recurred on the Bacteria of the genus Bartonella are Gram-negative, East European front in World War II. The disease, pleomorphic, fastidious bacilli that belong to the α-2 Trench fever, is rarely fatal and is characterized by an subclass of Proteobacteria. All Bartonella species appear intraerythrocytic bacteraemia with recurrent, cycling to have a specific mammalian species as a host, in which fever. It is transmitted among humans by the human body louse Pediculus humanus. Although almost forgotten Table 1. -

Laboratory Diagnostics of Rickettsia Infections in Denmark 2008–2015
biology Article Laboratory Diagnostics of Rickettsia Infections in Denmark 2008–2015 Susanne Schjørring 1,2, Martin Tugwell Jepsen 1,3, Camilla Adler Sørensen 3,4, Palle Valentiner-Branth 5, Bjørn Kantsø 4, Randi Føns Petersen 1,4 , Ole Skovgaard 6,* and Karen A. Krogfelt 1,3,4,6,* 1 Department of Bacteria, Parasites and Fungi, Statens Serum Institut (SSI), 2300 Copenhagen, Denmark; [email protected] (S.S.); [email protected] (M.T.J.); [email protected] (R.F.P.) 2 European Program for Public Health Microbiology Training (EUPHEM), European Centre for Disease Prevention and Control (ECDC), 27180 Solnar, Sweden 3 Scandtick Innovation, Project Group, InterReg, 551 11 Jönköping, Sweden; [email protected] 4 Virus and Microbiological Special Diagnostics, Statens Serum Institut (SSI), 2300 Copenhagen, Denmark; [email protected] 5 Department of Infectious Disease Epidemiology and Prevention, Statens Serum Institut (SSI), 2300 Copenhagen, Denmark; [email protected] 6 Department of Science and Environment, Roskilde University, 4000 Roskilde, Denmark * Correspondence: [email protected] (O.S.); [email protected] (K.A.K.) Received: 19 May 2020; Accepted: 15 June 2020; Published: 19 June 2020 Abstract: Rickettsiosis is a vector-borne disease caused by bacterial species in the genus Rickettsia. Ticks in Scandinavia are reported to be infected with Rickettsia, yet only a few Scandinavian human cases are described, and rickettsiosis is poorly understood. The aim of this study was to determine the prevalence of rickettsiosis in Denmark based on laboratory findings. We found that in the Danish individuals who tested positive for Rickettsia by serology, the majority (86%; 484/561) of the infections belonged to the spotted fever group. -

Some Organisms Which Are Risk Group 2 Can Be Particularly Hazardous To
Risk Groups of Microorganisms Note: Some organisms which are risk group 2 can be particularly hazardous to certain individuals and so a thorough understanding of the routes/ risk of infection, diseases caused is essential before any work is conducted with any microorganism. For example Rubella, Toxoplasma gondii and cytomegalovirus are all RG2 but are known to be teratogenic, so pregnant women or women that may be pregnant should not work with or be exposed to these organisms. Careful consideration of whether individuals that are immunosuppressed or on chemotherapy and or radiotherapy should be undertaken as these individuals may be at increased risk of infection. This list is not fully inclusive and is a modified from that in the Curtin University Biosafety manual. Bacteria Scientific name Risk Group Acinetobacter spp. 2 Aeromonas hydrophila 2 Bacillus anthracis 3 2 Bacillus cereus Bartonella henselae, quintana, vinsonii, elizabethiae, 2 weisii 3 Bartonella bacilliformis Bordetella pertussis 2 Borrelia spp. 2 Brucella ovis 2 3 Brucella spp. Burkholderia pseudomallei 2 3 Burkholderia mallei Campylobacter coli, fetus, jejuni 2 Chlamydia spp. 2 3 Chlamydia psittaci (avian) Clostridium botulinum 2 Clostridium tetani 2 Corynebacterium diphtheriae 2 2 Corynebacterium renale, pseudotuberculosis Coxiella burnetii (smears and serum samples) 2 3 Coxiella burnetii (cultures and concentrates) Edwardsiella tarda 2 Eikenella tarda 2 Enterococcus spp. (Vancomycin-resistant strains) 2 Erysipelothrix rhusiopathiae 2 Escherichia coli (pathogenic strains) 2 2 Escherichia coli VTEC strains (O157, O111) Francisella tularensis type A 3 Scientific name Risk Group Fusobacterium spp. 2 Gardnerella vaginalis 2 Haemophilus influenzae, ducreyi 2 Helicobacter pylori 2 Klebsiella spp. 2 Legionella spp. 2 Leptospira interrogans 2 Listeria monocytogenes 2 2 Listeria spp. -

Bartonella Henselae
Maggi et al. Parasites & Vectors 2013, 6:101 http://www.parasitesandvectors.com/content/6/1/101 RESEARCH Open Access Bartonella henselae bacteremia in a mother and son potentially associated with tick exposure Ricardo G Maggi1,3*, Marna Ericson2, Patricia E Mascarelli1, Julie M Bradley1 and Edward B Breitschwerdt1 Abstract Background: Bartonella henselae is a zoonotic, alpha Proteobacterium, historically associated with cat scratch disease (CSD), but more recently associated with persistent bacteremia, fever of unknown origin, arthritic and neurological disorders, and bacillary angiomatosis, and peliosis hepatis in immunocompromised patients. A family from the Netherlands contacted our laboratory requesting to be included in a research study (NCSU-IRB#1960), designed to characterize Bartonella spp. bacteremia in people with extensive arthropod or animal exposure. All four family members had been exposed to tick bites in Zeeland, southwestern Netherlands. The mother and son were exhibiting symptoms including fatigue, headaches, memory loss, disorientation, peripheral neuropathic pain, striae (son only), and loss of coordination, whereas the father and daughter were healthy. Methods: Each family member was tested for serological evidence of Bartonella exposure using B. vinsonii subsp. berkhoffii genotypes I-III, B. henselae and B. koehlerae indirect fluorescent antibody assays and for bacteremia using the BAPGM enrichment blood culture platform. Results: The mother was seroreactive to multiple Bartonella spp. antigens and bacteremia was confirmed by PCR amplification of B. henselae DNA from blood, and from a BAPGM blood agar plate subculture isolate. The son was not seroreactive to any Bartonella sp. antigen, but B. henselae DNA was amplified from several blood and serum samples, from BAPGM enrichment blood culture, and from a cutaneous striae biopsy.