Open Scheinberg Dissertation 2.8.15.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Get Consistent and Reliable Results
Need help selecting? M Microbiology Free Tech Support 800-323-4340 Cole-Parmer® Dehydrated Culture Media Get consistent and reliable results – Use when ready or dehydrated culture extends shelf life – Individually numbered with certificate of compliance expiration date, and shelf-life guarantee – Quick dissolve for faster processing – For laboratory use only Media, Dehydrated Media, Media Description Size (g) Catalog number Price Agar, bacteriological This clear gel agar is high grade and manufactured using the ice method 500 GH-14200-10 Azide dextrose broth Use for detection of fecal Streptococci in water and sewage 500 GH-14202-00 Baird parker agar Use for the selective isolation of coagulase positive Staphylococci in food 500 GH-14202-01 Blood agar base with low pH Use to cultivate a wide variety of bacteria 500 GH-14202-02 This is used as a differential medium in the isolation and presumptive identification of Bile Esculin agar 500 GH-14202-03 enterococci/group D streptococci Brain heart infusion agar Use to cultivate a wide spectrum of bacteria, yeasts, and molds 500 GH-14200-12 Brain heart infusion broth Use to cultivate fastidious aerobic and anaerobic bacteria 500 GH-14202-05 Brilliant green bile broth A standard methods medium for confirmed and completed tests for coliforms in water 500 GH-14200-14 Buffered peptone water Helps in the recovery of Salmonella from foods after preservation techniques 500 GH-14202-08 Cetrimide agar Use for the selective isolation of Pseudomonas aeruginosa 500 GH-14200-52 This broth is especially suited for environmental sampling where neutralization of the chemical D/E neutralizing Broth 500 GH-14202-11 is important to determining the bactericidal activity Use to isolate E. -

Nama from Listeria Monocytogenes
Identification and Characterisation of an Old Yellow Enzyme (OYE) - NamA from Listeria monocytogenes by Majid Abdullah Bamaga A thesis submitted in partial fulfilment of the requirements of Edinburgh Napier University, for the award of Doctor of Philosophy September, 2014 Abstract The food-borne pathogene Listeria monocytogenes has been considered a significant threat to human health worldwide. It mainly infects individuals suffering insuffecint immunity such as pregnant women. During pregnancy, L. monocytogenes is capable of causing a serious damage to the mother and the fetus. It can spread to different organs including the placenta via adaptation to interacellular lifestyle. To maintain pregnancy, the levels of the hormones progesterone and β-estradiol increase and reduction in hormone levels was proposed to be associated with fetal death and abortion. The objectives of this project therefore were to investigate the role of pregnancy hormones on the growth and virulence of L. monocytogenes, and to identify bacterial genes with possible roles in binding to pregnancy hormones. It was obsereved that the growth of L. monocytogenes in the presence of progesterone under anaerobic condition was affected by the action of the hormone and the effect was dose/time-dependent of exposure as increasing concentrations showed greater effect on the bacterial growth. Interestingly, bacterial growth was restored within 24 h of exposure to the hormone. In parallel, a Tn917-LTV3 insertion library was constructed and a number of mutants isolated that had reduced growth in the presence of β-estradiol were identified. However, reduction in growth was not microbiologically significant. Furthermore, bioinformatics analysis was performed to identify listerial genes with possible role in hormones degradation. -

Cross-Resistance to Phage Infection in Listeria Monocytogenes Serotype 1/2A Mutants and Preliminary Analysis of Their Wall Teichoic Acids
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Masters Theses Graduate School 8-2019 Cross-resistance to Phage Infection in Listeria monocytogenes Serotype 1/2a Mutants and Preliminary Analysis of their Wall Teichoic Acids Danielle Marie Trudelle University of Tennessee, [email protected] Follow this and additional works at: https://trace.tennessee.edu/utk_gradthes Recommended Citation Trudelle, Danielle Marie, "Cross-resistance to Phage Infection in Listeria monocytogenes Serotype 1/2a Mutants and Preliminary Analysis of their Wall Teichoic Acids. " Master's Thesis, University of Tennessee, 2019. https://trace.tennessee.edu/utk_gradthes/5512 This Thesis is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Masters Theses by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a thesis written by Danielle Marie Trudelle entitled "Cross-resistance to Phage Infection in Listeria monocytogenes Serotype 1/2a Mutants and Preliminary Analysis of their Wall Teichoic Acids." I have examined the final electronic copy of this thesis for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Master of Science, with a major in Food Science. Thomas G. Denes, Major Professor We have read this thesis and recommend its acceptance: -

Prepared Culture Media
PREPARED CULTURE MEDIA 121517SS PREPARED CULTURE MEDIA Made in the USA AnaeroGRO™ DuoPak A 02 Bovine Blood Agar, 5%, with Esculin 13 AnaeroGRO™ DuoPak B 02 Bovine Blood Agar, 5%, with Esculin/ AnaeroGRO™ BBE Agar 03 MacConkey Biplate 13 AnaeroGRO™ BBE/PEA 03 Bovine Selective Strep Agar 13 AnaeroGRO™ Brucella Agar 03 Brucella Agar with 5% Sheep Blood, Hemin, AnaeroGRO™ Campylobacter and Vitamin K 13 Selective Agar 03 Brucella Broth with 15% Glycerol 13 AnaeroGRO™ CCFA 03 Brucella with H and K/LKV Biplate 14 AnaeroGRO™ Egg Yolk Agar, Modified 03 Buffered Peptone Water 14 AnaeroGRO™ LKV Agar 03 Buffered Peptone Water with 1% AnaeroGRO™ PEA 03 Tween® 20 14 AnaeroGRO™ MultiPak A 04 Buffered NaCl Peptone EP, USP 14 AnaeroGRO™ MultiPak B 04 Butterfield’s Phosphate Buffer 14 AnaeroGRO™ Chopped Meat Broth 05 Campy Cefex Agar, Modified 14 AnaeroGRO™ Chopped Meat Campy CVA Agar 14 Carbohydrate Broth 05 Campy FDA Agar 14 AnaeroGRO™ Chopped Meat Campy, Blood Free, Karmali Agar 14 Glucose Broth 05 Cetrimide Select Agar, USP 14 AnaeroGRO™ Thioglycollate with Hemin and CET/MAC/VJ Triplate 14 Vitamin K (H and K), without Indicator 05 CGB Agar for Cryptococcus 14 Anaerobic PEA 08 Chocolate Agar 15 Baird-Parker Agar 08 Chocolate/Martin Lewis with Barney Miller Medium 08 Lincomycin Biplate 15 BBE Agar 08 CompactDry™ SL 16 BBE Agar/PEA Agar 08 CompactDry™ LS 16 BBE/LKV Biplate 09 CompactDry™ TC 17 BCSA 09 CompactDry™ EC 17 BCYE Agar 09 CompactDry™ YMR 17 BCYE Selective Agar with CAV 09 CompactDry™ ETB 17 BCYE Selective Agar with CCVC 09 CompactDry™ YM 17 BCYE -

View Our Full Water Sampling Vials Product Offering
TABLE OF CONTENTS Environmental Monitoring 1 Sample Prep and Dilution 8 Dehydrated Culture Media - Criterion™ 12 Prepared Culture Media 14 Chromogenic Media - HardyCHROM™ 18 CompactDry™ 20 Quality Control 24 Membrane Filtration 25 Rapid Tests 26 Lab Supplies/Sample Collection 27 Made in the USA Headquarters Distribution Centers 1430 West McCoy Lane Santa Maria, California Santa Maria, CA 93455 Olympia, Washington 800.266.2222 : phone Salt Lake City, Utah [email protected] Phoenix, Arizona HardyDiagnostics.com Dallas, Texas Springboro, Ohio Hardy Diagnostics has a Quality Lake City, Florida Management System that is certified Albany, New York to ISO 13485 and is a FDA licensed Copyright © 2020 Hardy Diagnostics Raleigh, North Carolina medical device manufacturer. Environmental Monitoring Hardy Diagnostics offers a wide selection of quality products intended to help keep you up to date with regulatory compliance, ensure the efficacy of your cleaning protocol, and properly monitor your environment. 800.266.2222 [email protected] HardyDiagnostics.com 1 Environmental Monitoring Air Sampling TRIO.BAS™ Impact Air Samplers introduced the newest generation of microbial air sampling. These ergonomically designed instruments combine precise air sampling with modern connectivity to help you properly assess the air quality of your laboratory and simplify your process. MONO DUO Each kit includes: Each kit includes: TRIO.BAS™ MONO air sampler, induction TRIO.BAS™ DUO air sampler, battery battery charger and cable, aspirating charger -

Listeria Monocytogenes Numa Queijaria
Estudo das vias de contaminação de Listeria monocytogenes numa queijaria PFGE, serotipagem, WGS e resistência a desinfetantes Mestrado em Inovação e Qualidade na Produção Alimentar Ana Rita Simões Ferraz Orientadores Cristina Maria Baptista Santos Pintado Carla Maria Heliodoro Maia Relatório de estágio apresentado à Escola Superior Agrária do Instituto Politécnico de Castelo Branco e ao Instituto Nacional de Saúde Doutor Ricardo Jorge para cumprimento dos requisitos necessários à obtenção do grau de Mestre em Inovação e Qualidade na Produção Alimentar, realizada sob a orientação científica da Doutora Cristina Maria Baptista Santos Pintado, Professora Adjunta da Escola Superior Agrária do Instituto Politécnico de Castelo Branco e da Mestre Carla Maria Heliodoro Maia Técnica Superior do Laboratório de Microbiologia, Departamento de Alimentação e Nutrição do Instituto Nacional de Saúde Doutor Ricardo Jorge, I.P.-Lisboa Junho 2017 II Composição do júri Presidente do júri Doutor, Celestino António Morais de Almeida, Professor Coordenador da Escola Superior Agrária de Castelo Branco Vogais Orientadores: Doutora, Cristina Maria Baptista Santos Pintado, Professora Adjunta da Escola Superior Agrária de Castelo Branco. Mestre, Carla Maria Heliodoro Maia, Técnica Superior no Instituto Nacional de Saúde Doutor Ricardo Jorge. Arguentes: Doutor, João Pedro Martins da Luz, Professor Coordenador da Escola Superior Agrária de Castelo Branco. Doutor, Manuel Vicente de Freitas Martins, Professor Coordenador da Escola Superior Agrária de Castelo Branco. III IV Dedicatória Eu, Ana Rita Simões Ferraz dedico o presente trabalho aos meus pais por todo o trabalho, dedicação, carinho e amor com que me educaram e fizeram de mim a pessoa que sou hoje. Em especial à minha mãe, por ser a enorme Mulher que é, que me faz crescer e lutar pelos meus sonhos. -

A Critical Review on Listeria Monocytogenes
International Journal of Innovations in Biological and Chemical Sciences, Volume 13, 2020, 95-103 A Critical Review on Listeria monocytogenes Vedavati Goudar and Nagalambika Prasad* *Department of Microbiology, Faculty of Life Science, School of Life Sciences, JSS Academy of Higher Education & Research, Mysuru, Karnataka, Pin code: 570015, India ABSTRACT Listeria monocytogenes is an omnipresent gram +ve, rod shaped, facultative, and motile bacteria. It is an opportunistic intracellular pathogenic microorganism that has become crucial reason for human food borne infections worldwide. It causes Listeriosis, the disease that can be serious and fatal to human and animals. Listeria outbreaks are often linked to dairy products, raw vegetables, raw meat and smoked fish, raw milk. The most effected country by Listeriosis is United States. CDC estimated that 1600 people get Listeriosis annually and regarding 260 die. It additionally contributes to negative economic impact because of the value of surveillance, investigation, treatment and prevention of sickness. The analysis of food products for presence of pathogenic microorganisms is one among the fundamental steps to regulate safety of food. This article intends to review the status of its introduction, characteristics, outbreaks, symptoms, prevention and treatment, more importantly to controlling the Listeriosis and its safety measures. Keywords: Listeria monocytogenes, Listeriosis, Food borne pathogens, Contamination INTRODUCTION Food borne health problem is outlined by the World Health Organization as “diseases, generally occurs by either infectious or hepatotoxic in nature, caused by the agents that enter the body through the activity of food WHO 2015 [1]. Causes of food borne health problem include bacteria, parasites, viruses, toxins, metals, and prions [2]. -

BD Industry Catalog
PRODUCT CATALOG INDUSTRIAL MICROBIOLOGY BD Diagnostics Diagnostic Systems Table of Contents Table of Contents 1. Dehydrated Culture Media and Ingredients 5. Stains & Reagents 1.1 Dehydrated Culture Media and Ingredients .................................................................3 5.1 Gram Stains (Kits) ......................................................................................................75 1.1.1 Dehydrated Culture Media ......................................................................................... 3 5.2 Stains and Indicators ..................................................................................................75 5 1.1.2 Additives ...................................................................................................................31 5.3. Reagents and Enzymes ..............................................................................................75 1.2 Media and Ingredients ...............................................................................................34 1 6. Identification and Quality Control Products 1.2.1 Enrichments and Enzymes .........................................................................................34 6.1 BBL™ Crystal™ Identification Systems ..........................................................................79 1.2.2 Meat Peptones and Media ........................................................................................35 6.2 BBL™ Dryslide™ ..........................................................................................................80 -

Listeria Sensu Stricto Specific Genes Involved in Colonization of the Gastrointestinal Tract by Listeria Monocytogenes
TECHNISCHE UNIVERSITÄT MÜNCHEN Lehrstuhl für Mikrobielle Ökologie Characterization of Listeria sensu stricto specific genes involved in colonization of the gastrointestinal tract by Listeria monocytogenes Jakob Johannes Schardt Vollständiger Abdruck der von der Fakultät Wissenschaftszentrum Weihenstephan für Ernährung, Landnutzung und Umwelt der Technischen Universität München zur Erlangung des akademischen Grades eines Doktors der Naturwissenschaften genehmigten Dissertation. Vorsitzender: Prof. Dr. rer.nat. Siegfried Scherer Prüfende der Dissertation: 1. apl.Prof. Dr.rer.nat. Thilo Fuchs 2. Prof. Dr.med Dietmar Zehn Die Dissertation wurde am 18.01.2018 bei der Technischen Universität München eingereicht und durch die Fakultät Wissenschaftszentrum Weihenstephan für Ernährung, Landnutzung und Umwelt am 14.05.2018 angenommen. Table of contents Table of contents ___________________________________________________________ I List of figures _______________________________________________________________ V List of tables ______________________________________________________________ VI List of abbreviations ________________________________________________________ VII Abstract __________________________________________________________________ IX Zusammenfassung __________________________________________________________ X 1 Introduction ______________________________________________________________ 1 1.1 The genus Listeria ____________________________________________________________ 1 1.1.1 Listeria sensu stricto ________________________________________________________________ -

150259-ID-None.Pdf
DIPONEGORO JOURNAL OF MAQUARES Volume 5, Nomor 3, Tahun 2016, Halaman: 157-164 MANAGEMENT OF AQUATIC RESOURCES http://ejournal-s1.undip.ac.id/index.php/maquares ANALISIS TOTAL BAKTERI COLIFORM DI PERAIRAN MUARA KALI WISO JEPARA The Analysis of Total Coliform Bacteria in Kali Wiso Estuary Jepara Wiwid Widyaningsih, Supriharyono *), Niniek Widyorini Program Studi Manajemen Sumberdaya Perairan Fakultas Perikanan dan Ilmu Kelautan, Universitas Diponegoro Jl. Prof. Soedarto, SH, Tembalang, Semarang, Jawa Tengah – 50275, Telp/Fax. +6224 7474698 Email : [email protected] ABSTRAK Kali Wiso merupakan sungai yang berada di tengah kota Jepara. Perairan ini menjadi tempat pembuangan limbah-limbah secara langsung. Limbah tersebut diantaranya limbah domestik, limbah pasar, limbah kapal, serta limbah TPI. Berdasarkan masukan limbah tersebut menjadikan muara ini tercemar. Perairan yang tercemar dapat dilihat dari pengamatan secara fisika, kimia, maupun biologis. Kondisi perairan yang tercemar secara biologis dilihat dari keberadaan bakteri patogen yang ada di perairan. Indikator bakteri yang digunakan yaitu bakteri coliform, karena sifatnya yang berkorelasi positif dengan bakteri patogen lainnya. Pemanfaatan perairan ini digunakan untuk kegiatan pelabuhan, tempat bersandar kapal nelayan, serta kegiatan perikanan yang ada di sekitar perairan Jepara. Oleh karena itu perlu diketahui kepadatan bakteri coliform sehingga dapat bermanfaat sesuai dengan peruntukannya. Tujuan dari penelitian ini adalah untuk mengetahui total bakteri coliform serta mengetahui adanya bakteri Escherichia coli. Penelitain ini dilakukan pada bulan Maret 2016 di Muara Kali Wiso dengan dua kali pengulangan dalam kondisi pasang dan surut. Metode yang digunakan yaitu survei dengan teknik sampling purposive sampling. Metode analisa laboratorium yang digunakan berdasarkan SNI -01-2332- 1991. Kepadatan bakteri coliform pada perairan muara Kali Wiso yaitu >110.000 sel/100ml dan bakteri Escherichia coli sebesar >110.000 sel/100ml. -
DONE Food and Beverage Testing
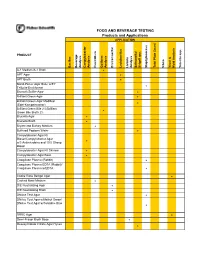
FOOD AND BEVERAGE TESTING Products and Applications APPLICATION PRODUCT Bacillus Beverage Analysis Campylobacter Analysis Clostridium Coliform Analysis Environmental Lactobacillus Listeria Analysis Salmonella/ Shigell spp. Staphylococcus Total Plate Count Vibrio Yeast & Mold Analysis Yersinia spp. A-1 Medium/A-1 Broth ! APT Agar ! APT Broth ! Baird-Parker Agar Base w/EY Tellurite Enrichment ! Bismuth Sulfite Agar ! Brilliant Green Agar ! Brilliant Green Agar Modified (Edel-Kampelmacher) ! Brilliant Green Bile 2%/Brilliant Green Bile Broth 2% ! Brucella Agar ! Brucella Broth ! Bryant and Burkey Medium ! Buffered Peptone Water ! Campylobacter Agar Kit Blaser/Campylobacter Agar w/5 Antimicrobics and 10% Sheep ! Blood Campylobacter Agar Kit Skirrow ! Campylobacter Agar Base ! Coagulase Plasma (Rabbit) ! Coagulase Plasma EDTA (Rabbit)/ Coagulase Plasma w/EDTA ! Cooke Rose Bengal Agar ! Cooked Meat Medium ! D/E Neutralizing Agar ! D/E Neutralizing Broth ! DNAse Test Agar ! DNAse Test Agar w/Methyl Green/ DNAse Test Agar w/Toluidine Blue ! DRBC Agar ! Demi-Fraser Broth Base ! Desoxycholate Citrate Agar Hynes ! FOOD AND BEVERAGE TESTING Products and Applications APPLICATION PRODUCT Bacillus Beverage Analysis Campylobacter Analysis Clostridium Coliform Analysis Environmental Lactobacillus Listeria Analysis Salmonella/ Shigell spp. Staphylococcus Total Plate Count Vibrio Yeast & Mold Analysis Yersinia spp. Differential Reinforced Clostridial Agar ! EC Medium/EC Broth ! EC Medium with MUG/EC Broth w/MUG ! Elliker Broth ! m Endo Agar LES ! m Endo -

Listeria Monocytogenes Soylarının Genetik Ve Virülens Farklılıkları
Vet Hekim Der Derg 89(1): 97-107,2018 Çağrılı Makale / Invited Paper Listeria monocytogenes soylarının genetik ve virülens farklılıkları Nurcay KOCAMAN*, Belgin SARIMEHMETOĞLU** Öz: Listeria monocytogenes insanlarda ve Giriş hayvanlarda septisemi, menenjit, meningoensefalit, L. monocytogenes, gıda kaynaklı hastalık düşük gibi ciddi invazif hastalıklara neden olabilen oluşturan etiyolojik bir ajandır (29, 39, 40, 49). Gıda gıda kaynaklı bir patojendir. Epidemiyolojik zincirinde yüksek tuz konsantrasyonu, ekstrem pH ve araştırmalarda, gıda işletmelerinden kontaminasyon sıcaklık gibi koşullarda hayatta kalabilme özelliğine kaynağının takibinde ve farklı türler arasındaki sahiptir (1, 15, 22, 27). ilişkinin evriminin belirlenmesinde L. monocytogenes Kısa çubuk görünümünde, tek veya kısa zincir türlerinin alt tiplendirmesi çok önemlidir. Bu şeklinde, 0,4 - 0,5 x 1-2 µm boyutlarında, paralel derlemede L. monocytogenes’in soyları ile soyları kenarlı ve küt uçlu, Gram pozitif bir bakteri olan L. arasındaki genetik ve virülens farklılıklarından monocytogenes; L. grayi, L. innocua, L. ivanovii, L. bahsedilmiştir. welshimeri ve L. seeligeri ile birlikte Bacilli sınıfı, Anahtar sözcükler: Epidemiyoloji, Listeria Bacillales takımı, Listeriaceae familyasında yer monocytogenes, soy, virülens almaktadır (30). Son zamanlarda, geleneksel fenotipik Genetic and virulence differences of Listeria metodlar ve genom dizilimi kullanılarak yapılan monocytogenes strains araştırmalarda, Listeria soyunun bilinen 6 türünden Abstract: Listeria monocytogenes is a foodborne