Exploring Virulence Factors and Alternative Therapies Against Staphylococcus Aureus Pneumonia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Predictive QSAR Tools to Aid in Early Process Development of Monoclonal Antibodies
Predictive QSAR tools to aid in early process development of monoclonal antibodies John Micael Andreas Karlberg Published work submitted to Newcastle University for the degree of Doctor of Philosophy in the School of Engineering November 2019 Abstract Monoclonal antibodies (mAbs) have become one of the fastest growing markets for diagnostic and therapeutic treatments over the last 30 years with a global sales revenue around $89 billion reported in 2017. A popular framework widely used in pharmaceutical industries for designing manufacturing processes for mAbs is Quality by Design (QbD) due to providing a structured and systematic approach in investigation and screening process parameters that might influence the product quality. However, due to the large number of product quality attributes (CQAs) and process parameters that exist in an mAb process platform, extensive investigation is needed to characterise their impact on the product quality which makes the process development costly and time consuming. There is thus an urgent need for methods and tools that can be used for early risk-based selection of critical product properties and process factors to reduce the number of potential factors that have to be investigated, thereby aiding in speeding up the process development and reduce costs. In this study, a framework for predictive model development based on Quantitative Structure- Activity Relationship (QSAR) modelling was developed to link structural features and properties of mAbs to Hydrophobic Interaction Chromatography (HIC) retention times and expressed mAb yield from HEK cells. Model development was based on a structured approach for incremental model refinement and evaluation that aided in increasing model performance until becoming acceptable in accordance to the OECD guidelines for QSAR models. -

Drug-Resistant Streptococcus Pneumoniae and Methicillin
NEWS & NOTES Conference Summary pneumoniae can vary among popula- conference sessions was that statically tions and is influenced by local pre- sound methods of data collection that Drug-resistant scribing practices and the prevalence capture valid, meaningful, and useful of resistant clones. Conference pre- data and meet the financial restric- Streptococcus senters discussed the role of surveil- tions of state budgets are indicated. pneumoniae and lance in raising awareness of the Active, population-based surveil- Methicillin- resistance problem and in monitoring lance for collecting relevant isolates is the effectiveness of prevention and considered the standard criterion. resistant control programs. National- and state- Unfortunately, this type of surveil- Staphylococcus level epidemiologists discussed the lance is labor-intensive and costly, aureus benefits of including state-level sur- making it an impractical choice for 1 veillance data with appropriate antibi- many states. The challenges of isolate Surveillance otic use programs designed to address collection, packaging and transport, The Centers for Disease Control the antibiotic prescribing practices of data collection, and analysis may and Prevention (CDC) convened a clinicians. The potential for local sur- place an unacceptable workload on conference on March 12–13, 2003, in veillance to provide information on laboratory and epidemiology person- Atlanta, Georgia, to discuss improv- the impact of a new pneumococcal nel. ing state-based surveillance of drug- vaccine for children was also exam- Epidemiologists from several state resistant Streptococcus pneumoniae ined; the vaccine has been shown to health departments that have elected (DRSP) and methicillin-resistant reduce infections caused by resistance to implement enhanced antimicrobial Staphylococcus aureus (MRSA). -
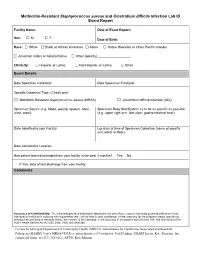
Methicillin-Resistant Staphylococcus Aureus and Clostridium Difficile Infection Lab ID Event Report
Methicillin-Resistant Staphylococcus aureus and Clostridium difficile Infection Lab ID Event Report Facility Name: Date of Event Report: Sex: M F □ □ Date of Birth: Race: □ White □ Black or African American □ Asian □ Native Hawaiian or Other Pacific Islander □ American Indian or Alaska Native □ Other [specify] __________________ Ethnicity: □ Hispanic or Latino □ Not Hispanic or Latino □ Other Event Details Date Specimen Collected: Date Specimen Finalized: Specific Organism Type: (Check one) □ Methicillin-Resistant Staphylococcus aureus (MRSA) □ Clostridium difficile Infection (CDI) Specimen Source (e.g. blood, wound, sputum, bone, Specimen Body Site/System try to be as specific as possible urine, stool): (e.g. upper right arm, foot ulcer, gastrointestinal tract): Date Admitted to your Facility: Location at time of Specimen Collection (name of specific unit, ward, or floor): Date Admitted to Location: Has patient been discharged from your facility in the past 3 months? Yes No If Yes, date of last discharge from your facility: Comments Assurance of Confidentiality: The voluntarily provided information obtained in this surveillance system that would permit identification of any individual or institution is collected with a guarantee that it will be held in strict confidence, will be used only for the purposes stated, and will not otherwise be disclosed or released without the consent of the individual, or the institution in accordance with Sections 304, 306 and 308(d) of the Public Health Service Act (42 USC 242b, 242k, and 242m(d)). For use by Michigan Department of Community Health (MDCH), Surveillance for Healthcare-Associated and Resistant Pathogens (SHARP) Unit’s MRSA/CDI Prevention Initiative (Coordinator: Gail Denkins, SHARP Intern: Kate Manton); fax completed forms to (517) 335-8263, ATTN: Kate Manton. -
Association Between Carriage of Streptococcus Pneumoniae and Staphylococcus Aureus in Children
BRIEF REPORT Association Between Carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children Gili Regev-Yochay, MD Context Widespread pneumococcal conjugate vaccination may bring about epidemio- Ron Dagan, MD logic changes in upper respiratory tract flora of children. Of particular significance may Meir Raz, MD be an interaction between Streptococcus pneumoniae and Staphylococcus aureus, in view of the recent emergence of community-acquired methicillin-resistant S aureus. Yehuda Carmeli, MD, MPH Objective To examine the prevalence and risk factors of carriage of S pneumoniae Bracha Shainberg, PhD and S aureus in the prevaccination era in young children. Estela Derazne, MSc Design, Setting, and Patients Cross-sectional surveillance study of nasopharyn- geal carriage of S pneumoniae and nasal carriage of S aureus by 790 children aged 40 Galia Rahav, MD months or younger seen at primary care clinics in central Israel during February 2002. Ethan Rubinstein, MD Main Outcome Measures Carriage rates of S pneumoniae (by serotype) and S aureus; risk factors associated with carriage of each pathogen. TREPTOCOCCUS PNEUMONIAE AND Results Among 790 children screened, 43% carried S pneumoniae and 10% car- Staphylococcus aureus are com- ried S aureus. Staphylococcus aureus carriage among S pneumoniae carriers was 6.5% mon inhabitants of the upper vs 12.9% in S pneumoniae noncarriers. Streptococcus pneumoniae carriage among respiratory tract in children and S aureus carriers was 27.5% vs 44.8% in S aureus noncarriers. Only 2.8% carried both Sare responsible for common infec- pathogens concomitantly vs 4.3% expected dual carriage (P=.03). Risk factors for tions. Carriage of S aureus and S pneu- S pneumoniae carriage (attending day care, having young siblings, and age older than moniae can result in bacterial spread and 3 months) were negatively associated with S aureus carriage. -

Turning on Virulence: Mechanisms That Underpin the Morphologic Transition and Pathogenicity of Blastomyces
Virulence ISSN: 2150-5594 (Print) 2150-5608 (Online) Journal homepage: http://www.tandfonline.com/loi/kvir20 Turning on Virulence: Mechanisms that underpin the Morphologic Transition and Pathogenicity of Blastomyces Joseph A. McBride, Gregory M. Gauthier & Bruce S. Klein To cite this article: Joseph A. McBride, Gregory M. Gauthier & Bruce S. Klein (2018): Turning on Virulence: Mechanisms that underpin the Morphologic Transition and Pathogenicity of Blastomyces, Virulence, DOI: 10.1080/21505594.2018.1449506 To link to this article: https://doi.org/10.1080/21505594.2018.1449506 © 2018 The Author(s). Published by Informa UK Limited, trading as Taylor & Francis Group© Joseph A. McBride, Gregory M. Gauthier and Bruce S. Klein Accepted author version posted online: 13 Mar 2018. Submit your article to this journal Article views: 15 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=kvir20 Publisher: Taylor & Francis Journal: Virulence DOI: https://doi.org/10.1080/21505594.2018.1449506 Turning on Virulence: Mechanisms that underpin the Morphologic Transition and Pathogenicity of Blastomyces Joseph A. McBride, MDa,b,d, Gregory M. Gauthier, MDa,d, and Bruce S. Klein, MDa,b,c a Division of Infectious Disease, Department of Medicine, University of Wisconsin School of Medicine and Public Health, 600 Highland Avenue, Madison, WI 53792, USA; b Division of Infectious Disease, Department of Pediatrics, University of Wisconsin School of Medicine and Public Health, 1675 Highland Avenue, Madison, WI 53792, USA; c Department of Medical Microbiology and Immunology, University of Wisconsin School of Medicine and Public Health, 1550 Linden Drive, Madison, WI 53706, USA. -
Clostridium Difficile Infection: How to Deal with the Problem DH INFORMATION RE ADER B OX
Clostridium difficile infection: How to deal with the problem DH INFORMATION RE ADER B OX Policy Estates HR / Workforce Commissioning Management IM & T Planning / Finance Clinical Social Care / Partnership Working Document Purpose Best Practice Guidance Gateway Reference 9833 Title Clostridium difficile infection: How to deal with the problem Author DH and HPA Publication Date December 2008 Target Audience PCT CEs, NHS Trust CEs, SHA CEs, Care Trust CEs, Medical Directors, Directors of PH, Directors of Nursing, PCT PEC Chairs, NHS Trust Board Chairs, Special HA CEs, Directors of Infection Prevention and Control, Infection Control Teams, Health Protection Units, Chief Pharmacists Circulation List Description This guidance outlines newer evidence and approaches to delivering good infection control and environmental hygiene. It updates the 1994 guidance and takes into account a national framework for clinical governance which did not exist in 1994. Cross Ref N/A Superseded Docs Clostridium difficile Infection Prevention and Management (1994) Action Required CEs to consider with DIPCs and other colleagues Timing N/A Contact Details Healthcare Associated Infection and Antimicrobial Resistance Department of Health Room 528, Wellington House 133-155 Waterloo Road London SE1 8UG For Recipient's Use Front cover image: Clostridium difficile attached to intestinal cells. Reproduced courtesy of Dr Jan Hobot, Cardiff University School of Medicine. Clostridium difficile infection: How to deal with the problem Contents Foreword 1 Scope and purpose 2 Introduction 3 Why did CDI increase? 4 Approach to compiling the guidance 6 What is new in this guidance? 7 Core Guidance Key recommendations 9 Grading of recommendations 11 Summary of healthcare recommendations 12 1. -
Evaluating Alternative Hypotheses to Explain the Downward Trend in the Indices of the COVID-19 Pandemic Death Rate
Evaluating alternative hypotheses to explain the downward trend in the indices of the COVID-19 pandemic death rate Sonali Shinde1, Pratima Ranade1 and Milind Watve2 1 Department of Biodiversity, Abasaheb Garware College, Pune, Pune, Maharashtra, India 2 Independent Researcher, Pune, Maharashtra, India ABSTRACT Background: In the ongoing Covid-19 pandemic, in the global data on the case fatality ratio (CFR) and other indices reflecting death rate, there is a consistent downward trend from mid-April to mid-November. The downward trend can be an illusion caused by biases and limitations of data or it could faithfully reflect a declining death rate. A variety of explanations for this trend are possible, but a systematic analysis of the testable predictions of the alternative hypotheses has not yet been attempted. Methodology: We state six testable alternative hypotheses, analyze their testable predictions using public domain data and evaluate their relative contributions to the downward trend. Results: We show that a decline in the death rate is real; changing age structure of the infected population and evolution of the virus towards reduced virulence are the most supported hypotheses and together contribute to major part of the trend. The testable predictions from other explanations including altered testing efficiency, time lag, improved treatment protocols and herd immunity are not consistently supported, or do not appear to make a major contribution to this trend although they may influence some other patterns of the epidemic. Conclusion: The fatality of the infection showed a robust declining time trend between mid April to mid November. Changing age class of the infected and Submitted 7 December 2020 Accepted 3 March 2021 decreasing virulence of the pathogen were found to be the strongest contributors to Published 20 April 2021 the trend. -

Metabolic Sensor Governing Bacterial Virulence in Staphylococcus Aureus
Metabolic sensor governing bacterial virulence in PNAS PLUS Staphylococcus aureus Yue Dinga, Xing Liub, Feifei Chena, Hongxia Dia, Bin Xua, Lu Zhouc, Xin Dengd,e, Min Wuf, Cai-Guang Yangb,1, and Lefu Lana,1 aDepartment of Molecular Pharmacology and bChinese Academy of Sciences Key Laboratory of Receptor Research, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Shanghai 201203, China; cDepartment of Medicinal Chemistry, School of Pharmacy, Fudan University, Shanghai 201203, China; dDepartment of Chemistry and eInstitute for Biophysical Dynamics, The University of Chicago, Chicago, IL 60637; and fDepartment of Basic Sciences University of North Dakota School of Medicine and Health Sciences, Grand Forks, ND 58203 Edited by Richard P. Novick, New York University School of Medicine, New York, NY, and approved October 14, 2014 (received for review June 13, 2014) An effective metabolism is essential to all living organisms, in- To survive and replicate efficiently in the host, S. aureus has cluding the important human pathogen Staphylococcus aureus.To developed exquisite mechanisms for scavenging nutrients and establish successful infection, S. aureus must scavenge nutrients adjusting its metabolism to maintain growth while also coping with and coordinate its metabolism for proliferation. Meanwhile, it also stress (6, 11). On the other hand, S. aureus produces a wide array must produce an array of virulence factors to interfere with host of virulence factors to evade host immune defenses and to derive defenses. However, the ways in which S. aureus ties its metabolic nutrition either parasitically or destructively from the host during state to its virulence regulation remain largely unknown. Here we infections (6). -

Studies of Staphylococcal Infections. I. Virulence of Staphy- Lococci and Characteristics of Infections in Embryonated Eggs * WILLIAM R
Journal of Clinical Investigation Vol. 43, No. 11, 1964 Studies of Staphylococcal Infections. I. Virulence of Staphy- lococci and Characteristics of Infections in Embryonated Eggs * WILLIAM R. MCCABE t (From the Research Laboratory, West Side Veterans Administration Hospital, and the Department of Medicine, Research and Educational Hospitals, University of Illinois College of Medicine, Chicago, Ill.) Many of the determinants of the pathogenesis niques still require relatively large numbers of and course of staphylococcal infections remain staphylococci to produce infection (19). Fatal imprecisely defined (1, 2) despite their increas- systemic infections have been equally difficult to ing importance (3-10). Experimental infections produce in animals and have necessitated the in- in suitable laboratory animals have been of con- jection of 107 to 109 bacteria (20-23). A few siderable assistance in clarifying the role of host strains of staphylococci have been found that are defense mechanisms and specific bacterial virulence capable of producing lethal systemic infections factors with a variety of other infectious agents. with inocula of from 102 to 103 bacteria (24) and A sensitive experimental model would be of value have excited considerable interest (25-27). The in defining the importance of these factors in virulence of these strains apparently results from staphylococcal infections, but both humans and an unusual antigenic variation (27, 28) which, the usual laboratory animals are relatively re- despite its interest, is of doubtful significance in sistant. Extremely large numbers of staphylo- human staphylococcal infection, since such strains cocci are required to produce either local or sys- have been isolated only rarely from clinical in- temic infections experimentally. -

Virulence During Newcastle Disease Viruses Cross Species Adaptation
viruses Review Virulence during Newcastle Disease Viruses Cross Species Adaptation Claudio L. Afonso Base2bio, LLC, Oshkosh, WI 54905, USA; [email protected]; Tel.: +1-800-817-7160 Abstract: The hypothesis that host adaptation in virulent Newcastle disease viruses (NDV) has been accompanied by virulence modulation is reviewed here. Historical records, experimental data, and phylogenetic analyses from available GenBank sequences suggest that currently circulating NDVs emerged in the 1920–19400s from low virulence viruses by mutation at the fusion protein cleavage site. These viruses later gave rise to multiple virulent genotypes by modulating virulence in opposite directions. Phylogenetic and pathotyping studies demonstrate that older virulent NDVs further evolved into chicken-adapted genotypes by increasing virulence (velogenic-viscerotropic pathotypes with intracerebral pathogenicity indexes [ICPIs] of 1.6 to 2), or into cormorant-adapted NDVs by moderating virulence (velogenic–neurotropic pathotypes with ICPIs of 1.4 to 1.6), or into pigeon-adapted viruses by further attenuating virulence (mesogenic pathotypes with ICPIs of 0.9 to 1.4). Pathogenesis and transmission experiments on adult chickens demonstrate that chicken-adapted velogenic-viscerotropic viruses are more capable of causing disease than older velogenic-neurotropic viruses. Currently circulating velogenic–viscerotropic viruses are also more capable of replicating and of being transmitted in naïve chickens than viruses from cormorants and pigeons. These evolutionary virulence changes are consistent with theories that predict that virulence may evolve in many directions in order to achieve maximum fitness, as determined by genetic and ecologic constraints. Keywords: NDV; evolution; virulence; host adaptation Citation: Afonso, C.L. Virulence during Newcastle Disease Viruses Cross Species Adaptation. -

Methicillin-Resistant Staphylococcus Aureus (MRSA)
Methicillin-Resistant Staphylococcus Aureus (MRSA) Over the past several decades, the incidence of resistant gram-positive organisms has risen in the United States. MRSA strains, first identified in the 1960s in England, were first observed in the U.S. in the mid 1980s.1 Resistance quickly developed, increasing from 2.4% in 1979 to 29% in 1991.2 The current prevalence for MRSA in hospitals and other facilities ranges from <10% to 65%. In 1999, MRSA accounted for more than 50% of all Staphylococcus aureus isolates within U.S. intensive care units.3, 4 The past years, however, outbreaks of MRSA have also been seen in the community setting, particularly among preschool-age children, some of whom have attended day-care centers.5, 6, 7 MRSA does not appear to be more virulent than methicillin-sensitive Staphylococcus aureus, but certainly poses a greater treatment challenge. MRSA also has been associated with higher hospital costs and mortality.8 Within a decade of its development, methicillin resistance to Staphylococcus aureus emerged.9 MRSA strains generally are now resistant to other antimicrobial classes including aminoglycosides, beta-lactams, carbapenems, cephalosporins, fluoroquinolones and macrolides.10,11 Most of the resistance was secondary to production of beta-lactamase enzymes or intrinsic resistance with alterations in penicillin-binding proteins. Staphylococcus aureus is the most frequent cause of nosocomial pneumonia and surgical- wound infections and the second most common cause of nosocomial bloodstream infections.12 Long-term care facilities (LTCFs) have developed rates of MRSA ranging from 25%-35%. MRSA rates may be higher in LTCFs if they are associated with hospitals that have higher rates.13 Transmission of MRSA generally occurs through direct or indirect contact with a reservoir. -

Virulence of Japanese Encephalitis Virus Genotypes I and III, Taiwan
Virulence of Japanese Encephalitis Virus Genotypes I and III, Taiwan Yi-Chin Fan,1 Jen-Wei Lin,1 Shu-Ying Liao, within a year (8,9), which provided an excellent opportu- Jo-Mei Chen, Yi-Ying Chen, Hsien-Chung Chiu, nity to study the transmission dynamics and pathogenicity Chen-Chang Shih, Chi-Ming Chen, of these 2 JEV genotypes. Ruey-Yi Chang, Chwan-Chuen King, A mouse model showed that the pathogenic potential Wei-June Chen, Yi-Ting Ko, Chao-Chin Chang, is similar among different JEV genotypes (10). However, Shyan-Song Chiou the pathogenic difference between GI and GIII virus infec- tions among humans remains unclear. Endy et al. report- The virulence of genotype I (GI) Japanese encephalitis vi- ed that the proportion of asymptomatic infected persons rus (JEV) is under debate. We investigated differences in among total infected persons (asymptomatic ratio) is an the virulence of GI and GIII JEV by calculating asymptomat- excellent indicator for estimating virulence or pathogenic- ic ratios based on serologic studies during GI- and GIII-JEV endemic periods. The results suggested equal virulence of ity of dengue virus infections among humans (11). We used GI and GIII JEV among humans. the asymptomatic ratio method for a study to determine if GI JEV is associated with lower virulence than GIII JEV among humans in Taiwan. apanese encephalitis virus (JEV), a mosquitoborne Jflavivirus, causes Japanese encephalitis (JE). This virus The Study has been reported in Southeast Asia and Western Pacific re- JEVs were identified in 6 locations in Taiwan during 1994– gions since it emerged during the 1870s in Japan (1).