Methicillin-Resistant Staphylococcus Aureus (MRSA)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio In
microorganisms Review The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel disease Spase Stojanov 1,2, Aleš Berlec 1,2 and Borut Štrukelj 1,2,* 1 Faculty of Pharmacy, University of Ljubljana, SI-1000 Ljubljana, Slovenia; [email protected] (S.S.); [email protected] (A.B.) 2 Department of Biotechnology, Jožef Stefan Institute, SI-1000 Ljubljana, Slovenia * Correspondence: borut.strukelj@ffa.uni-lj.si Received: 16 September 2020; Accepted: 31 October 2020; Published: 1 November 2020 Abstract: The two most important bacterial phyla in the gastrointestinal tract, Firmicutes and Bacteroidetes, have gained much attention in recent years. The Firmicutes/Bacteroidetes (F/B) ratio is widely accepted to have an important influence in maintaining normal intestinal homeostasis. Increased or decreased F/B ratio is regarded as dysbiosis, whereby the former is usually observed with obesity, and the latter with inflammatory bowel disease (IBD). Probiotics as live microorganisms can confer health benefits to the host when administered in adequate amounts. There is considerable evidence of their nutritional and immunosuppressive properties including reports that elucidate the association of probiotics with the F/B ratio, obesity, and IBD. Orally administered probiotics can contribute to the restoration of dysbiotic microbiota and to the prevention of obesity or IBD. However, as the effects of different probiotics on the F/B ratio differ, selecting the appropriate species or mixture is crucial. The most commonly tested probiotics for modifying the F/B ratio and treating obesity and IBD are from the genus Lactobacillus. In this paper, we review the effects of probiotics on the F/B ratio that lead to weight loss or immunosuppression. -

Probiotic Properties of Enterococcus Faecium CE5-1 Producing A
Czech J. Anim. Sci., 57, 2012 (11): 529–539 Original Paper Probiotic properties of Enterococcus faecium CE5-1 producing a bacteriocin-like substance and its antagonistic effect against antibiotic-resistant enterococci in vitro K. Saelim1, N. Sohsomboon1, S. Kaewsuwan2, S. Maneerat1 1Department of Industrial Biotechnology, Faculty of Agro-Industry, Prince of Songkla University, Hat Yai, Thailand 2Department of Pharmacognosy and Pharmaceutical Botany, Faculty of Pharmaceutical Sciences, Prince of Songkla University, Hat Yai, Thailand ABSTRACT: A bacteriocin-like substance (BLS) producing Enterococcus faecium CE5-1 was isolated from the gastrointestinal tract (GIT) of Thai indigenous chickens. Investigations of its probiotic potential were carried out. The competition between the BLS probiotic strain and antibiotic-resistant enterococci was also studied. Ent. faecium CE5-1 exhibited a good tolerance to pH 3.0 after 2 h and in 7% fresh chicken bile after 6 h, but the viability of Ent. faecium CE5-1 decreased by about 2–3 log CFU/ml after 2 h incubation in pH 2.5. It was susceptible to the antibiotics tested (tetracycline, erythromycin, penicillin G, and vancomycin). The maximum BLS production from Ent. faecium CE5-1 was observed at 15 h of cultivation. It showed activity against Listeria monocytogenes DMST17303, Pediococcus pentosaceus 3CE27, Lactobacillus sakei subsp. sakei JCM1157, and antibiotic-resistant enterococci. The detection by polymerase chain reaction (PCR) in the enterocin structural gene determined the presence of enterocin A gene in Ent. faecium CE5-1 only. Ent. faecium CE5-1 showed the highest inhibitory activity against two antibiotic-resistant Ent. faecalis VanB (from 6.68 to 4.29 log CFU/ml) and Ent. -

Drug-Resistant Streptococcus Pneumoniae and Methicillin
NEWS & NOTES Conference Summary pneumoniae can vary among popula- conference sessions was that statically tions and is influenced by local pre- sound methods of data collection that Drug-resistant scribing practices and the prevalence capture valid, meaningful, and useful of resistant clones. Conference pre- data and meet the financial restric- Streptococcus senters discussed the role of surveil- tions of state budgets are indicated. pneumoniae and lance in raising awareness of the Active, population-based surveil- Methicillin- resistance problem and in monitoring lance for collecting relevant isolates is the effectiveness of prevention and considered the standard criterion. resistant control programs. National- and state- Unfortunately, this type of surveil- Staphylococcus level epidemiologists discussed the lance is labor-intensive and costly, aureus benefits of including state-level sur- making it an impractical choice for 1 veillance data with appropriate antibi- many states. The challenges of isolate Surveillance otic use programs designed to address collection, packaging and transport, The Centers for Disease Control the antibiotic prescribing practices of data collection, and analysis may and Prevention (CDC) convened a clinicians. The potential for local sur- place an unacceptable workload on conference on March 12–13, 2003, in veillance to provide information on laboratory and epidemiology person- Atlanta, Georgia, to discuss improv- the impact of a new pneumococcal nel. ing state-based surveillance of drug- vaccine for children was also exam- Epidemiologists from several state resistant Streptococcus pneumoniae ined; the vaccine has been shown to health departments that have elected (DRSP) and methicillin-resistant reduce infections caused by resistance to implement enhanced antimicrobial Staphylococcus aureus (MRSA). -

Detection of ESKAPE Pathogens and Clostridioides Difficile in Simulated
bioRxiv preprint doi: https://doi.org/10.1101/2021.03.04.433847; this version posted March 4, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Detection of ESKAPE pathogens and Clostridioides difficile in 2 Simulated Skin Transmission Events with Metagenomic and 3 Metatranscriptomic Sequencing 4 5 Krista L. Ternusa#, Nicolette C. Keplingera, Anthony D. Kappella, Gene D. Godboldb, Veena 6 Palsikara, Carlos A. Acevedoa, Katharina L. Webera, Danielle S. LeSassiera, Kathleen Q. 7 Schultea, Nicole M. Westfalla, and F. Curtis Hewitta 8 9 aSignature Science, LLC, 8329 North Mopac Expressway, Austin, Texas, USA 10 bSignature Science, LLC, 1670 Discovery Drive, Charlottesville, VA, USA 11 12 #Address correspondence to Krista L. Ternus, [email protected] 13 14 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.03.04.433847; this version posted March 4, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 15 1 Abstract 16 Background: Antimicrobial resistance is a significant global threat, posing major public health 17 risks and economic costs to healthcare systems. Bacterial cultures are typically used to diagnose 18 healthcare-acquired infections (HAI); however, culture-dependent methods provide limited 19 presence/absence information and are not applicable to all pathogens. -

Current Trends of Enterococci in Dairy Products: a Comprehensive Review of Their Multiple Roles
foods Review Current Trends of Enterococci in Dairy Products: A Comprehensive Review of Their Multiple Roles Maria de Lurdes Enes Dapkevicius 1,2,* , Bruna Sgardioli 1,2 , Sandra P. A. Câmara 1,2, Patrícia Poeta 3,4 and Francisco Xavier Malcata 5,6,* 1 Faculty of Agricultural and Environmental Sciences, University of the Azores, 9700-042 Angra do Heroísmo, Portugal; [email protected] (B.S.); [email protected] (S.P.A.C.) 2 Institute of Agricultural and Environmental Research and Technology (IITAA), University of the Azores, 9700-042 Angra do Heroísmo, Portugal 3 Microbiology and Antibiotic Resistance Team (MicroART), Department of Veterinary Sciences, University of Trás-os-Montes and Alto Douro (UTAD), 5001-801 Vila Real, Portugal; [email protected] 4 Associated Laboratory for Green Chemistry (LAQV-REQUIMTE), University NOVA of Lisboa, 2829-516 Lisboa, Portugal 5 LEPABE—Laboratory for Process Engineering, Environment, Biotechnology and Energy, Faculty of Engineering, University of Porto, 420-465 Porto, Portugal 6 FEUP—Faculty of Engineering, University of Porto, 4200-465 Porto, Portugal * Correspondence: [email protected] (M.d.L.E.D.); [email protected] (F.X.M.) Abstract: As a genus that has evolved for resistance against adverse environmental factors and that readily exchanges genetic elements, enterococci are well adapted to the cheese environment and may reach high numbers in artisanal cheeses. Their metabolites impact cheese flavor, texture, Citation: Dapkevicius, M.d.L.E.; and rheological properties, thus contributing to the development of its typical sensorial properties. Sgardioli, B.; Câmara, S.P.A.; Poeta, P.; Due to their antimicrobial activity, enterococci modulate the cheese microbiota, stimulate autoly- Malcata, F.X. -
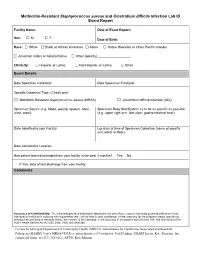
Methicillin-Resistant Staphylococcus Aureus and Clostridium Difficile Infection Lab ID Event Report
Methicillin-Resistant Staphylococcus aureus and Clostridium difficile Infection Lab ID Event Report Facility Name: Date of Event Report: Sex: M F □ □ Date of Birth: Race: □ White □ Black or African American □ Asian □ Native Hawaiian or Other Pacific Islander □ American Indian or Alaska Native □ Other [specify] __________________ Ethnicity: □ Hispanic or Latino □ Not Hispanic or Latino □ Other Event Details Date Specimen Collected: Date Specimen Finalized: Specific Organism Type: (Check one) □ Methicillin-Resistant Staphylococcus aureus (MRSA) □ Clostridium difficile Infection (CDI) Specimen Source (e.g. blood, wound, sputum, bone, Specimen Body Site/System try to be as specific as possible urine, stool): (e.g. upper right arm, foot ulcer, gastrointestinal tract): Date Admitted to your Facility: Location at time of Specimen Collection (name of specific unit, ward, or floor): Date Admitted to Location: Has patient been discharged from your facility in the past 3 months? Yes No If Yes, date of last discharge from your facility: Comments Assurance of Confidentiality: The voluntarily provided information obtained in this surveillance system that would permit identification of any individual or institution is collected with a guarantee that it will be held in strict confidence, will be used only for the purposes stated, and will not otherwise be disclosed or released without the consent of the individual, or the institution in accordance with Sections 304, 306 and 308(d) of the Public Health Service Act (42 USC 242b, 242k, and 242m(d)). For use by Michigan Department of Community Health (MDCH), Surveillance for Healthcare-Associated and Resistant Pathogens (SHARP) Unit’s MRSA/CDI Prevention Initiative (Coordinator: Gail Denkins, SHARP Intern: Kate Manton); fax completed forms to (517) 335-8263, ATTN: Kate Manton. -

Methicillin-Resistant Staphylococcus Aureus Infections in County Jails
Prevention, Treatment, and Containment of Methicillin-Resistant Staphylococcus aureus Infections in County Jails Texas Department of State Health Services and Correctional Facilities Workgroup September 2006 2 Clinical guidelines are being made available to the public for informational purposes only. Texas Department of State Health Services (DSHS) does not warrant these guidelines for any other purpose and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient-specific. 3 We acknowledge the Federal Bureau of Prisons Clinical Practice Guidelines for the Management Of Methicillin-Resistant Staphylococcus Aureus (MRSA) Infections, August 2005 for general organization and content of this document. 4 Table of Contents Introduction ......................................................................................................................... 6 Colonization ......................................................................................................................... 6 Transmission........................................................................................................................ 7 Screening and Surveillance ................................................................................................ 7 Diagnosis .............................................................................................................................. 8 -
Association Between Carriage of Streptococcus Pneumoniae and Staphylococcus Aureus in Children
BRIEF REPORT Association Between Carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children Gili Regev-Yochay, MD Context Widespread pneumococcal conjugate vaccination may bring about epidemio- Ron Dagan, MD logic changes in upper respiratory tract flora of children. Of particular significance may Meir Raz, MD be an interaction between Streptococcus pneumoniae and Staphylococcus aureus, in view of the recent emergence of community-acquired methicillin-resistant S aureus. Yehuda Carmeli, MD, MPH Objective To examine the prevalence and risk factors of carriage of S pneumoniae Bracha Shainberg, PhD and S aureus in the prevaccination era in young children. Estela Derazne, MSc Design, Setting, and Patients Cross-sectional surveillance study of nasopharyn- geal carriage of S pneumoniae and nasal carriage of S aureus by 790 children aged 40 Galia Rahav, MD months or younger seen at primary care clinics in central Israel during February 2002. Ethan Rubinstein, MD Main Outcome Measures Carriage rates of S pneumoniae (by serotype) and S aureus; risk factors associated with carriage of each pathogen. TREPTOCOCCUS PNEUMONIAE AND Results Among 790 children screened, 43% carried S pneumoniae and 10% car- Staphylococcus aureus are com- ried S aureus. Staphylococcus aureus carriage among S pneumoniae carriers was 6.5% mon inhabitants of the upper vs 12.9% in S pneumoniae noncarriers. Streptococcus pneumoniae carriage among respiratory tract in children and S aureus carriers was 27.5% vs 44.8% in S aureus noncarriers. Only 2.8% carried both Sare responsible for common infec- pathogens concomitantly vs 4.3% expected dual carriage (P=.03). Risk factors for tions. Carriage of S aureus and S pneu- S pneumoniae carriage (attending day care, having young siblings, and age older than moniae can result in bacterial spread and 3 months) were negatively associated with S aureus carriage. -
Clostridium Difficile Infection: How to Deal with the Problem DH INFORMATION RE ADER B OX
Clostridium difficile infection: How to deal with the problem DH INFORMATION RE ADER B OX Policy Estates HR / Workforce Commissioning Management IM & T Planning / Finance Clinical Social Care / Partnership Working Document Purpose Best Practice Guidance Gateway Reference 9833 Title Clostridium difficile infection: How to deal with the problem Author DH and HPA Publication Date December 2008 Target Audience PCT CEs, NHS Trust CEs, SHA CEs, Care Trust CEs, Medical Directors, Directors of PH, Directors of Nursing, PCT PEC Chairs, NHS Trust Board Chairs, Special HA CEs, Directors of Infection Prevention and Control, Infection Control Teams, Health Protection Units, Chief Pharmacists Circulation List Description This guidance outlines newer evidence and approaches to delivering good infection control and environmental hygiene. It updates the 1994 guidance and takes into account a national framework for clinical governance which did not exist in 1994. Cross Ref N/A Superseded Docs Clostridium difficile Infection Prevention and Management (1994) Action Required CEs to consider with DIPCs and other colleagues Timing N/A Contact Details Healthcare Associated Infection and Antimicrobial Resistance Department of Health Room 528, Wellington House 133-155 Waterloo Road London SE1 8UG For Recipient's Use Front cover image: Clostridium difficile attached to intestinal cells. Reproduced courtesy of Dr Jan Hobot, Cardiff University School of Medicine. Clostridium difficile infection: How to deal with the problem Contents Foreword 1 Scope and purpose 2 Introduction 3 Why did CDI increase? 4 Approach to compiling the guidance 6 What is new in this guidance? 7 Core Guidance Key recommendations 9 Grading of recommendations 11 Summary of healthcare recommendations 12 1. -

Effects of Lactobacillus Rhamnosus and Enterococcus Faecalis Supplementation As Direct-Fed Microbials on Rumen Microbiota of Boer and Speckled Goat Breeds
veterinary sciences Article Effects of Lactobacillus rhamnosus and Enterococcus faecalis Supplementation as Direct-Fed Microbials on Rumen Microbiota of Boer and Speckled Goat Breeds Takalani Whitney Maake 1,2, Olayinka Ayobami Aiyegoro 2,3,* and Matthew Adekunle Adeleke 1 1 Discipline of Genetics, School of Life Sciences, College of Agricultural, Engineering and Science, University of Kwazulu-Natal, Westville Campus, Private Bag X 54001, Durban 4000, South Africa; [email protected] (T.W.M.); [email protected] (M.A.A.) 2 Gastrointestinal Microbiology and Biotechnology, Agricultural Research Council-Animal Production, Private Bag X 02, Irene 0062, South Africa 3 Research Unit for Environmental Sciences and Management, North-West University, Potchefstroom Campus, Private Bag X 1290, Potchefstroom 2520, South Africa * Correspondence: [email protected] or [email protected]; Tel.: +27-126-729-368 Abstract: The effects on rumen microbial communities of direct-fed probiotics, Lactobacillus rhamnosus and Enterococcus faecalis, singly and in combination as feed supplements to both the Boer and Speckled goats were studied using the Illumina Miseq platform targeting the V3-V4 region of the 16S rRNA microbial genes from sampled rumen fluid. Thirty-six goats of both the Boer and Speckled were divided into five experimental groups: (T1) = diet + Lactobacillus rhamnosus; (T2) = diet + Enterococcus faecalis; (T3) = diet + Lactobacillus rhamnosus + Enterococcus faecalis; (T4, positive control) = diet + antibiotic and (T5, negative control) = diet without antibiotics and without probiotics. Our results revealed that Bacteroidetes, Firmicutes, TM7, Proteobacteria, and Euryarchaeota dominate Citation: Maake, T.W.; Aiyegoro, O.A.; Adeleke, M.A. Effects of the bacterial communities. In our observations, Lactobacillus rhamnosus and Enterococcus faecalis Lactobacillus rhamnosus and supplements reduced the archaeal population of Methanomassiliicocca in the T1, T2 and T3 groups, Enterococcus faecalis Supplementation and caused an increase in the T4 group. -

Contribution of Enterococcus Faecalis to Urinary Tract Infection
Western University Scholarship@Western Electronic Thesis and Dissertation Repository 3-29-2018 3:00 PM Contribution of Enterococcus faecalis to urinary tract infection Samantha Ann Whiteside The University of Western Ontario Supervisor Reid, Gregor The University of Western Ontario Co-Supervisor Burton, Jeremy P. The University of Western Ontario Graduate Program in Microbiology and Immunology A thesis submitted in partial fulfillment of the equirr ements for the degree in Doctor of Philosophy © Samantha Ann Whiteside 2018 Follow this and additional works at: https://ir.lib.uwo.ca/etd Part of the Bacterial Infections and Mycoses Commons Recommended Citation Whiteside, Samantha Ann, "Contribution of Enterococcus faecalis to urinary tract infection" (2018). Electronic Thesis and Dissertation Repository. 5270. https://ir.lib.uwo.ca/etd/5270 This Dissertation/Thesis is brought to you for free and open access by Scholarship@Western. It has been accepted for inclusion in Electronic Thesis and Dissertation Repository by an authorized administrator of Scholarship@Western. For more information, please contact [email protected]. Abstract The purpose of this thesis was to increase understanding of enterococcal urinary tract infection (UTI), in particular, the response of Enterococcus to antibiotic prophylaxis in vitro and in vivo and enterococcal communication with the bladder. We studied the in vitro effects of trimethoprim-sulfamethoxazole (TMP/SMX) and nitrofurantoin, two of the most commonly used antibiotic treatments for the management of both UTI and recurrent UTI (RUTI), on Enterococcus faecalis attachment to urothelial cells. In doing so, we documented increases in bacterial attachment at growth inhibitory concentrations of nitrofurantoin, but not TMP/SMX. This increased virulence did not correlate with increased expression of virulence factors but was correlated with increased expression of three putative genes. -

Invanz® (Ertapenem for Injection)
INVANZ® (ERTAPENEM FOR INJECTION) To reduce the development of drug-resistant bacteria and maintain the effectiveness of INVANZ and other antibacterial drugs, INVANZ should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. For Intravenous or Intramuscular Use DESCRIPTION INVANZ∗ (Ertapenem for Injection) is a sterile, synthetic, parenteral, 1-β methyl-carbapenem that is structurally related to beta-lactam antibiotics. Chemically, INVANZ is described as [4R-[3(3S*,5S*),4α,5β,6β(R*)]]-3-[[5-[[(3- carboxyphenyl)amino]carbonyl]-3-pyrrolidinyl]thio]-6-(1-hydroxyethyl)-4-methyl-7-oxo-1- azabicyclo[3.2.0]hept-2-ene-2-carboxylic acid monosodium salt. Its molecular weight is 497.50. The empirical formula is C22H24N3O7SNa, and its structural formula is: OH _ CH3 H H COO 3CH S N Na+ O _ COO NH + N H 2 O Ertapenem sodium is a white to off-white hygroscopic, weakly crystalline powder. It is soluble in water and 0.9% sodium chloride solution, practically insoluble in ethanol, and insoluble in isopropyl acetate and tetrahydrofuran. INVANZ is supplied as sterile lyophilized powder for intravenous infusion after reconstitution with appropriate diluent (see DOSAGE AND ADMINISTRATION, PREPARATION OF SOLUTION) and transfer to 50 mL 0.9% Sodium Chloride Injection or for intramuscular injection following reconstitution with 1% lidocaine hydrochloride. Each vial contains 1.046 grams ertapenem sodium, equivalent to 1 gram ertapenem. The sodium content is approximately 137 mg (approximately 6.0 mEq). Each vial of INVANZ contains the following inactive ingredients: 175 mg sodium bicarbonate and sodium hydroxide to adjust pH to 7.5.