Bartonella: Feline Diseases and Emerging Zoonosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bartonella Apis Sp. Nov., a Honey Bee Gut Symbiont of the Class Alphaproteobacteria
Serveur Academique´ Lausannois SERVAL serval.unil.ch Author Manuscript Faculty of Biology and Medicine Publication This paper has been peer-reviewed but does not include the final publisher proof-corrections or journal pagination. Published in final edited form as: Title: Bartonella apis sp. nov., a honey bee gut symbiont of the class Alphaproteobacteria. Authors: Keˇsnerov´aL, Moritz R, Engel P Journal: International journal of systematic and evolutionary microbiology Year: 2016 Jan Issue: 66 Volume: 1 Pages: 414-21 DOI: 10.1099/ijsem.0.000736 In the absence of a copyright statement, users should assume that standard copyright protection applies, unless the article contains an explicit statement to the contrary. In case of doubt, contact the journal publisher to verify the copyright status of an article. 1 Bartonella apis sp. nov., a honey bee gut symbiont of the 2 class Alphaproteobacteria 3 4 Lucie Kešnerová, Roxane Moritz, Philipp Engel* 5 6 Department of Fundamental Microbiology, University of Lausanne, CH-1015 7 Lausanne, Switzerland 8 9 Running title: Description of a bee gut symbiont 10 11 *Correspondence: 12 Prof. Philipp Engel 13 Department of Fundamental Microbiology 14 University of Lausanne, CH-1015 Lausanne, Switzerland 15 Tel.: +41 (0)21 692 56 12 16 e-mail: [email protected] 17 18 Category: New Taxa – Proteobacteria 19 Keywords: Apis mellifera; insect; Bartonella; gut microbiota; Alpha-1 20 21 Sequence deposition: The 16S rRNA gene sequences and protein-coding gene 22 sequences of the bacterial strains PEB0122T, PEB0149, PEB0150, BBC0104, and 23 BBC0108 from Apis mellifera, and the uncultured Rhizobiales bacterium from 24 Herpagnathos saltator are deposited in GenBank with accession numbers KP987849 25 – KP987886 and KT315729 – KT315734. -

Impact of HIV on Gastroenterology/Hepatology
Core Curriculum: Impact of HIV on Gastroenterology/Hepatology AshutoshAshutosh Barve,Barve, M.D.,M.D., Ph.D.Ph.D. Gastroenterology/HepatologyGastroenterology/Hepatology FellowFellow UniversityUniversityUniversity ofofof LouisvilleLouisville Louisville Case 4848 yearyear oldold manman presentspresents withwith aa historyhistory ofof :: dysphagiadysphagia odynophagiaodynophagia weightweight lossloss EGDEGD waswas donedone toto evaluateevaluate thethe problemproblem University of Louisville Case – EGD Report ExtensivelyExtensively scarredscarred esophagealesophageal mucosamucosa withwith mucosalmucosal bridging.bridging. DistalDistal esophagealesophageal nodulesnodules withwithUniversity superficialsuperficial ulcerationulceration of Louisville Case – Esophageal Nodule Biopsy InflammatoryInflammatory lesionlesion withwith ulceratedulcerated mucosamucosa SpecialSpecial stainsstains forfor fungifungi revealreveal nonnon-- septateseptate branchingbranching hyphaehyphae consistentconsistent withwith MUCORMUCOR University of Louisville Case TheThe patientpatient waswas HIVHIV positivepositive !!!! University of Louisville HAART (Highly Active Anti Retroviral Therapy) HIV/AIDS Before HAART After HAART University of Louisville HIV/AIDS BeforeBefore HAARTHAART AfterAfter HAARTHAART ImmuneImmune dysfunctiondysfunction ImmuneImmune reconstitutionreconstitution OpportunisticOpportunistic InfectionsInfections ManagementManagement ofof chronicchronic ¾ Prevention diseasesdiseases e.g.e.g. HepatitisHepatitis CC ¾ Management CirrhosisCirrhosis NeoplasmsNeoplasms -

Recognizing and Treating New and Emerging Infections Encountered in Everyday Practice
Recognizing and treating new and emerging infections encountered in everyday practice STEVEN M. GORDON, MD NFECTIOUS DISEASES, pre- MiikWirj:« Although infectious diseases were once considered a dicted earlier in this cen- diminishing threat, new pathogens are constantly challenging tury to be eliminated as a the health care system. This article reviews the clinical presen- public health problem, re- tation, diagnosis, and treatment of seven emerging infections I main the chief cause of death that primary care physicians are likely to encounter. worldwide and a significant cause of death and morbidity in i Parvovirus B19 attacks erythrocyte precursors; the United States.1 Challenging infection is usually benign and self-limiting but can cause the US public health system are aplastic crises in patients with chronic hemolytic disorders. several newly identified patho- Hemorrhagic colitis due to Escherichia coli 0157:H7 infection gens (eg, human immunodefi- can lead to the hemolytic-uremic syndrome, especially in chil- ciency virus [HIV], Escherichia dren; it also can cause thrombotic thrombocytopenia purpura. coli 0157:H7, hepatitis C) and a Chlamydia pneumoniae causes a mild pneumonia that resem- resurgence of old diseases pre- bles mycoplasmal pneumonia. Bacillary angiomatosis primar- sumed to be under control (eg, ily affects immunocompromised patients, especially those tuberculosis, syphilis). Further, infected with human immunodeficiency virus (HIV). At least multiple-drug resistance in two organisms can cause bacillary angiomatosis: Bartonella hense- strains of pneumococci, gono- lae and Bartonella quintana. Hantavirus pulmonary syndrome cocci, enterococci, staphylo- is spread by exposure to the droppings of infected rodents. cocci, salmonella, and mycobac- Contrary to previous thought, HIV continues to replicate teria undermines efforts to throughout the course of the illness and does not have a latency control the diseases they cause.2 phase. -

CHRONIC PAIN in CATS Recent Advances in Clinical Assessment
601_614_Monteiro_Chronic pain3.qxp_FAB 12/06/2019 14:59 Page 601 Journal of Feline Medicine and Surgery (2019) 21, 601–614 CLINICAL REVIEW CHRONIC PAIN IN CATS Recent advances in clinical assessment Beatriz P Monteiro and Paulo V Steagall Negative impacts of chronic pain Practical relevance: Chronic pain is a feline health and welfare issue. It has Domestic animals may now have a long life expectancy, given a negative impact on quality of life and advances in veterinary healthcare; as a consequence, there is an impairs the owner–cat bond. Chronic increased prevalence of chronic conditions associated with pain. pain can exist by itself or may be Chronic pain affects feline health and welfare. It has a negative impact associated with disease and/or injury, on quality of life (QoL) and impairs the owner–cat bond. including osteoarthritis (OA), cancer, and oral Nowadays, chronic pain assessment should be considered a funda- and periodontal disease, among others. mental part of feline practice. Clinical challenges: Chronic pain assessment Indeed, lack of knowledge on is a fundamental part of feline practice, but can be Chronic pain-related changes the subject and the use of appro- challenging due to differences in pain mechanisms in behavior are subtle and priate tools for pain recognition underlying different conditions, and the cat’s natural are some of the reasons why behavior. It relies mostly on owner-assessed likely to be suppressed analgesic administration is com- behavioral changes and time-consuming veterinary monly neglected in cats.1 consultations. Beyond OA – for which disease- in the clinical setting. In chronic pain, changes in specific clinical signs have been described – little behavior are subtle and slow, and is known regarding other feline conditions that may only be evident in the home produce chronic pain. -

Mixed Breed Cats
Mixed Breed Cats: What a Unique Breed! Your cat is special! She senses your moods, is curious about your day, and has purred her way into your heart. Chances are that you chose her because you like Mixed Breed Cats and you expected her to have certain traits that would fit your lifestyle, like: May meow to communicate with you Lively, with a friendly personality Agile, sturdy, and athletic However, no cat is perfect! You may have also noticed these characteristics: Can become overweight easily if not exercised regularly Scratches when bored May be mischievous if not given enough attention Is it all worth it? Of course! She is of a mixed background and can come is all sizes and colors. Her personality is just as varied as her looks, but she makes an excellent companion. Your Mixed Breed Cat's Health We know that because you care so much about your cat, you want to take great care of her. That is why we have summarized the health concerns we will be discussing with you over the life of your cat. By knowing about the health concerns common among cats, we can help you tailor an individual preventive health plan and hopefully prevent some predictable risks in your pet. Many diseases and health conditions are genetic, meaning they are related to your pet’s breed. The conditions we will describe here have a significant rate of incidence or a strong PET MEDICAL CENTER 501 E. FM 2410 ● Harker Heights, Texas 76548 (254) 690-6769 www.pet-medcenter.com impact upon this mixed breed particularly, according to a motivate cats with more food-based interests to romp and general consensus among feline genetic researchers and tumble. -
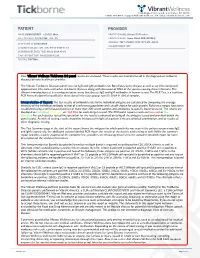
View Tickborne Diseases Sample Report
1360 Bayport Ave, Ste B. San Carlos, CA 94070 1(866) 364-0963 | [email protected] | www. vibrant-wellness.com PATIENT PROVIDER NAME: DEMO REPORT GENDER: Male PRACTICE NAME: Vibrant IT4 Practice DATE OF BIRTH: 04/14/1998 AGE: 22 PROVIDER NAME: Demo Client, DDD (999994) ADDRESS: TEST STREET, TEST CITY, KY- 42437. ACCESSION ID: 2009220006 PHLEBOTOMIST: 607 SPECIMEN COLLECTION TIME: 09-21-2020 11:14 SPECIMEN RECEIVED TIME: 09-22-2020 05:14 FINAL REPORT TIME: 09-25-2020 15:56 FASTING: FASTING Your Vibrant Wellness TickBorne 2.0 panel results are enclosed. These results are intended to aid in the diagnosis of tickborne diseases by your healthcare provider. The Vibrant Tickborne Diseases panel tests for IgG and IgM antibodies for Borreliosis/Lyme disease as well as co-infection(s) and opportunistic infections with other tick-borne illnesses along with detection of DNA of the species causing these infections. The Vibrant Immunochip test is a semiquantitative assay that detects IgG and IgM antibodies in human serum. The PCR Test is a real-time PCR Assay designed for qualitative detection of infectious group- specific DNA in clinical samples. Interpretation of Report: The test results of antibody levels to the individual antigens are calculated by comparing the average intensity of the individual antibody to that of a reference population and cut-off chosen for each protein. Reference ranges have been established using a well characterized set of more than 300 serum samples and antibodies to specific bacteria tested. The results are displayed as In Control, Moderate, or High Risk.for each antigen tested. -

Genetic Diversity of Bartonella Species in Small Mammals in the Qaidam
www.nature.com/scientificreports OPEN Genetic diversity of Bartonella species in small mammals in the Qaidam Basin, western China Huaxiang Rao1, Shoujiang Li3, Liang Lu4, Rong Wang3, Xiuping Song4, Kai Sun5, Yan Shi3, Dongmei Li4* & Juan Yu2* Investigation of the prevalence and diversity of Bartonella infections in small mammals in the Qaidam Basin, western China, could provide a scientifc basis for the control and prevention of Bartonella infections in humans. Accordingly, in this study, small mammals were captured using snap traps in Wulan County and Ge’ermu City, Qaidam Basin, China. Spleen and brain tissues were collected and cultured to isolate Bartonella strains. The suspected positive colonies were detected with polymerase chain reaction amplifcation and sequencing of gltA, ftsZ, RNA polymerase beta subunit (rpoB) and ribC genes. Among 101 small mammals, 39 were positive for Bartonella, with the infection rate of 38.61%. The infection rate in diferent tissues (spleens and brains) (χ2 = 0.112, P = 0.738) and gender (χ2 = 1.927, P = 0.165) of small mammals did not have statistical diference, but that in diferent habitats had statistical diference (χ2 = 10.361, P = 0.016). Through genetic evolution analysis, 40 Bartonella strains were identifed (two diferent Bartonella species were detected in one small mammal), including B. grahamii (30), B. jaculi (3), B. krasnovii (3) and Candidatus B. gerbillinarum (4), which showed rodent-specifc characteristics. B. grahamii was the dominant epidemic strain (accounted for 75.0%). Furthermore, phylogenetic analysis showed that B. grahamii in the Qaidam Basin, might be close to the strains isolated from Japan and China. -

Novel Small Rnas Expressed by Bartonella Bacilliformis Under Multiple Conditions 2 Reveal Potential Mechanisms for Persistence in the Sand Fly Vector and Human 3 Host
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.04.235903; this version posted August 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Novel small RNAs expressed by Bartonella bacilliformis under multiple conditions 2 reveal potential mechanisms for persistence in the sand fly vector and human 3 host 4 5 6 Shaun Wachter1, Linda D. Hicks1, Rahul Raghavan2 and Michael F. Minnick1* 7 8 9 10 1 Program in Cellular, Molecular & Microbial Biology, Division of Biological Sciences, 11 University of Montana, Missoula, Montana, United States of America 12 2 Department of Biology and Center for Life in Extreme Environments, Portland State 13 University, Portland, Oregon, United States of America 14 15 16 17 * Corresponding author 18 E-mail: [email protected] (MFM) 19 20 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.04.235903; this version posted August 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 21 Abstract 22 Bartonella bacilliformis, the etiological agent of Carrión’s disease, is a Gram-negative, 23 facultative intracellular alphaproteobacterium. Carrión’s disease is an emerging but neglected 24 tropical illness endemic to Peru, Colombia, and Ecuador. B. bacilliformis is spread between 25 humans through the bite of female phlebotomine sand flies. -

09 Piqueras.Qxp
PERSPECTIVES INTERNATIONAL MICROBIOLOGY (2007) 10:217-226 DOI: 10.2436/20.1501.01.30 ISSN: 1139-6709 www.im.microbios.org Microbiology: a dangerous profession? Mercè Piqueras President, Catalan Association for Science Communication (ACCC), Barcelona, Spain The history of science contains many cases of researchers eases in Minorca from the year 1744 to 1749 to which is pre- who have died because of their professional activity. In the fixed, a short account of the climate, productions, inhabi- field of microbiology, some have died or have come close to tants, and endemical distempers of that island (T. Cadell, D. death from infection by agents that were the subject of their Wilson and G. Nicol, London, 1751), which he dedicated to research (Table 1). Infections that had a lethal outcome were the Society of Surgeons of His Majesty’s Royal Navy. usually accidental. Sometimes, however, researchers inocu- Minorcan historian of science Josep M. Vidal Hernández has lated themselves with the pathogen or did not take preventive described and carefully analyzed Cleghorn’s work in measures against the potential pathogen because they wanted Minorca and his report [43]. According to Vidal, what to prove their hypotheses—or disprove someone else’s— Cleghorn describes is “tertian” fever, which was the name regarding the origin of the infection. Here is an overview of given at the time to fever caused by malaria parasites with a several episodes in the history of microbiology since the mid periodicity of 48 hours. In fact, Cleghorn used quinine to nineteenth century involving researchers or workers in fields treat tertian fever (i.e, malaria), which was not eradicated related to microbiology who have become infected. -

Bartonella Henselae • Fleas and Black-Legged Ticks (Also Called Deer Ticks) of the Genus Ixodes May Serve As Vectors, but This Has Not Disease Agent: Been Proven
APPENDIX 2 Bartonella henselae • Fleas and black-legged ticks (also called deer ticks) of the genus Ixodes may serve as vectors, but this has not Disease Agent: been proven. • Bartonella henselae Blood Phase: Disease Agent Characteristics: • Agent found in endothelial cells and associated with RBCs in symptomatic cases • Gram-negative bacillus or coccobacillus, aerobic, • Occult bacteremia sometimes occurs in the absence nonmotile, nonspore-forming, facultatively intracel- of specific antibodies. lular bacterium • Order: Rhizobiales; Family: Bartonellaceae Survival/Persistence in Blood Products: • Size: 0.3-0.6 ¥ 0.3-1.0 mm • Nucleic acid: Approximately 1900 kb of DNA • A spiking study suggests that B. henselae added to RBCs can be recovered on solid media through 35 Disease Name: days of storage at 4°C. • Cat scratch disease • Cat scratch fever Transmission by Blood Transfusion: • Bacillary angiomatosis • Theoretical • Bacillary peliosis Cases/Frequency in Population: Priority Level: • 22,000 cases per year estimated in the US • Scientific/Epidemiologic evidence regarding blood • 2-6% in US blood donors safety: Theoretical • Cumulative seroprevalence of 7.1% to B. henselae and • Public perception and/or regulatory concern regard- B. quintana in US veterinary professionals ing blood safety: Absent • Public concern regarding disease agent: Very low Incubation Period: Background: • 3-10 days to appearance of papule at inoculation site; regional adenopathy may follow after a few weeks • In 1909,ALBartondescribed organisms that adhered to RBCs. Likelihood of Clinical Disease: • The name Bartonella bacilliformis was used for the • Relatively benign and self-limiting, lasting 6-12 weeks only member of the group identified before 1993. in the absence of antibiotic therapy • Several other species of Bartonella are known to infect humans, but at present, B. -

Bacillary Angiomatosis with Bone Invasion*
CASE REPORT 811 s Bacillary angiomatosis with bone invasion* Lucia Martins Diniz1 Karina Bittencourt Medeiros1 Luana Gomes Landeiro1 Elton Almeida Lucas1 DOI: http://dx.doi.org/10.1590/abd1806-4841.20165436 Abstract: Bacillary angiomatosis is an infection determined by Bartonella henselae and B. quintana, rare and prevalent in pa- tients with acquired immunodeficiency syndrome. We describe a case of a patient with AIDS and TCD4+ cells equal to 9/mm3, showing reddish-violet papular and nodular lesions, disseminated over the skin, most on the back of the right hand and third finger, with osteolysis of the distal phalanx observed by radiography. The findings of vascular proliferation with presence of bacilli, on the histopathological examination of the skin and bone lesions, led to the diagnosis of bacillary angiomatosis. Corroborating the literature, in the present case the infection affected a young man (29 years old) with advanced immunosup- pression and clinical and histological lesions compatible with the diagnosis. Keywords: Acquired immunodeficiency syndrome; Angiomatosis, bacillary; Bartonella; Bartonella quintana INTRODUCTION Histology of the lesions of affected organs shows vascular Bacillary angiomatosis is an infection universally distrib- proliferation, hence the name “angiomatosis”. By silver staining, the uted, rare, caused by Gram-negative and facultative intracellular presence of the bacilli is revealed, thus “bacillary”.4 In histological bacilli of the Bartonella genus, which 18 species and subspecies are description, capillary proliferation is observed characteristically in currently known, and which also determine other diseases in man.1 lobes – central capillaries are more differentiated and peripheral The species responsible for bacillary angiomatosis are B. henselae capillaries are less mature – with lumens not so evident. -

Bartonella Henselae Detected in Malignant Melanoma, a Preliminary Study
pathogens Article Bartonella henselae Detected in Malignant Melanoma, a Preliminary Study Marna E. Ericson 1, Edward B. Breitschwerdt 2 , Paul Reicherter 3, Cole Maxwell 4, Ricardo G. Maggi 2, Richard G. Melvin 5 , Azar H. Maluki 4,6 , Julie M. Bradley 2, Jennifer C. Miller 7, Glenn E. Simmons, Jr. 5 , Jamie Dencklau 4, Keaton Joppru 5, Jack Peterson 4, Will Bae 4, Janet Scanlon 4 and Lynne T. Bemis 5,* 1 T Lab Inc., 910 Clopper Road, Suite 220S, Gaithersburg, MD 20878, USA; [email protected] 2 Intracellular Pathogens Research Laboratory, Comparative Medicine Institute, College of Veterinary Medicine, North Carolina State University, Raleigh, NC 27607, USA; [email protected] (E.B.B.); [email protected] (R.G.M.); [email protected] (J.M.B.) 3 Dermatology Clinic, Truman Medical Center, University of Missouri, Kansas City, MO 64108, USA; [email protected] 4 Department of Dermatology, University of Minnesota, Minneapolis, MN 55455, USA; [email protected] (C.M.); [email protected] (A.H.M.); [email protected] (J.D.); [email protected] (J.P.); [email protected] (W.B.); [email protected] (J.S.) 5 Department of Biomedical Sciences, Duluth Campus, Medical School, University of Minnesota, Duluth, MN 55812, USA; [email protected] (R.G.M.); [email protected] (G.E.S.J.); [email protected] (K.J.) 6 Department of Dermatology, College of Medicine, University of Kufa, Kufa 54003, Iraq 7 Galaxy Diagnostics Inc., Research Triangle Park, NC 27709, USA; [email protected] Citation: Ericson, M.E.; * Correspondence: [email protected]; Tel.: +1-720-560-0278; Fax: +1-218-726-7906 Breitschwerdt, E.B.; Reicherter, P.; Maxwell, C.; Maggi, R.G.; Melvin, Abstract: Bartonella bacilliformis (B.