Uncommon Vancomycin-Induced Side Effects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ceftazidime for Injection) PHARMACY BULK PACKAGE – NOT for DIRECT INFUSION
PRESCRIBING INFORMATION FORTAZ® (ceftazidime for injection) PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION To reduce the development of drug-resistant bacteria and maintain the effectiveness of FORTAZ and other antibacterial drugs, FORTAZ should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION Ceftazidime is a semisynthetic, broad-spectrum, beta-lactam antibacterial drug for parenteral administration. It is the pentahydrate of pyridinium, 1-[[7-[[(2-amino-4 thiazolyl)[(1-carboxy-1-methylethoxy)imino]acetyl]amino]-2-carboxy-8-oxo-5-thia-1 azabicyclo[4.2.0]oct-2-en-3-yl]methyl]-, hydroxide, inner salt, [6R-[6α,7β(Z)]]. It has the following structure: The molecular formula is C22H32N6O12S2, representing a molecular weight of 636.6. FORTAZ is a sterile, dry-powdered mixture of ceftazidime pentahydrate and sodium carbonate. The sodium carbonate at a concentration of 118 mg/g of ceftazidime activity has been admixed to facilitate dissolution. The total sodium content of the mixture is approximately 54 mg (2.3 mEq)/g of ceftazidime activity. The Pharmacy Bulk Package vial contains 709 mg of sodium carbonate. The sodium content is approximately 54 mg (2.3mEq) per gram of ceftazidime. FORTAZ in sterile crystalline form is supplied in Pharmacy Bulk Packages equivalent to 6g of anhydrous ceftazidime. The Pharmacy Bulk Package bottle is a container of sterile preparation for parenteral use that contains many single doses. The contents are intended for use in a pharmacy admixture program and are restricted to the preparation of admixtures for intravenous use. THE PHARMACY BULK PACKAGE IS NOT FOR DIRECT INFUSION, FURTHER DILUTION IS REQUIRED BEFORE USE. -

Severe Sepsis and Septic Shock Antibiotic Guide
Stanford Health Issue Date: 05/2017 Stanford Antimicrobial Safety and Sustainability Program Severe Sepsis and Septic Shock Antibiotic Guide Table 1: Antibiotic selection options for healthcare associated and/or immunocompromised patients • Healthcare associated: intravenous therapy, wound care, or intravenous chemotherapy within the prior 30 days, residence in a nursing home or other long-term care facility, hospitalization in an acute care hospital for two or more days within the prior 90 days, attendance at a hospital or hemodialysis clinic within the prior 30 days • Immunocompromised: Receiving chemotherapy, known systemic cancer not in remission, ANC <500, severe cell-mediated immune deficiency Table 2: Antibiotic selection options for community acquired, immunocompetent patients Table 3: Antibiotic selection options for patients with simple sepsis, community acquired, immunocompetent patients requiring hospitalization. Risk Factors for Select Organisms P. aeruginosa MRSA Invasive Candidiasis VRE (and other resistant GNR) Community acquired: • Known colonization with MDROs • Central venous catheter • Liver transplant • Prior IV antibiotics within 90 day • Recent MRSA infection • Broad-spectrum antibiotics • Known colonization • Known colonization with MDROs • Known MRSA colonization • + 1 of the following risk factors: • Prolonged broad antibacterial • Skin & Skin Structure and/or IV access site: ♦ Parenteral nutrition therapy Hospital acquired: ♦ Purulence ♦ Dialysis • Prolonged profound • Prior IV antibiotics within 90 days ♦ Abscess -

Antimicrobial Stewardship Guidance
Antimicrobial Stewardship Guidance Federal Bureau of Prisons Clinical Practice Guidelines March 2013 Clinical guidelines are made available to the public for informational purposes only. The Federal Bureau of Prisons (BOP) does not warrant these guidelines for any other purpose, and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient-specific. Consult the BOP Clinical Practice Guidelines Web page to determine the date of the most recent update to this document: http://www.bop.gov/news/medresources.jsp Federal Bureau of Prisons Antimicrobial Stewardship Guidance Clinical Practice Guidelines March 2013 Table of Contents 1. Purpose ............................................................................................................................................. 3 2. Introduction ...................................................................................................................................... 3 3. Antimicrobial Stewardship in the BOP............................................................................................ 4 4. General Guidance for Diagnosis and Identifying Infection ............................................................. 5 Diagnosis of Specific Infections ........................................................................................................ 6 Upper Respiratory Infections (not otherwise specified) .............................................................................. -

Synermox 500 Mg/125 Mg Tablets
New Zealand Data Sheet 1. PRODUCT NAME Synermox 500 mg/125 mg Tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Synermox 500 mg/125 mg Tablets: Each film‐coated tablet contains amoxicillin trihydrate equivalent to 500 mg amoxicillin, with potassium clavulanate equivalent to 125 mg clavulanic acid. Excipient(s) with known effect For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Synermox 500 mg/125 mg Tablets: White to off‐white, oval shaped film‐coated tablets, debossed with “RX713” on one side and plain on the other. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Synermox is indicated in adults and children (see sections 4.2, 4.4 and 5.1) for short term treatment of common bacterial infections such as: Upper Respiratory Tract Infections (including ENT) e.g. Tonsillitis, sinusitis, otitis media. Lower Respiratory Tract Infection e.g. acute exacerbations of chronic bronchitis, lobar and broncho‐pneumonia. Genito‐urinary Tract Infections e.g. Cystitis, urethritis, pyelonephritis, female genital infections. Skin and Soft Tissue Infections. Bone and Joint Infections e.g. Osteomyelitis. Other Infections e.g. septic abortion, puerperal sepsis, intra‐abdominal sepsis, septicaemia, peritonitis, post‐surgical infections. Synermox is indicated for prophylaxis against infection which may be associated with major surgical procedures such as those involving: Gastro‐intestinal tract Pelvic cavity 1 | Page Head and neck Cardiac Renal Joint replacement Biliary tract surgery Infections caused by amoxicillin susceptible organisms are amenable to Synermox treatment due to its amoxicillin content. Mixed infections caused by amoxicillin susceptible organisms in conjunction with Synermox‐susceptible beta‐lactamase‐producing organisms may therefore be treated by Synermox. -
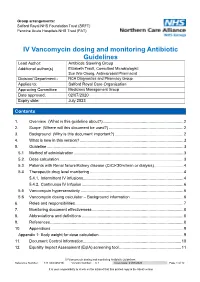
IV Vancomycin Dosing and Monitoring Antibiotic Guidelines Reference Number: 144TD(C)25(H3) Version Number: 6.1 Issue Date: 21/07/2020 Page 1 of 12
Group arrangements: Salford Royal NHS Foundation Trust (SRFT) Pennine Acute Hospitals NHS Trust (PAT) IV Vancomycin dosing and monitoring Antibiotic Guidelines Lead Author: Antibiotic Steering Group Additional author(s) Elizabeth Trautt, Consultant Microbiologist; Sue Wei Chong, Antimicrobial Pharmacist Division/ Department:: NCA Diagnostics and Pharmacy Group Applies to: Salford Royal Care Organisation Approving Committee Medicines Management Group Date approved: 02/07/2020 Expiry date: July 2023 Contents Contents 1. Overview (What is this guideline about?) ....................................................................... 2 2. Scope (Where will this document be used?) .................................................................. 2 3. Background (Why is this document important?) ............................................................. 2 4. What is new in this version? ............................................................................................ 3 5. Guideline ......................................................................................................................... 3 5.1 Method of administration ................................................................................................. 3 5.2. Dose calculation .............................................................................................................. 3 5.3. Patients with Renal failure/Kidney disease (CrCl<30ml/min or dialysis) .......................... 4 5.4 Therapeutic drug level monitoring .................................................................................. -

Eml-2017-Antibacterials-Eng.Pdf
Consideration of antibacterial medicines as part of the revisions to 2017 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2017 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee, 2017 and this summary should be read in conjunction with the full report (WHO Technical Report Series, No. 1006; http://apps.who.int/iris/bitstream/10665/259481/1/9789241210157-eng.pdf?ua=1). The revised lists of essential medicines (in English) are available as follows: 2017 WHO Model List of Essential Medicines for adults (EML) http://www.who.int/medicines/publications/essentialmedicines/20th_EML2017_FINAL_amend edAug2017.pdf?ua=1 2017 Model List of Essential Medicines for children (EMLc) http://www.who.int/medicines/publications/essentialmedicines/6th_EMLc2017_FINAL_amend edAug2017.pdf?ua=1 Summary of changes to Section 6.2 Antibacterials: Section 6 of the EML covers anti-infective medicines. Disease-specific subsections within Section 6, such as those covering medicines for tuberculosis, HIV, hepatitis and malaria, have been regularly reviewed and updated, taking into consideration relevant WHO treatment guidelines. -

Can Amoxicillin Clavulanate Be Used for Treating MRSA?
ORIGINAL ARTICLE Can amoxicillin clavulanate be used for treating MRSA? Sana Jamil1, Uzma Saad2, Saleem Hafiz1 Jamil S, Saad U, Hafiz S. Can amoxicillin clavulanate be used for treating positive for Beta lactamase production 52.1% of these Beta lactamase MRSA? J Pharmacol Res December-2017;1(1):21-23. producing MRSA were sensitive to amoxicillin-clavulanate and the remaining (47.9%) were resistant. Objective: To determine the frequency of beta lactamase producing Conclusion: If beta lactamase producing Staphlococcus aureus are tested Staphlococcus aureus and their sensitivity to Amoxicillin clavulanate in against beta-lactam antimicrobial agents in combination with clavulanic major cities of Pakistan. acid or sulbactam (Beta-lactamase inhibitors), they become susceptible to Setting: Various laboratories of the country with one as the central the Beta-lactam antimicrobial agents. This might have therapeutic and Laboratory. epidemiological implications in near future. Materials and Methods: Seven hundred and ninety two consecutive Key Words: Methicillin resistant Staphylococcus aureus; Vancomycin clinical isolates of Staphylococcus aureus were collected from 8 intermediate Staphylococcus aureus; Vancomycin resistant Staphylococcus laboratories all over Pakistan i.e. Karachi, Peshawar, Lahore, Sukkhur, aureus; Clinical laboratory standard institute; Penicillinase resistant Islamabad, Quetta, and Mirpur, Azad Kashmir. Antibiotic sensitivity was penicillins; Minimum inhibitory concentration; Penicillin binding proteins; done by Kirby Bauer disc diffusion method and Beta lactamase production Center of disease control was identified by using Nitrocefin test. Results: Forty two percent of the isolates were found to be Methicillin resistant Staphylococcus aureus (MRSA) out of which 87.9% were INTRODUCTION lactamase producing MRSA in Pakistan and its sensitivity to Amoxicillin clavulanate. -

Ceftaroline Fosamil As an Alternative for a Severe Methicillin-Resistant Staphylococcus Aureus Infection: a Case Report
Open Access Case Report DOI: 10.7759/cureus.3776 Ceftaroline Fosamil as an Alternative for a Severe Methicillin-resistant Staphylococcus aureus Infection: A Case Report Talha N. Jilani 1 , Syed O. Masood 2 1. Internal Medicine, Ziauddin University, Karachi, PAK 2. Infectious Diseases, University of Cincinnati Medical Center, Cincinnati, USA Corresponding author: Talha N. Jilani, [email protected] Abstract Bacteremia secondary to methicillin-resistant Staphylococcus aureus (MRSA) is a dreaded medical condition that is not only associated with a significant medical cost but also carries high morbidity and mortality. The poor clinical outcomes seen in MRSA patients and the nephrotoxic effects of high-doses of vancomycin are challenging its current status as the first-line treatment for MRSA. Fortunately, vancomycin-intermediate- staphylococcus aureus (VISA) and vancomycin-resistant-staphylococcus aureus (VRSA) are not common in the United States. However, MRSA still presents different treatment challenges. Elevated vancomycin minimum inhibitory concentrations (MICs) commonly result in decreased efficacy and an increased probability of treatment failure, prompting the use of alternative agents. Although daptomycin is an alternative, adverse effects (i.e., elevations in serum creatine phosphokinase (CPK), drug-induced myopathy, peripheral neuropathy, and eosinophilic pneumonia) may limit its use in some patients. In the search for a suitable replacement for vancomycin, great promise has been shown by anti-MRSA cephalosporins. We present a case of MRSA bacteremia and endocarditis requiring a different approach to treatment as compared to traditional treatment with vancomycin alone. This case report describes the successful treatment of MRSA bacteremia with ceftaroline fosamil in a patient who responded poorly to conventional therapy, specifically vancomycin, due to an elevated MIC (2 µg/mL). -

Vancomycin Injection, USP for Intravenous Use Only
Vancomycin Injection, USP For Intravenous Use Only To reduce the development of drug-resistant bacteria and maintain the effectiveness of vancomycin and other antibacterial drugs, vancomycin should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION Vancomycin Injection, USP in the GALAXY plastic container (PL 2040) contains vancomycin, added as Vancomycin Hydrochloride, USP. It is a tricyclic glycopeptide antibiotic drug derived from Amycolatopsis orientalis (formerly Nocardia orientalis). The molecular formula is C66H75Cl2N9O24•HCl and the molecular weight is 1,485.71. Vancomycin hydrochloride has the following structural formula: Vancomycin Injection, USP in the GALAXY plastic container (PL 2040) is a frozen, iso osmotic, sterile, nonpyrogenic premixed 100 mL, 150 mL, or 200 mL solution containing 500 mg, 750 mg, or 1 g Vancomycin respectively as Vancomycin hydrochloride. Each 100 mL of solution contains approximately 5 g of Dextrose Hydrous, USP or 0.9 g of Sodium Chloride, USP. The pH of the solution may have been adjusted with hydrochloric acid and/or sodium hydroxide. Thawed solutions have a pH in the range of 3.0 to 5.0. After thawing to room temperature, this solution is intended for intravenous use only. Reference ID: 4159835 This GALAXY container is fabricated from a specially designed multilayer plastic (PL 2040). Solutions are in contact with the polyethylene layer of this container and can leach out certain chemical components of the plastic in very small amounts within the expiration period. The suitability of the plastic has been confirmed in tests in animals according to USP biological tests for plastic containers as well as by tissue culture toxicity studies. -

Use of Ceftaroline in Hospitalized Patients with and Without COVID-19: a Descriptive Cross-Sectional Study
antibiotics Article Use of Ceftaroline in Hospitalized Patients with and without COVID-19: A Descriptive Cross-Sectional Study Daniele Roberto Giacobbe 1,2,*, Chiara Russo 1,2, Veronica Martini 3, Silvia Dettori 1,2, Federica Briano 1,2, Michele Mirabella 2, Federica Portunato 2, Chiara Dentone 2, Sara Mora 4, Mauro Giacomini 4 , Marco Berruti 1,2 and Matteo Bassetti 1,2 1 Department of Health Sciences, University of Genoa, 16132 Genoa, Italy; [email protected] (C.R.); [email protected] (S.D.); [email protected] (F.B.); [email protected] (M.B.); [email protected] (M.B.) 2 Clinica Malattie Infettive, San Martino Policlinico Hospital—IRCCS, 16132 Genoa, Italy; [email protected] (M.M.); [email protected] (F.P.); [email protected] (C.D.) 3 School of Medicine, University of Genoa, 16132 Genoa, Italy; [email protected] 4 Department of Informatics Bioengineering, Robotics, and Systems Engineering (DIBRIS), University of Genoa, 16145 Genoa, Italy; [email protected] (S.M.); [email protected] (M.G.) * Correspondence: [email protected] Abstract: A single-center cross-sectional study was conducted to describe the use of ceftaroline in a large teaching hospital in Northern Italy, during a period also including the first months of the coronavirus disease 2019 (COVID-19) pandemic. The primary objective was to describe the use of ceftaroline in terms of indications and characteristics of patients. A secondary objective was to Citation: Giacobbe, D.R.; Russo, C.; describe the rate of favorable clinical response in patients with bloodstream infections (BSI) due to Martini, V.; Dettori, S.; Briano, F.; methicillin-resistant Staphylococcus aureus (MRSA-BSI) receiving ceftaroline. -

VANCOMYCIN DOSING and MONITORING GUIDELINES (NB Provincial Health Authorities Anti-Infective Stewardship Committee)
Amended: October 2020 VANCOMYCIN DOSING AND MONITORING GUIDELINES (NB Provincial Health Authorities Anti-Infective Stewardship Committee) GENERAL COMMENTS • Vancomycin is a glycopeptide antibiotic with bactericidal activity • It is active against gram-positive bacteria, including methicillin-resistant staphylococcus (MRSA) • Vancomycin is less effective than beta-lactams against Staphylococcus aureus that is susceptible to cloxacillin/methicillin • Vancomycin exhibits time-dependent killing: its effect depends primarily upon the time the concentration exceeds the organism’s Minimum Inhibitory Concentration (MIC) • These guidelines pertain to IV vancomycin only; they do not apply to PO vancomycin, which is not absorbed • Ensure that an adequate mg/kg dose and appropriate interval are ordered initially. Adjust the dose if necessary immediately; do not wait for a confirmatory trough level. • When managing a severe Staphylococcus aureus infection (e.g., bacteremia), an Infectious Diseases consultation is strongly encouraged. VANCOMYCIN IN ADULT PATIENTS ADULT INITIAL DOSE Loading dose: • Consider using a loading dose in patients with: o severe infections where rapid attainment of target level of 10-15 mg/mL is desired o significant renal dysfunction in order to decrease the time required to attain steady state • Recommended dose: 25-30 mg/kg IV o based on actual body weight, for 1 dose, followed by maintenance dose separated by recommended dosing interval o consider capping the loading dose at a maximum of 3g o loading doses DO NOT need to -

Therapeutic Monitoring of Vancomycin in Adult Patients
ASHP Therapeutic Position Statements 685 Therapeutic Monitoring of Vancomycin in Adult Patients: A Consensus Review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists Vancomycin is a glycopeptide antibiotic that has been in and consideration of these suggestions, the document was clinical use for nearly 50 years as a penicillin alternative revised and circulated among the committee and supporting to treat penicillinase-producing strains of Staphylococcus organizations for final comment. This consensus review rep- aureus. It is one of the most widely used antibiotics in the resents the opinion of the majority of committee members. United States for the treatment of serious gram-positive in- A search of PubMed was conducted using the follow- fections involving methicillin-resistant S. aureus (MRSA).1 ing search terms: vancomycin pharmacokinetics, pharmaco- Early use of vancomycin was associated with a number of dynamics, efficacy, resistance, and toxicity. All relevant adverse effects, including infusion-related toxicities, neph- and available peer-reviewed studies in the English language rotoxicity, and possible ototoxicity. Upon further investi- published between 1958 and 2008 were considered. Studies gation, it appears that the impurities in early formulations were rated by their quality of evidence, and the subsequent of vancomycin caused many of these adverse events.1-4 Its recommendations were graded using the classification sche- overall use was curtailed significantly with the development mata of the Canadian Medical Association (Table 1).13 of semisynthetic penicillins (e.g., methicillin, oxacillin, naf- Recommendations of the expert panel are presented in Table 2.