Ceftazidime for Injection) PHARMACY BULK PACKAGE – NOT for DIRECT INFUSION
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Activity of Aztreonam in Combination with Ceftazidime-Avibactam Against
Diagnostic Microbiology and Infectious Disease 99 (2021) 115227 Contents lists available at ScienceDirect Diagnostic Microbiology and Infectious Disease journal homepage: www.elsevier.com/locate/diagmicrobio Activity of aztreonam in combination with ceftazidime–avibactam against serine- and metallo-β-lactamase–producing ☆ ☆☆ ★ Pseudomonas aeruginosa , , Michelle Lee a, Taylor Abbey a, Mark Biagi b, Eric Wenzler a,⁎ a College of Pharmacy, University of Illinois at Chicago, Chicago, IL, USA b College of Pharmacy, University of Illinois at Chicago, Rockford, IL, USA article info abstract Article history: Existing data support the combination of aztreonam and ceftazidime–avibactam against serine-β-lactamase Received 29 June 2020 (SBL)– and metallo-β-lactamase (MBL)–producing Enterobacterales, although there is a paucity of data against Received in revised form 15 September 2020 SBL- and MBL-producing Pseudomonas aeruginosa. In this study, 5 SBL- and MBL-producing P. aeruginosa (1 Accepted 19 September 2020 IMP, 4 VIM) were evaluated against aztreonam and ceftazidime–avibactam alone and in combination via broth Available online xxxx microdilution and time-kill analyses. All 5 isolates were nonsusceptible to aztreonam, aztreonam–avibactam, – – Keywords: and ceftazidime avibactam. Combining aztreonam with ceftazidime avibactam at subinhibitory concentrations Metallo-β-lactamase produced synergy and restored bactericidal activity in 4/5 (80%) isolates tested. These results suggest that the VIM combination of aztreonam and ceftazidime–avibactam may be a viable treatment option against SBL- and IMP MBL-producing P. aeruginosa. Aztreonam © 2020 Elsevier Inc. All rights reserved. Ceftazidime–avibactam Synergy 1. Introduction of SBLs and MBLs harbored by P. aeruginosa are fundamentally different than those in Enterobacterales (Alm et al., 2015; Kazmierczak et al., The rapid global dissemination of Ambler class B metallo-β- 2016; Periasamy et al., 2020; Poirel et al., 2000; Watanabe et al., lactamase (MBL) enzymes along with their increasing diversity across 1991). -

Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and Its Application
Infect Dis Ther (2017) 6:57–67 DOI 10.1007/s40121-016-0144-8 REVIEW Use of Ceftaroline Fosamil in Children: Review of Current Knowledge and its Application Juwon Yim . Leah M. Molloy . Jason G. Newland Received: November 10, 2016 / Published online: December 30, 2016 Ó The Author(s) 2016. This article is published with open access at Springerlink.com ABSTRACT infections, CABP caused by penicillin- and ceftriaxone-resistant S. pneumoniae and Ceftaroline is a novel cephalosporin recently resistant Gram-positive infections that fail approved in children for treatment of acute first-line antimicrobial agents. However, bacterial skin and soft tissue infections and limited data are available on tolerability in community-acquired bacterial pneumonia neonates and infants younger than 2 months (CABP) caused by methicillin-resistant of age, and on pharmacokinetic characteristics Staphylococcus aureus, Streptococcus pneumoniae in children with chronic medical conditions and other susceptible bacteria. With a favorable and those with invasive, complicated tolerability profile and efficacy proven in infections. In this review, the microbiological pediatric patients and excellent in vitro profile of ceftaroline, its mechanism of action, activity against resistant Gram-positive and and pharmacokinetic profile will be presented. Gram-negative bacteria, ceftaroline may serve Additionally, clinical evidence for use in as a therapeutic option for polymicrobial pediatric patients and proposed place in therapy is discussed. Enhanced content To view enhanced content for this article go to http://www.medengine.com/Redeem/ 1F47F0601BB3F2DD. Keywords: Antibiotic resistance; Ceftaroline J. Yim (&) fosamil; Children; Methicillin-resistant St. John Hospital and Medical Center, Detroit, MI, Staphylococcus aureus; Streptococcus pneumoniae USA e-mail: [email protected] L. -

Global Assessment of the Antimicrobial Activity of Polymyxin B Against 54 731 Clinical Isolates of Gram-Negative Bacilli
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector ORIGINAL ARTICLE 10.1111/j.1469-0691.2005.01351.x Global assessment of the antimicrobial activity of polymyxin B against 54 731 clinical isolates of Gram-negative bacilli: report from the SENTRY antimicrobial surveillance programme (2001–2004) A. C. Gales1, R. N. Jones2,3 and H. S. Sader1,2 1Division of Infectious Diseases, Universidade Federal de Sa˜o Paulo, Sa˜o Paulo, Brazil, 2JMI Laboratories, North Liberty, IA, USA, and 3Tufts University School of Medicine, Boston, MA, USA ABSTRACT In total, 54 731 Gram-negative bacilli isolated worldwide between 2001 and 2004 from diverse sites of infection were tested for susceptibility to polymyxin B by the broth reference microdilution method, with interpretation of results according to CLSI (formerly NCCLS) guidelines. Polymyxin B showed excellent potency and spectrum against 8705 Pseudomonas aeruginosa and 2621 Acinetobacter spp. isolates (MIC50, £ ⁄ ⁄ 1mg L and MIC90,2mg L for both pathogens). Polymyxin B resistance rates were slightly higher for carbapenem-resistant P. aeruginosa (2.7%) and Acinetobacter spp. (2.8%), or multidrug-resistant (MDR) P. aeruginosa (3.3%) and Acinetobacter spp. (3.2%), when compared with the entire group (1.3% for P. aeruginosa and 2.1% for Acinetobacter spp.). Among P. aeruginosa, polymyxin B resistance rates varied from 2.9% in the Asia-Pacific region to only 1.1% in Europe, Latin America and North America, while polymyxin B resistance rates ranged from 2.7% in Europe to 1.7% in North America and Latin America £ ⁄ % among Acinetobacter spp. -
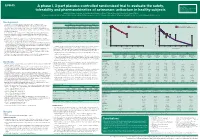
A Phase I, 3-Part Placebo-Controlled Randomised Trial to Evaluate the Safety, Tolerability and Pharmacokinetics of Aztreonam-Av
EV0643 Contactinformation: A phase I, 3-part placebo-controlled randomised trial to evaluate the safety, SeamusO’Brien AstraZenecaResearch&Development Macclesfield,Cheshire,UK tolerability and pharmacokinetics of aztreonam-avibactam in healthy subjects [email protected] Timi Edeki1, Diansong Zhou2, Frans van den Berg3, Helen Broadhurst4, William C. Holmes5, Gary Peters3, Maria Sunzel6, Seamus O’Brien4 1AstraZeneca, Wilmington, DE, USA; 2AstraZeneca, Waltham, MA, USA; 3Hammersmith Medicines Research, London, UK; 4AstraZeneca, Macclesfield, UK; 5AstraZeneca, Gaithersburg, MD, USA; 6Contractor at AstraZeneca, Wilmington, DE, USA Background Table 1.Subjects’baselinecharacteristics Figure 1. Geometricmean(A)aztreonamand(B)avibactamconcentration-timeprofilesinPartAfollowingindividualandcombinedadministrationofaztreonam2000mgandavibactam600mgby1-hIVinfusion Part A Part B Part C • Theemergenceandglobaldisseminationofmetallo-β-lactamase(MBL)-producing (A) (B) Enterobacteriaceae,includingNDM-typeandVIM-type,whichareresistanttocarbapenems, Active Placebo Active Placebo Active Placebo 100 Aztreonam 2000 mg alone (n=7) 100 Avibactam 600 mg alone (n=8) representsanurgentthreattohumanhealthforwhichfewtreatmentoptionscurrentlyexist.1, 2 (n=8) (n=4) (n=40) (n=16) (n=18) (n=6) Aztreonam-avibactam 2000-600 mg (n=7) Aztreonam-avibactam 2000-600 mg (n=7) • Aztreonam,amonobactamβ-lactam,isstabletoAmblerclassBMBLsincludingNDM-typeand Mean(SD)age,years 31(7) 34(7) 30(7) 27(5) 49(19) 51(19) VIM-type.However,bacteriathatexpressMBLsfrequentlyco-expressotherclassesofβ-lactamase -

Severe Sepsis and Septic Shock Antibiotic Guide
Stanford Health Issue Date: 05/2017 Stanford Antimicrobial Safety and Sustainability Program Severe Sepsis and Septic Shock Antibiotic Guide Table 1: Antibiotic selection options for healthcare associated and/or immunocompromised patients • Healthcare associated: intravenous therapy, wound care, or intravenous chemotherapy within the prior 30 days, residence in a nursing home or other long-term care facility, hospitalization in an acute care hospital for two or more days within the prior 90 days, attendance at a hospital or hemodialysis clinic within the prior 30 days • Immunocompromised: Receiving chemotherapy, known systemic cancer not in remission, ANC <500, severe cell-mediated immune deficiency Table 2: Antibiotic selection options for community acquired, immunocompetent patients Table 3: Antibiotic selection options for patients with simple sepsis, community acquired, immunocompetent patients requiring hospitalization. Risk Factors for Select Organisms P. aeruginosa MRSA Invasive Candidiasis VRE (and other resistant GNR) Community acquired: • Known colonization with MDROs • Central venous catheter • Liver transplant • Prior IV antibiotics within 90 day • Recent MRSA infection • Broad-spectrum antibiotics • Known colonization • Known colonization with MDROs • Known MRSA colonization • + 1 of the following risk factors: • Prolonged broad antibacterial • Skin & Skin Structure and/or IV access site: ♦ Parenteral nutrition therapy Hospital acquired: ♦ Purulence ♦ Dialysis • Prolonged profound • Prior IV antibiotics within 90 days ♦ Abscess -

Antimicrobial Stewardship Guidance
Antimicrobial Stewardship Guidance Federal Bureau of Prisons Clinical Practice Guidelines March 2013 Clinical guidelines are made available to the public for informational purposes only. The Federal Bureau of Prisons (BOP) does not warrant these guidelines for any other purpose, and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient-specific. Consult the BOP Clinical Practice Guidelines Web page to determine the date of the most recent update to this document: http://www.bop.gov/news/medresources.jsp Federal Bureau of Prisons Antimicrobial Stewardship Guidance Clinical Practice Guidelines March 2013 Table of Contents 1. Purpose ............................................................................................................................................. 3 2. Introduction ...................................................................................................................................... 3 3. Antimicrobial Stewardship in the BOP............................................................................................ 4 4. General Guidance for Diagnosis and Identifying Infection ............................................................. 5 Diagnosis of Specific Infections ........................................................................................................ 6 Upper Respiratory Infections (not otherwise specified) .............................................................................. -

209627Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209627Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review Reviewers of Multi-Disciplinary Review and Evaluation SECTIONS OFFICE/ AUTHORED/ ACKNOWLEDGED/ DISCIPLINE REVIEWER DIVISION APPROVED Mark Seggel, Ph.D. OPQ/ONDP/DNDP2 Authored: Section 4.2 Digitally signed by Mark R. Seggel -S CMC Lead DN: c=US, o=U.S. Government, ou=HHS, ou=FDA, ou=People, cn=Mark R. Signature: Mark R. Seggel -S Seggel -S, 0.9.2342.19200300.100.1.1=1300071539 Date: 2018.08.08 16:29:15 -04'00' Frederic Moulin, DVM, PhD OND/ODE3/DBRUP Authored: Section 5 Pharmacology/ Digitally signed by Frederic Moulin -S Toxicology DN: c=US, o=U.S. Government, ou=HHS, ou=FDA, ou=People, Reviewer Signature: Frederic Moulin -S 0.9.2342.19200300.100.1.1=2001708658, cn=Frederic Moulin -S Date: 2018.08.08 15:26:57 -04'00' Kimberly Hatfield, PhD OND/ODE3/DBRUP Approved: Section 5 Pharmacology/ Toxicology Digitally signed by Kimberly P. Hatfield -S DN: c=US, o=U.S. Government, ou=HHS, ou=FDA, ou=People, Team Leader Signature: Kimberly P. Hatfield -S 0.9.2342.19200300.100.1.1=1300387215, cn=Kimberly P. Hatfield -S Date: 2018.08.08 14:56:10 -04'00' Li Li, Ph.D. OCP/DCP3 Authored: Sections 6 and 17.3 Clinical Pharmacology Dig ta ly signed by Li Li S DN c=US o=U S Government ou=HHS ou=FDA ou=People Reviewer cn=Li Li S Signature: Li Li -S 0 9 2342 19200300 100 1 1=20005 08577 Date 2018 08 08 15 39 23 04'00' Doanh Tran, Ph.D. -

Antibiotic Use Guidelines for Companion Animal Practice (2Nd Edition) Iii
ii Antibiotic Use Guidelines for Companion Animal Practice (2nd edition) iii Antibiotic Use Guidelines for Companion Animal Practice, 2nd edition Publisher: Companion Animal Group, Danish Veterinary Association, Peter Bangs Vej 30, 2000 Frederiksberg Authors of the guidelines: Lisbeth Rem Jessen (University of Copenhagen) Peter Damborg (University of Copenhagen) Anette Spohr (Evidensia Faxe Animal Hospital) Sandra Goericke-Pesch (University of Veterinary Medicine, Hannover) Rebecca Langhorn (University of Copenhagen) Geoffrey Houser (University of Copenhagen) Jakob Willesen (University of Copenhagen) Mette Schjærff (University of Copenhagen) Thomas Eriksen (University of Copenhagen) Tina Møller Sørensen (University of Copenhagen) Vibeke Frøkjær Jensen (DTU-VET) Flemming Obling (Greve) Luca Guardabassi (University of Copenhagen) Reproduction of extracts from these guidelines is only permitted in accordance with the agreement between the Ministry of Education and Copy-Dan. Danish copyright law restricts all other use without written permission of the publisher. Exception is granted for short excerpts for review purposes. iv Foreword The first edition of the Antibiotic Use Guidelines for Companion Animal Practice was published in autumn of 2012. The aim of the guidelines was to prevent increased antibiotic resistance. A questionnaire circulated to Danish veterinarians in 2015 (Jessen et al., DVT 10, 2016) indicated that the guidelines were well received, and particularly that active users had followed the recommendations. Despite a positive reception and the results of this survey, the actual quantity of antibiotics used is probably a better indicator of the effect of the first guidelines. Chapter two of these updated guidelines therefore details the pattern of developments in antibiotic use, as reported in DANMAP 2016 (www.danmap.org). -

Synermox 500 Mg/125 Mg Tablets
New Zealand Data Sheet 1. PRODUCT NAME Synermox 500 mg/125 mg Tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Synermox 500 mg/125 mg Tablets: Each film‐coated tablet contains amoxicillin trihydrate equivalent to 500 mg amoxicillin, with potassium clavulanate equivalent to 125 mg clavulanic acid. Excipient(s) with known effect For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Synermox 500 mg/125 mg Tablets: White to off‐white, oval shaped film‐coated tablets, debossed with “RX713” on one side and plain on the other. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Synermox is indicated in adults and children (see sections 4.2, 4.4 and 5.1) for short term treatment of common bacterial infections such as: Upper Respiratory Tract Infections (including ENT) e.g. Tonsillitis, sinusitis, otitis media. Lower Respiratory Tract Infection e.g. acute exacerbations of chronic bronchitis, lobar and broncho‐pneumonia. Genito‐urinary Tract Infections e.g. Cystitis, urethritis, pyelonephritis, female genital infections. Skin and Soft Tissue Infections. Bone and Joint Infections e.g. Osteomyelitis. Other Infections e.g. septic abortion, puerperal sepsis, intra‐abdominal sepsis, septicaemia, peritonitis, post‐surgical infections. Synermox is indicated for prophylaxis against infection which may be associated with major surgical procedures such as those involving: Gastro‐intestinal tract Pelvic cavity 1 | Page Head and neck Cardiac Renal Joint replacement Biliary tract surgery Infections caused by amoxicillin susceptible organisms are amenable to Synermox treatment due to its amoxicillin content. Mixed infections caused by amoxicillin susceptible organisms in conjunction with Synermox‐susceptible beta‐lactamase‐producing organisms may therefore be treated by Synermox. -

Penicillin Allergy Guidance Document
Penicillin Allergy Guidance Document Key Points Background Careful evaluation of antibiotic allergy and prior tolerance history is essential to providing optimal treatment The true incidence of penicillin hypersensitivity amongst patients in the United States is less than 1% Alterations in antibiotic prescribing due to reported penicillin allergy has been shown to result in higher costs, increased risk of antibiotic resistance, and worse patient outcomes Cross-reactivity between truly penicillin allergic patients and later generation cephalosporins and/or carbapenems is rare Evaluation of Penicillin Allergy Obtain a detailed history of allergic reaction Classify the type and severity of the reaction paying particular attention to any IgE-mediated reactions (e.g., anaphylaxis, hives, angioedema, etc.) (Table 1) Evaluate prior tolerance of beta-lactam antibiotics utilizing patient interview or the electronic medical record Recommendations for Challenging Penicillin Allergic Patients See Figure 1 Follow-Up Document tolerance or intolerance in the patient’s allergy history Consider referring to allergy clinic for skin testing Created July 2017 by Macey Wolfe, PharmD; John Schoen, PharmD, BCPS; Scott Bergman, PharmD, BCPS; Sara May, MD; and Trevor Van Schooneveld, MD, FACP Disclaimer: This resource is intended for non-commercial educational and quality improvement purposes. Outside entities may utilize for these purposes, but must acknowledge the source. The guidance is intended to assist practitioners in managing a clinical situation but is not mandatory. The interprofessional group of authors have made considerable efforts to ensure the information upon which they are based is accurate and up to date. Any treatments have some inherent risk. Recommendations are meant to improve quality of patient care yet should not replace clinical judgment. -

NPTC-Formulary Brief Acne
Indian Health Service National Pharmacy and Therapeutics Committee Formulary Brief: Treatment of Acne vulgaris -January 2020- Background: The Indian Health Service (IHS) National Pharmacy and Therapeutics Committee (NPTC) reviewed the medical management of acne vulgaris at their January 2020 meeting. This review included topical therapies (retinoids, antibiotics, bactericidal and other anti-comedonal or anti-inflammatory agents) and oral therapies (antibiotics, isotretinoin, oral contraceptives, antiandrogens). Topical clindamycin, topical tretinoin, spironolactone, and combined estrogen-containing oral contraceptives are currently on the IHS National Core Formulary (NCF). Following clinical review, pharmacoeconomic evaluation and internal deliberation, the NPTC voted to ADD (1.) benzoyl peroxide (any topical formulation) and REPLACE topical clindamycin with (2.) combination clindamycin and benzoyl peroxide gel to the NCF. Discussion: Acne is the most common skin disorder in the United States (US), affecting 40-50 million persons of all ages. It can have significant sequelae from physical scarring, persistent hyperpigmentation, and psychological issues. Small studies focused on acne among American Indian/Alaska Native (AI/AN) populations suggest that the prevalence of acne is similar to other racial/ethnic groups in the US, but that the sequelae of scarring is significantly higher (55% in AI/AN vs. 3% among US white populations) and access to specialty care services is disproportionately low1. Acne is a chronic inflammatory disease of the pilosebaceous unit involving increased sebum production by sebaceous glands, hyperkeratinization of the follicle, colonization of the follicle by Propionobacterium acnes, and an inflammatory reaction. Acne is manifested with both non-inflammatory (open and closed comedones) and inflammatory lesions (papules, pustules, and nodules). Inflammatory acne is graded as mild, moderate, or severe based on the frequency of the various inflammatory lesions. -

Impact of Retreatment with an Artemisinin-Based Combination On
Muhindo Mavoko et al. Trials 2013, 14:307 http://www.trialsjournal.com/content/14/1/307 TRIALS STUDY PROTOCOL Open Access Impact of retreatment with an artemisinin-based combination on malaria incidence and its potential selection of resistant strains: study protocol for a randomized controlled clinical trial Hypolite Muhindo Mavoko1*, Carolyn Nabasumba2, Halidou Tinto3, Umberto D’Alessandro4,5, Martin Peter Grobusch6, Pascal Lutumba1 and Jean-Pierre Van Geertruyden7 Abstract Background: Artemisinin-based combination therapy is currently recommended by the World Health Organization as first-line treatment of uncomplicated malaria. Recommendations were adapted in 2010 regarding rescue treatment in case of treatment failure. Instead of quinine monotherapy, it should be combined with an antibiotic with antimalarial properties; alternatively, another artemisinin-based combination therapy may be used. However, for informing these policy changes, no clear evidence is yet available. The need to provide the policy makers with hard data on the appropriate rescue therapy is obvious. We hypothesize that the efficacy of the same artemisinin- based combination therapy used as rescue treatment is as efficacious as quinine + clindamycin or an alternative artemisinin-based combination therapy, without the risk of selecting drug resistant strains. Design: We embed a randomized, open label, three-arm clinical trial in a longitudinal cohort design following up children with uncomplicated malaria until they are malaria parasite free for 4 weeks. The study is conducted in both the Democratic Republic of Congo and Uganda and performed in three steps. In the first step, the pre-randomized controlled trial (RCT) phase, children aged 12 to 59 months with uncomplicated malaria are treated with the recommended first-line drug and constitute a cohort that is passively followed up for 42 days.