Clostridium Difficile Infection: How to Deal with the Problem DH INFORMATION RE ADER B OX
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio In
microorganisms Review The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel disease Spase Stojanov 1,2, Aleš Berlec 1,2 and Borut Štrukelj 1,2,* 1 Faculty of Pharmacy, University of Ljubljana, SI-1000 Ljubljana, Slovenia; [email protected] (S.S.); [email protected] (A.B.) 2 Department of Biotechnology, Jožef Stefan Institute, SI-1000 Ljubljana, Slovenia * Correspondence: borut.strukelj@ffa.uni-lj.si Received: 16 September 2020; Accepted: 31 October 2020; Published: 1 November 2020 Abstract: The two most important bacterial phyla in the gastrointestinal tract, Firmicutes and Bacteroidetes, have gained much attention in recent years. The Firmicutes/Bacteroidetes (F/B) ratio is widely accepted to have an important influence in maintaining normal intestinal homeostasis. Increased or decreased F/B ratio is regarded as dysbiosis, whereby the former is usually observed with obesity, and the latter with inflammatory bowel disease (IBD). Probiotics as live microorganisms can confer health benefits to the host when administered in adequate amounts. There is considerable evidence of their nutritional and immunosuppressive properties including reports that elucidate the association of probiotics with the F/B ratio, obesity, and IBD. Orally administered probiotics can contribute to the restoration of dysbiotic microbiota and to the prevention of obesity or IBD. However, as the effects of different probiotics on the F/B ratio differ, selecting the appropriate species or mixture is crucial. The most commonly tested probiotics for modifying the F/B ratio and treating obesity and IBD are from the genus Lactobacillus. In this paper, we review the effects of probiotics on the F/B ratio that lead to weight loss or immunosuppression. -

DC Console Using DC Console Application Design Software
DC Console Using DC Console Application Design Software DC Console is easy-to-use, application design software developed specifically to work in conjunction with AML’s DC Suite. Create. Distribute. Collect. Every LDX10 handheld computer comes with DC Suite, which includes seven (7) pre-developed applications for common data collection tasks. Now LDX10 users can use DC Console to modify these applications, or create their own from scratch. AML 800.648.4452 Made in USA www.amltd.com Introduction This document briefly covers how to use DC Console and the features and settings. Be sure to read this document in its entirety before attempting to use AML’s DC Console with a DC Suite compatible device. What is the difference between an “App” and a “Suite”? “Apps” are single applications running on the device used to collect and store data. In most cases, multiple apps would be utilized to handle various operations. For example, the ‘Item_Quantity’ app is one of the most widely used apps and the most direct means to take a basic inventory count, it produces a data file showing what items are in stock, the relative quantities, and requires minimal input from the mobile worker(s). Other operations will require additional input, for example, if you also need to know the specific location for each item in inventory, the ‘Item_Lot_Quantity’ app would be a better fit. Apps can be used in a variety of ways and provide the LDX10 the flexibility to handle virtually any data collection operation. “Suite” files are simply collections of individual apps. Suite files allow you to easily manage and edit multiple apps from within a single ‘store-house’ file and provide an effortless means for device deployment. -

Drug-Resistant Streptococcus Pneumoniae and Methicillin
NEWS & NOTES Conference Summary pneumoniae can vary among popula- conference sessions was that statically tions and is influenced by local pre- sound methods of data collection that Drug-resistant scribing practices and the prevalence capture valid, meaningful, and useful of resistant clones. Conference pre- data and meet the financial restric- Streptococcus senters discussed the role of surveil- tions of state budgets are indicated. pneumoniae and lance in raising awareness of the Active, population-based surveil- Methicillin- resistance problem and in monitoring lance for collecting relevant isolates is the effectiveness of prevention and considered the standard criterion. resistant control programs. National- and state- Unfortunately, this type of surveil- Staphylococcus level epidemiologists discussed the lance is labor-intensive and costly, aureus benefits of including state-level sur- making it an impractical choice for 1 veillance data with appropriate antibi- many states. The challenges of isolate Surveillance otic use programs designed to address collection, packaging and transport, The Centers for Disease Control the antibiotic prescribing practices of data collection, and analysis may and Prevention (CDC) convened a clinicians. The potential for local sur- place an unacceptable workload on conference on March 12–13, 2003, in veillance to provide information on laboratory and epidemiology person- Atlanta, Georgia, to discuss improv- the impact of a new pneumococcal nel. ing state-based surveillance of drug- vaccine for children was also exam- Epidemiologists from several state resistant Streptococcus pneumoniae ined; the vaccine has been shown to health departments that have elected (DRSP) and methicillin-resistant reduce infections caused by resistance to implement enhanced antimicrobial Staphylococcus aureus (MRSA). -

Current Trends of Enterococci in Dairy Products: a Comprehensive Review of Their Multiple Roles
foods Review Current Trends of Enterococci in Dairy Products: A Comprehensive Review of Their Multiple Roles Maria de Lurdes Enes Dapkevicius 1,2,* , Bruna Sgardioli 1,2 , Sandra P. A. Câmara 1,2, Patrícia Poeta 3,4 and Francisco Xavier Malcata 5,6,* 1 Faculty of Agricultural and Environmental Sciences, University of the Azores, 9700-042 Angra do Heroísmo, Portugal; [email protected] (B.S.); [email protected] (S.P.A.C.) 2 Institute of Agricultural and Environmental Research and Technology (IITAA), University of the Azores, 9700-042 Angra do Heroísmo, Portugal 3 Microbiology and Antibiotic Resistance Team (MicroART), Department of Veterinary Sciences, University of Trás-os-Montes and Alto Douro (UTAD), 5001-801 Vila Real, Portugal; [email protected] 4 Associated Laboratory for Green Chemistry (LAQV-REQUIMTE), University NOVA of Lisboa, 2829-516 Lisboa, Portugal 5 LEPABE—Laboratory for Process Engineering, Environment, Biotechnology and Energy, Faculty of Engineering, University of Porto, 420-465 Porto, Portugal 6 FEUP—Faculty of Engineering, University of Porto, 4200-465 Porto, Portugal * Correspondence: [email protected] (M.d.L.E.D.); [email protected] (F.X.M.) Abstract: As a genus that has evolved for resistance against adverse environmental factors and that readily exchanges genetic elements, enterococci are well adapted to the cheese environment and may reach high numbers in artisanal cheeses. Their metabolites impact cheese flavor, texture, Citation: Dapkevicius, M.d.L.E.; and rheological properties, thus contributing to the development of its typical sensorial properties. Sgardioli, B.; Câmara, S.P.A.; Poeta, P.; Due to their antimicrobial activity, enterococci modulate the cheese microbiota, stimulate autoly- Malcata, F.X. -
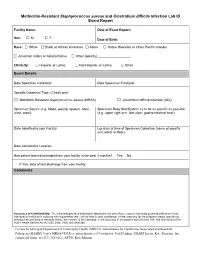
Methicillin-Resistant Staphylococcus Aureus and Clostridium Difficile Infection Lab ID Event Report
Methicillin-Resistant Staphylococcus aureus and Clostridium difficile Infection Lab ID Event Report Facility Name: Date of Event Report: Sex: M F □ □ Date of Birth: Race: □ White □ Black or African American □ Asian □ Native Hawaiian or Other Pacific Islander □ American Indian or Alaska Native □ Other [specify] __________________ Ethnicity: □ Hispanic or Latino □ Not Hispanic or Latino □ Other Event Details Date Specimen Collected: Date Specimen Finalized: Specific Organism Type: (Check one) □ Methicillin-Resistant Staphylococcus aureus (MRSA) □ Clostridium difficile Infection (CDI) Specimen Source (e.g. blood, wound, sputum, bone, Specimen Body Site/System try to be as specific as possible urine, stool): (e.g. upper right arm, foot ulcer, gastrointestinal tract): Date Admitted to your Facility: Location at time of Specimen Collection (name of specific unit, ward, or floor): Date Admitted to Location: Has patient been discharged from your facility in the past 3 months? Yes No If Yes, date of last discharge from your facility: Comments Assurance of Confidentiality: The voluntarily provided information obtained in this surveillance system that would permit identification of any individual or institution is collected with a guarantee that it will be held in strict confidence, will be used only for the purposes stated, and will not otherwise be disclosed or released without the consent of the individual, or the institution in accordance with Sections 304, 306 and 308(d) of the Public Health Service Act (42 USC 242b, 242k, and 242m(d)). For use by Michigan Department of Community Health (MDCH), Surveillance for Healthcare-Associated and Resistant Pathogens (SHARP) Unit’s MRSA/CDI Prevention Initiative (Coordinator: Gail Denkins, SHARP Intern: Kate Manton); fax completed forms to (517) 335-8263, ATTN: Kate Manton. -
Association Between Carriage of Streptococcus Pneumoniae and Staphylococcus Aureus in Children
BRIEF REPORT Association Between Carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children Gili Regev-Yochay, MD Context Widespread pneumococcal conjugate vaccination may bring about epidemio- Ron Dagan, MD logic changes in upper respiratory tract flora of children. Of particular significance may Meir Raz, MD be an interaction between Streptococcus pneumoniae and Staphylococcus aureus, in view of the recent emergence of community-acquired methicillin-resistant S aureus. Yehuda Carmeli, MD, MPH Objective To examine the prevalence and risk factors of carriage of S pneumoniae Bracha Shainberg, PhD and S aureus in the prevaccination era in young children. Estela Derazne, MSc Design, Setting, and Patients Cross-sectional surveillance study of nasopharyn- geal carriage of S pneumoniae and nasal carriage of S aureus by 790 children aged 40 Galia Rahav, MD months or younger seen at primary care clinics in central Israel during February 2002. Ethan Rubinstein, MD Main Outcome Measures Carriage rates of S pneumoniae (by serotype) and S aureus; risk factors associated with carriage of each pathogen. TREPTOCOCCUS PNEUMONIAE AND Results Among 790 children screened, 43% carried S pneumoniae and 10% car- Staphylococcus aureus are com- ried S aureus. Staphylococcus aureus carriage among S pneumoniae carriers was 6.5% mon inhabitants of the upper vs 12.9% in S pneumoniae noncarriers. Streptococcus pneumoniae carriage among respiratory tract in children and S aureus carriers was 27.5% vs 44.8% in S aureus noncarriers. Only 2.8% carried both Sare responsible for common infec- pathogens concomitantly vs 4.3% expected dual carriage (P=.03). Risk factors for tions. Carriage of S aureus and S pneu- S pneumoniae carriage (attending day care, having young siblings, and age older than moniae can result in bacterial spread and 3 months) were negatively associated with S aureus carriage. -

The Four Health Systems of the United Kingdom: How Do They Compare?
The four health systems of the United Kingdom: how do they compare? Gwyn Bevan, Marina Karanikolos, Jo Exley, Ellen Nolte, Sheelah Connolly and Nicholas Mays Source report April 2014 About this research This report is the fourth in a series dating back to 1999 which looks at how the publicly financed health care systems in the four countries of the UK have fared before and after devolution. The report was commissioned jointly by The Health Foundation and the Nuffield Trust. The research team was led by Nicholas Mays at the London School of Hygiene and Tropical Medicine. The research looks at how the four national health systems compare and how they have performed in terms of quality and productivity before and after devolution. The research also examines performance in North East England, which is acknowledged to be the region that is most comparable to Wales, Scotland and Northern Ireland in terms of socioeconomic and other indicators. This report, along with an accompanying summary report, data appendices, digital outputs and a short report on the history of devolution (to be published later in 2014), are available to download free of charge at www.nuffieldtrust.org.uk/compare-uk-health www.health.org.uk/compareUKhealth. Acknowledgements We are grateful: to government statisticians in the four countries for guidance on sources of data, highlighting problems of comparability and for checking the data we have used; for comments on the draft report from anonymous referees and from Vernon Bogdanor, Alec Morton and Laura Schang; and for guidance on national clinical audits from Nick Black and on nursing data from Jim Buchan. -

Unix (And Linux)
AWK....................................................................................................................................4 BC .....................................................................................................................................11 CHGRP .............................................................................................................................16 CHMOD.............................................................................................................................19 CHOWN ............................................................................................................................26 CP .....................................................................................................................................29 CRON................................................................................................................................34 CSH...................................................................................................................................36 CUT...................................................................................................................................71 DATE ................................................................................................................................75 DF .....................................................................................................................................79 DIFF ..................................................................................................................................84 -

5 Command Line Functions by Barbara C
ADAPS: Chapter 5. Command Line Functions 5 Command Line Functions by Barbara C. Hoopes and James F. Cornwall This chapter describes ADAPS command line functions. These are functions that are executed from the UNIX command line instead of from ADAPS menus, and that may be run manually or by automated means such as “cron” jobs. Most of these functions are NOT accessible from the ADAPS menus. These command line functions are described in detail below. 5.1 Hydra Although Hydra is available from ADAPS at the PR sub-menu, Edit Time Series Data using Hydra (TS_EDIT), it can also be started from the command line. However, to start Hydra outside of ADAPS, a DV or UV RDB file needs to be available to edit. The command is “hydra rdb_file_name.” For a complete description of using Hydra, refer to Section 4.5.2 Edit Time-Series Data using Hydra (TS_EDIT). 5.2 nwrt2rdb This command is used to output rating information in RDB format. It writes RDB files with a table containing the rating equation parameters or the rating point pairs, with all other information contained in the RDB comments. The following arguments can be used with this command: nwrt2rdb -ooutfile -zdbnum -aagency -nstation -dddid -trating_type -irating_id -e (indicates to output ratings in expanded form; it is ignored for equation ratings.) -l loctzcd (time zone code or local time code "LOC") -m (indicates multiple output files.) -r (rounding suppression) Rules • If -o is omitted, nwrt2rdb writes to stdout; AND arguments -n, -d, -t, and -i must be present. • If -o is present, no other arguments are required, and the program will use ADAPS routines to prompt for them. -

An Attribute- Grammar Compiling System Based on Yacc, Lex, and C Kurt M
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Digital Repository @ Iowa State University Computer Science Technical Reports Computer Science 12-1992 Design, Implementation, Use, and Evaluation of Ox: An Attribute- Grammar Compiling System based on Yacc, Lex, and C Kurt M. Bischoff Iowa State University Follow this and additional works at: http://lib.dr.iastate.edu/cs_techreports Part of the Programming Languages and Compilers Commons Recommended Citation Bischoff, Kurt M., "Design, Implementation, Use, and Evaluation of Ox: An Attribute- Grammar Compiling System based on Yacc, Lex, and C" (1992). Computer Science Technical Reports. 23. http://lib.dr.iastate.edu/cs_techreports/23 This Article is brought to you for free and open access by the Computer Science at Iowa State University Digital Repository. It has been accepted for inclusion in Computer Science Technical Reports by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Design, Implementation, Use, and Evaluation of Ox: An Attribute- Grammar Compiling System based on Yacc, Lex, and C Abstract Ox generalizes the function of Yacc in the way that attribute grammars generalize context-free grammars. Ordinary Yacc and Lex specifications may be augmented with definitions of synthesized and inherited attributes written in C syntax. From these specifications, Ox generates a program that builds and decorates attributed parse trees. Ox accepts a most general class of attribute grammars. The user may specify postdecoration traversals for easy ordering of side effects such as code generation. Ox handles the tedious and error-prone details of writing code for parse-tree management, so its use eases problems of security and maintainability associated with that aspect of translator development. -

Methicillin-Resistant Staphylococcus Aureus (MRSA)
Methicillin-Resistant Staphylococcus Aureus (MRSA) Over the past several decades, the incidence of resistant gram-positive organisms has risen in the United States. MRSA strains, first identified in the 1960s in England, were first observed in the U.S. in the mid 1980s.1 Resistance quickly developed, increasing from 2.4% in 1979 to 29% in 1991.2 The current prevalence for MRSA in hospitals and other facilities ranges from <10% to 65%. In 1999, MRSA accounted for more than 50% of all Staphylococcus aureus isolates within U.S. intensive care units.3, 4 The past years, however, outbreaks of MRSA have also been seen in the community setting, particularly among preschool-age children, some of whom have attended day-care centers.5, 6, 7 MRSA does not appear to be more virulent than methicillin-sensitive Staphylococcus aureus, but certainly poses a greater treatment challenge. MRSA also has been associated with higher hospital costs and mortality.8 Within a decade of its development, methicillin resistance to Staphylococcus aureus emerged.9 MRSA strains generally are now resistant to other antimicrobial classes including aminoglycosides, beta-lactams, carbapenems, cephalosporins, fluoroquinolones and macrolides.10,11 Most of the resistance was secondary to production of beta-lactamase enzymes or intrinsic resistance with alterations in penicillin-binding proteins. Staphylococcus aureus is the most frequent cause of nosocomial pneumonia and surgical- wound infections and the second most common cause of nosocomial bloodstream infections.12 Long-term care facilities (LTCFs) have developed rates of MRSA ranging from 25%-35%. MRSA rates may be higher in LTCFs if they are associated with hospitals that have higher rates.13 Transmission of MRSA generally occurs through direct or indirect contact with a reservoir. -

Methicillin Resistant Staphylococcus Aureus (MRSA)
Methicillin resistant Staphylococcus aureus (MRSA), Clostridium difficile and ESBL-producing Escherichia coli in the home and community: assessing the problem, controlling the spread An expert report commissioned by the International Scientific Forum on Home Hygiene © International Scientific Forum on Home Hygiene, 2006 2 CONTENTS ACKNOWLEDGMENTS 4 SUMMARY 5 1. INTRODUCTION – INFECTIOUS DISEASE AND HYGIENE IN THE 21ST CENTURY 7 2. THE CHAIN OF INFECTION TRANSMISSION IN THE HOME 10 3. METHICILLIN RESISTANT STAPHYLOCOCCUS AUREUS (MRSA) 11 3.1 CHARACTERISTICS OF STAPHYLOCOCCUS AUREUS AND METHICILLIN RESISTANT STAPHYLOCOCCUS AUREUS 11 3.2 HOSPITAL-ACQUIRED, HEALTHCARE ASSOCIATED AND COMMUNITY ACQUIRED MRSA 11 3.3 UNDERSTANDING THE CHAIN OF INFECTION FOR S. AUREUS AND MRSA IN THE HOME 13 3.4 WHAT ARE THE RISKS ASSOCIATED WITH S. AUREUS AND MRSA IN THE COMMUNITY? 22 4. CLOSTRIDIUM DIFFICILE 24 4.1 CHARACTERISTICS OF CLOSTRIDIUM DIFFICILE 24 4.2 HOSPITAL-ACQUIRED AND COMMUNITY- ACQUIRED C. DIFFICILE 24 4.3 UNDERSTANDING THE CHAIN OF INFECTION FOR C. DIFFICILE IN THE HOME 25 4.4 WHAT ARE THE RISKS ASSOCIATED WITH C. DIFFICILE IN THE HOME AND COMMUNITY 28 5. EXTENDED-SPECTRUM ß-LACTAMASE ESCHERICHIA COLI (ESBLS) 30 5.1 CHARACTERISTICS OF ESCHERICHIA COLI 30 5.2 HOSPITAL AND COMMUNITY-ACQUIRED ESBL-PRODUCING E. COLI INFECTIONS 31 5.3 UNDERSTANDING THE CHAIN OF INFECTION FOR E. COLI AND ESBL-PRODUCING E. COLI IN THE HOME 31 5.4 RISKS ASSOCIATED WITH ESBLS IN THE COMMUNITY 33 6. REDUCING THE RISKS OF TRANSMISSION OF METHICILLIN RESISTANT STAPHYLOCOCCUS AUREUS (MRSA), CLOSTRIDIUM DIFFICILE AND ESBL-PRODUCING ESCHERICHIA COLI IN THE HOME AND COMMUNITY - DEVELOPING A RISK-BASED APPROACH TO HOME HYGIENE 35 6.1 BREAKING THE CHAIN OF TRANSMISSION OF INFECTION IN THE HOME 35 6.2 DEVELOPING A RISK-BASED APPROACH TO HOME HYGIENE 35 6.3 INTERRUPTING THE CHAIN OF INFECTION TRANSMISSION IN THE HOME 38 7.