Ceftaroline Fosamil As an Alternative for a Severe Methicillin-Resistant Staphylococcus Aureus Infection: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ceftazidime for Injection) PHARMACY BULK PACKAGE – NOT for DIRECT INFUSION
PRESCRIBING INFORMATION FORTAZ® (ceftazidime for injection) PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION To reduce the development of drug-resistant bacteria and maintain the effectiveness of FORTAZ and other antibacterial drugs, FORTAZ should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION Ceftazidime is a semisynthetic, broad-spectrum, beta-lactam antibacterial drug for parenteral administration. It is the pentahydrate of pyridinium, 1-[[7-[[(2-amino-4 thiazolyl)[(1-carboxy-1-methylethoxy)imino]acetyl]amino]-2-carboxy-8-oxo-5-thia-1 azabicyclo[4.2.0]oct-2-en-3-yl]methyl]-, hydroxide, inner salt, [6R-[6α,7β(Z)]]. It has the following structure: The molecular formula is C22H32N6O12S2, representing a molecular weight of 636.6. FORTAZ is a sterile, dry-powdered mixture of ceftazidime pentahydrate and sodium carbonate. The sodium carbonate at a concentration of 118 mg/g of ceftazidime activity has been admixed to facilitate dissolution. The total sodium content of the mixture is approximately 54 mg (2.3 mEq)/g of ceftazidime activity. The Pharmacy Bulk Package vial contains 709 mg of sodium carbonate. The sodium content is approximately 54 mg (2.3mEq) per gram of ceftazidime. FORTAZ in sterile crystalline form is supplied in Pharmacy Bulk Packages equivalent to 6g of anhydrous ceftazidime. The Pharmacy Bulk Package bottle is a container of sterile preparation for parenteral use that contains many single doses. The contents are intended for use in a pharmacy admixture program and are restricted to the preparation of admixtures for intravenous use. THE PHARMACY BULK PACKAGE IS NOT FOR DIRECT INFUSION, FURTHER DILUTION IS REQUIRED BEFORE USE. -

Clinical Review (Cubicin)
Clinical Review Amol Purandare, MD NDA 021572 Cubicin (Daptomycin for injection) CLINICAL REVIEW Application Type NDA supplement Application Number(s) 21572 Priority or Standard Priority Submit Date(s) June 30, 2016 Received Date(s) June 30, 2016 PDUFA Goal Date March 30, 2017 (Major amendment) Division / Office DAIP/OAP Reviewer Name(s) Amol Purandare, MD Review Completion Date March 23, 2017 Established Name Daptomycin (Proposed) Trade Name Cubicin Therapeutic Class Cyclic Lipopeptide Applicant Cubist Pharmaceuticals Formulation(s) Injection Dosing Regimen 5 mg/kg (12-<18 years), 7 mg/kg (7-11 years), 9 mg/kg (2-6 years), and 10 mg/kg (1-< 2 years) Indication(s) Complicated Skin and Skin Structure Infections 1 Reference ID: 4075320 Clinical Review Amol Purandare, MD NDA 021572 Cubicin (Daptomycin for injection) Intended Population(s) Ages 1 year to <18 years Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT..........................................6 1.1 Recommendation on Regulatory Action ..............................................................6 1.2 Risk Benefit Assessment .....................................................................................6 1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies ....6 1.4 Recommendations for Postmarket Requirements and Commitments.................7 2 INTRODUCTION AND REGULATORY BACKGROUND .........................................7 2.1 Product Information .............................................................................................7 -

Severe Sepsis and Septic Shock Antibiotic Guide
Stanford Health Issue Date: 05/2017 Stanford Antimicrobial Safety and Sustainability Program Severe Sepsis and Septic Shock Antibiotic Guide Table 1: Antibiotic selection options for healthcare associated and/or immunocompromised patients • Healthcare associated: intravenous therapy, wound care, or intravenous chemotherapy within the prior 30 days, residence in a nursing home or other long-term care facility, hospitalization in an acute care hospital for two or more days within the prior 90 days, attendance at a hospital or hemodialysis clinic within the prior 30 days • Immunocompromised: Receiving chemotherapy, known systemic cancer not in remission, ANC <500, severe cell-mediated immune deficiency Table 2: Antibiotic selection options for community acquired, immunocompetent patients Table 3: Antibiotic selection options for patients with simple sepsis, community acquired, immunocompetent patients requiring hospitalization. Risk Factors for Select Organisms P. aeruginosa MRSA Invasive Candidiasis VRE (and other resistant GNR) Community acquired: • Known colonization with MDROs • Central venous catheter • Liver transplant • Prior IV antibiotics within 90 day • Recent MRSA infection • Broad-spectrum antibiotics • Known colonization • Known colonization with MDROs • Known MRSA colonization • + 1 of the following risk factors: • Prolonged broad antibacterial • Skin & Skin Structure and/or IV access site: ♦ Parenteral nutrition therapy Hospital acquired: ♦ Purulence ♦ Dialysis • Prolonged profound • Prior IV antibiotics within 90 days ♦ Abscess -

Methicillin-Resistant Staphylococcus Aureus Infections in County Jails
Prevention, Treatment, and Containment of Methicillin-Resistant Staphylococcus aureus Infections in County Jails Texas Department of State Health Services and Correctional Facilities Workgroup September 2006 2 Clinical guidelines are being made available to the public for informational purposes only. Texas Department of State Health Services (DSHS) does not warrant these guidelines for any other purpose and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient-specific. 3 We acknowledge the Federal Bureau of Prisons Clinical Practice Guidelines for the Management Of Methicillin-Resistant Staphylococcus Aureus (MRSA) Infections, August 2005 for general organization and content of this document. 4 Table of Contents Introduction ......................................................................................................................... 6 Colonization ......................................................................................................................... 6 Transmission........................................................................................................................ 7 Screening and Surveillance ................................................................................................ 7 Diagnosis .............................................................................................................................. 8 -

Antimicrobial Stewardship Guidance
Antimicrobial Stewardship Guidance Federal Bureau of Prisons Clinical Practice Guidelines March 2013 Clinical guidelines are made available to the public for informational purposes only. The Federal Bureau of Prisons (BOP) does not warrant these guidelines for any other purpose, and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient-specific. Consult the BOP Clinical Practice Guidelines Web page to determine the date of the most recent update to this document: http://www.bop.gov/news/medresources.jsp Federal Bureau of Prisons Antimicrobial Stewardship Guidance Clinical Practice Guidelines March 2013 Table of Contents 1. Purpose ............................................................................................................................................. 3 2. Introduction ...................................................................................................................................... 3 3. Antimicrobial Stewardship in the BOP............................................................................................ 4 4. General Guidance for Diagnosis and Identifying Infection ............................................................. 5 Diagnosis of Specific Infections ........................................................................................................ 6 Upper Respiratory Infections (not otherwise specified) .............................................................................. -

Ceftaroline in the Management of Complicated Skin and Soft Tissue Infections and Community Acquired Pneumonia
Journal name: Therapeutics and Clinical Risk Management Article Designation: Review Year: 2015 Volume: 11 Therapeutics and Clinical Risk Management Dovepress Running head verso: Mpenge and MacGowan Running head recto: Ceftaroline in the management of cSSTI and CAP open access to scientific and medical research DOI: http://dx.doi.org/10.2147/TCRM.S75412 Open Access Full Text Article REVIEW Ceftaroline in the management of complicated skin and soft tissue infections and community acquired pneumonia Mbiye A Mpenge¹ Abstract: Ceftaroline is a new parenteral cephalosporin approved by the European Medicines Alasdair P MacGowan² Agency (EMA) and the US Food and Drug Administration (FDA) for the treatment of com- plicated skin and soft tissue infections (cSSTIs) including those due to methicillin-resistant ¹Department of Medical Microbiology, University Hospitals Bristol NHS Staphylococcus aureus (MRSA), and community-acquired pneumonia (CAP). Ceftaroline has Trust, Bristol Royal Infirmary, Bristol, broad-spectrum activity against gram-positive and gram-negative bacteria and exerts its bacteri- England; ²Department of Medical Microbiology, North Bristol NHS cidal effects by binding to penicillin-binding proteins (PBPs), resulting in inhibition of bacterial Trust, Southmead Hospital, Bristol, cell wall synthesis. It binds to PBP 2a of MRSA with high affinity and also binds to all six PBPs England in Streptococcus pneumoniae. In in vitro studies, ceftaroline demonstrated potent activity against Staphylococcus aureus (including MRSA and vancomycin-intermediate isolates), Streptococ- For personal use only. cus pneumoniae (including multidrug resistant isolates), Haemophilus influenzae, Moraxella catarrhalis, and many common gram-negative pathogens, excluding extended spectrum beta- lactamase (ESBL)-producing Enterobacteriaceae and Pseudomonas aeruginosa. In Phase II and Phase III clinical trials, ceftaroline was noninferior to its comparator agents and demonstrated high clinical cure rates in the treatment of cSSTIs and CAP. -

Synermox 500 Mg/125 Mg Tablets
New Zealand Data Sheet 1. PRODUCT NAME Synermox 500 mg/125 mg Tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Synermox 500 mg/125 mg Tablets: Each film‐coated tablet contains amoxicillin trihydrate equivalent to 500 mg amoxicillin, with potassium clavulanate equivalent to 125 mg clavulanic acid. Excipient(s) with known effect For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Synermox 500 mg/125 mg Tablets: White to off‐white, oval shaped film‐coated tablets, debossed with “RX713” on one side and plain on the other. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Synermox is indicated in adults and children (see sections 4.2, 4.4 and 5.1) for short term treatment of common bacterial infections such as: Upper Respiratory Tract Infections (including ENT) e.g. Tonsillitis, sinusitis, otitis media. Lower Respiratory Tract Infection e.g. acute exacerbations of chronic bronchitis, lobar and broncho‐pneumonia. Genito‐urinary Tract Infections e.g. Cystitis, urethritis, pyelonephritis, female genital infections. Skin and Soft Tissue Infections. Bone and Joint Infections e.g. Osteomyelitis. Other Infections e.g. septic abortion, puerperal sepsis, intra‐abdominal sepsis, septicaemia, peritonitis, post‐surgical infections. Synermox is indicated for prophylaxis against infection which may be associated with major surgical procedures such as those involving: Gastro‐intestinal tract Pelvic cavity 1 | Page Head and neck Cardiac Renal Joint replacement Biliary tract surgery Infections caused by amoxicillin susceptible organisms are amenable to Synermox treatment due to its amoxicillin content. Mixed infections caused by amoxicillin susceptible organisms in conjunction with Synermox‐susceptible beta‐lactamase‐producing organisms may therefore be treated by Synermox. -

Consideration of Antibacterial Medicines As Part Of
Consideration of antibacterial medicines as part of the revisions to 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee on Selection and Use of Essential Medicines (see The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization; 2019 (WHO Technical Report Series, No. 1021). Licence: CC BY-NC-SA 3.0 IGO: https://apps.who.int/iris/bitstream/handle/10665/330668/9789241210300-eng.pdf?ua=1) and Corrigenda (March 2020) – TRS1021 (https://www.who.int/medicines/publications/essentialmedicines/TRS1021_corrigenda_March2020. pdf?ua=1). Executive summary of the report: https://apps.who.int/iris/bitstream/handle/10665/325773/WHO- MVP-EMP-IAU-2019.05-eng.pdf?ua=1. -
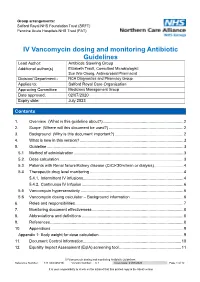
IV Vancomycin Dosing and Monitoring Antibiotic Guidelines Reference Number: 144TD(C)25(H3) Version Number: 6.1 Issue Date: 21/07/2020 Page 1 of 12
Group arrangements: Salford Royal NHS Foundation Trust (SRFT) Pennine Acute Hospitals NHS Trust (PAT) IV Vancomycin dosing and monitoring Antibiotic Guidelines Lead Author: Antibiotic Steering Group Additional author(s) Elizabeth Trautt, Consultant Microbiologist; Sue Wei Chong, Antimicrobial Pharmacist Division/ Department:: NCA Diagnostics and Pharmacy Group Applies to: Salford Royal Care Organisation Approving Committee Medicines Management Group Date approved: 02/07/2020 Expiry date: July 2023 Contents Contents 1. Overview (What is this guideline about?) ....................................................................... 2 2. Scope (Where will this document be used?) .................................................................. 2 3. Background (Why is this document important?) ............................................................. 2 4. What is new in this version? ............................................................................................ 3 5. Guideline ......................................................................................................................... 3 5.1 Method of administration ................................................................................................. 3 5.2. Dose calculation .............................................................................................................. 3 5.3. Patients with Renal failure/Kidney disease (CrCl<30ml/min or dialysis) .......................... 4 5.4 Therapeutic drug level monitoring .................................................................................. -

Eml-2017-Antibacterials-Eng.Pdf
Consideration of antibacterial medicines as part of the revisions to 2017 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2017 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee, 2017 and this summary should be read in conjunction with the full report (WHO Technical Report Series, No. 1006; http://apps.who.int/iris/bitstream/10665/259481/1/9789241210157-eng.pdf?ua=1). The revised lists of essential medicines (in English) are available as follows: 2017 WHO Model List of Essential Medicines for adults (EML) http://www.who.int/medicines/publications/essentialmedicines/20th_EML2017_FINAL_amend edAug2017.pdf?ua=1 2017 Model List of Essential Medicines for children (EMLc) http://www.who.int/medicines/publications/essentialmedicines/6th_EMLc2017_FINAL_amend edAug2017.pdf?ua=1 Summary of changes to Section 6.2 Antibacterials: Section 6 of the EML covers anti-infective medicines. Disease-specific subsections within Section 6, such as those covering medicines for tuberculosis, HIV, hepatitis and malaria, have been regularly reviewed and updated, taking into consideration relevant WHO treatment guidelines. -

Invanz® (Ertapenem for Injection)
INVANZ® (ERTAPENEM FOR INJECTION) To reduce the development of drug-resistant bacteria and maintain the effectiveness of INVANZ and other antibacterial drugs, INVANZ should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. For Intravenous or Intramuscular Use DESCRIPTION INVANZ∗ (Ertapenem for Injection) is a sterile, synthetic, parenteral, 1-β methyl-carbapenem that is structurally related to beta-lactam antibiotics. Chemically, INVANZ is described as [4R-[3(3S*,5S*),4α,5β,6β(R*)]]-3-[[5-[[(3- carboxyphenyl)amino]carbonyl]-3-pyrrolidinyl]thio]-6-(1-hydroxyethyl)-4-methyl-7-oxo-1- azabicyclo[3.2.0]hept-2-ene-2-carboxylic acid monosodium salt. Its molecular weight is 497.50. The empirical formula is C22H24N3O7SNa, and its structural formula is: OH _ CH3 H H COO 3CH S N Na+ O _ COO NH + N H 2 O Ertapenem sodium is a white to off-white hygroscopic, weakly crystalline powder. It is soluble in water and 0.9% sodium chloride solution, practically insoluble in ethanol, and insoluble in isopropyl acetate and tetrahydrofuran. INVANZ is supplied as sterile lyophilized powder for intravenous infusion after reconstitution with appropriate diluent (see DOSAGE AND ADMINISTRATION, PREPARATION OF SOLUTION) and transfer to 50 mL 0.9% Sodium Chloride Injection or for intramuscular injection following reconstitution with 1% lidocaine hydrochloride. Each vial contains 1.046 grams ertapenem sodium, equivalent to 1 gram ertapenem. The sodium content is approximately 137 mg (approximately 6.0 mEq). Each vial of INVANZ contains the following inactive ingredients: 175 mg sodium bicarbonate and sodium hydroxide to adjust pH to 7.5. -

Methicillin-Resistant Staphylococcus Aureus (MRSA)
Methicillin-Resistant Staphylococcus Aureus (MRSA) Over the past several decades, the incidence of resistant gram-positive organisms has risen in the United States. MRSA strains, first identified in the 1960s in England, were first observed in the U.S. in the mid 1980s.1 Resistance quickly developed, increasing from 2.4% in 1979 to 29% in 1991.2 The current prevalence for MRSA in hospitals and other facilities ranges from <10% to 65%. In 1999, MRSA accounted for more than 50% of all Staphylococcus aureus isolates within U.S. intensive care units.3, 4 The past years, however, outbreaks of MRSA have also been seen in the community setting, particularly among preschool-age children, some of whom have attended day-care centers.5, 6, 7 MRSA does not appear to be more virulent than methicillin-sensitive Staphylococcus aureus, but certainly poses a greater treatment challenge. MRSA also has been associated with higher hospital costs and mortality.8 Within a decade of its development, methicillin resistance to Staphylococcus aureus emerged.9 MRSA strains generally are now resistant to other antimicrobial classes including aminoglycosides, beta-lactams, carbapenems, cephalosporins, fluoroquinolones and macrolides.10,11 Most of the resistance was secondary to production of beta-lactamase enzymes or intrinsic resistance with alterations in penicillin-binding proteins. Staphylococcus aureus is the most frequent cause of nosocomial pneumonia and surgical- wound infections and the second most common cause of nosocomial bloodstream infections.12 Long-term care facilities (LTCFs) have developed rates of MRSA ranging from 25%-35%. MRSA rates may be higher in LTCFs if they are associated with hospitals that have higher rates.13 Transmission of MRSA generally occurs through direct or indirect contact with a reservoir.