Nutrition Survey Report JAJARKOT DISTRICT, NEPAL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -

NCCSP Success Story 2017.Pdf
Government of Nepal Ministry of Population & Environment Nepal Climate Change Support Programme SUCCESS STORIES ON ADAPTATION FROM THE FIELD Vol. II • December 2016 Helping Local Communities Adapt to the Effects of Climate Change in Nepal Publisher Government of Nepal Ministry of Population and Environment Nepal Climate Change Support Programme Singhadurbar, Kathmandu, Nepal Phone : (977) 1 4211894 (977) 1 4200580 Email : [email protected] Web : www.nccsp.gov.np Copyright © 2016 Government of Nepal, Ministry of Population and Environment All right reserved. Information given in this publication may be reproduced, stored in retrieval system or transmitted in any form or by any means - electronic, mechanical or otherwise - by duly acknowledging the source. Citation MoPE/NCCSP. (2016). Success Stories on Adaptation from the field. Government of Nepal. Ministry of Population and Environment, Kathmandu, Nepal. Stories & Photographs Nepal Climate Change Support Programme Design & Printed at Golden Egg Creation Pvt. Ltd. Nayabazar, Kathmandu. [email protected] Government of Nepal Ministry of Population & Environment Nepal Climate Change Support Programme SUCCESS STORIES ON ADAPTATION FROM THE FIELD Vol. II • December 2016 Foreword Nepal Climate Change Support Programme (NCCSP) is the first significant initiative by the Government of Nepal in the sector of climate change adaptation. Ministry of Population and Environment (MoPE) is a lead agency implementing the NCCSP in close collaboration with the Ministry of Federal Affairs and Local Development (MoFALD) and the Alternative Energy Promotion Center (AEPC). The overall goal of this programme is to ensure that Nepal’s poorest and most vulnerable people are able to adapt well to the negative impacts of climate change. -
Decentralized Rural Infrastructure and Livelihood Project- Additional Financing
Environmental Assessment Document I nitial Environmental Examination Loan Number: 2796 and Grant Number: 0267 NEP october 2012 Nepal: Decentralized Rural Infrastructure and Livelihood Project- Additional Financing Thalaha-Batu le-Au latari Road (Section of Dhungil-Rokayagaon road) Subproject , Jajarkot Prepared by the Government of Nepal The Environmental Assessment is a document of the borrower, The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or statf, and may be preliminary in narure. Decentralized Rural Infrastructure and Livelihood Project-Additional Financing (DRILP-AF) Initial Environmental Examination (IEE) of Thalaha-Batule-Aulatari Road (Section of Dhungil-Rokayagaon road) Subproject Submitted to: Ministry Of Federal Affairs and Local Development Government of Nepal Proponent: District Development Committee, Jajarkot Khalanga, October, 2012 1 Table of Contents Table of Contents ................................................................................................................... i List of Tables ......................................................................................................................... ii List of Figures ........................................................................................................................ ii Appendixes ........................................................................................................................... ii ABBREVIATIONS ............................................................................................................... -
Pdf | 268.57 Kb
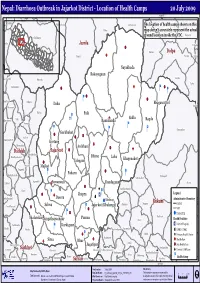
Nepal: Diarrhoea Outbreak in Jajarkot District - Location of Health Camps 20 July 2009 82°30'0"E Jubika Ramchuli Pakha Dah Malikathota Guthichaur The location of health camps shown on this Haku map doesn't accuratelyRIMI represent the actual ground location inside the VDC. Kaigaun Chilkhaya Gela Jumla &! Pahada Kalikot Sarmi Dolpa Tamti GF Narku Likhu Nayakbada Rokayagaun Kalika Kasikandh Odanku Laha GF ! Baluwatar &! Ý & Ý &! &! Raniban Odhari Ý Bhagawatitol Daha Suhun Bhawani Kalika Paik ; &! Sakla Kharigera Toli Ý Ramidanda Ragda Nomule Ý Ý Ý Ý Gautamkot &! Garkhakot ! Salleri &! & Narayan N.P. Kortang GF Chauratha Archhani &! GF Dailekh Jajarkot &! Moheltolee Dhime Bindhyabasini Laha Khagenakot &! Talegaun Room Majkot Pagnath ! Padaru & BadaBhairab Ý Ý Syalagadi AathbisKot Jaganath Lakuri &!Suwanauli Dandagaun Sisne ! & h AathbisDanda Katti ! Jhapra Æ Ý Legend & Ý GF × q DadaParajul Dasera Khalanga Administrative Boundary ! Rukum Jang Ghetma Magma District AwalParajul ! Salma Jajarkot (Khalanga) & Ý &! VDC Ý &! ! District HQ Thalarekar &! Punma Baflikot Jungathapachaur Duli Health Facilities Æ Pwang Lalikanda Karkigaun Pipalq District Hospital Piladi Matela Ý PurtimKanda Garayala × DPHO / DHO GF Ý Jhula ; Primary Health Centre Ratu GF Kotjahari GF GF Sima Bhur Health Post Simli ! AWALCHING Jagatipur & SubPokhara Health Post Rangsi Surkhet Syalapakha Garpan Ghoreta Chaurjahari( (Bijayashwari) h District Cold Room Kholagaun MusikotKhalanga( Ranibas Arma Chhiwang Kanda Pamka Bame Health Camp Rajena Agragaun Suikot Sankha Sobha Satakhani Kafalkot Salyan Kalagaun Nuwakot Pyaugha Bhalakacha Ý 82°30'0"E Produced on: 2 July 2009 Disclaimers: Map Produced by OCHA, Nepal Map Doc Name: D_Outbreak_Jajarkot_3W_A4_21072009_v01 The boundaries and names shown and the 02 4 Km Data Source(s): Data are collected from DPHO, UN Agencies and I/NGOs Web Resources: http://www.un.org.np designations used on this map do not imply official I Boundaries - Department of Survey, Nepal Projection/Datum: Geographic/Everest 1830 endorsement or acceptance by the United Nations.. -
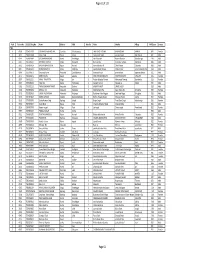
TSLC PMT Result
Page 62 of 132 Rank Token No SLC/SEE Reg No Name District Palika WardNo Father Mother Village PMTScore Gender TSLC 1 42060 7574O15075 SOBHA BOHARA BOHARA Darchula Rithachaupata 3 HARI SINGH BOHARA BIMA BOHARA AMKUR 890.1 Female 2 39231 7569013048 Sanju Singh Bajura Gotree 9 Gyanendra Singh Jansara Singh Manikanda 902.7 Male 3 40574 7559004049 LOGAJAN BHANDARI Humla ShreeNagar 1 Hari Bhandari Amani Bhandari Bhandari gau 907 Male 4 40374 6560016016 DHANRAJ TAMATA Mugu Dhainakot 8 Bali Tamata Puni kala Tamata Dalitbada 908.2 Male 5 36515 7569004014 BHUVAN BAHADUR BK Bajura Martadi 3 Karna bahadur bk Dhauli lawar Chaurata 908.5 Male 6 43877 6960005019 NANDA SINGH B K Mugu Kotdanda 9 Jaya bahadur tiruwa Muga tiruwa Luee kotdanda mugu 910.4 Male 7 40945 7535076072 Saroj raut kurmi Rautahat GarudaBairiya 7 biswanath raut pramila devi pipariya dostiya 911.3 Male 8 42712 7569023079 NISHA BUDHa Bajura Sappata 6 GAN BAHADUR BUDHA AABHARI BUDHA CHUDARI 911.4 Female 9 35970 7260012119 RAMU TAMATATA Mugu Seri 5 Padam Bahadur Tamata Manamata Tamata Bamkanda 912.6 Female 10 36673 7375025003 Akbar Od Baitadi Pancheswor 3 Ganesh ram od Kalawati od Kalauti 915.4 Male 11 40529 7335011133 PRAMOD KUMAR PANDIT Rautahat Dharhari 5 MISHRI PANDIT URMILA DEVI 915.8 Male 12 42683 7525055002 BIMALA RAI Nuwakot Madanpur 4 Man Bahadur Rai Gauri Maya Rai Ghodghad 915.9 Female 13 42758 7525055016 SABIN AALE MAGAR Nuwakot Madanpur 4 Raj Kumar Aale Magqar Devi Aale Magar Ghodghad 915.9 Male 14 42459 7217094014 SOBHA DHAKAL Dolakha GhangSukathokar 2 Bishnu Prasad Dhakal -
Climate Nepal ' Eeomn Predicaments Development S
VULNERABILITY Through the Eyes of the VULNERABILITY VULNERABLE Through the Eyes of the VULNERABLE Climate Change Induced Uncertainties and Nepal ' s Development Predicaments Climate Change Induced Uncertainties and Nepal's Development Predicaments Nepal Climate Vulnerability Study Team (NCVST) October 2009 VULNERABILITY Through the Eyes of the VULNERABLE Climate Change Induced Uncertainties and Nepal's Development Predicaments Climate ChangeNepal Climate Vulnerability Induced Study Team (NCVST) October 2009 Uncertainties and Nepal's Development Predicaments NEPAL CLIMATE VULNERABILITY STUDY © Copyright, ISET-N and ISET 2009 Reasonable amount of text from this report can be quoted provided the source is acknowledged and ISET-N and ISET informed. TEAM (NCVST) ISBN: 978-9937-2-1828-3 Published by Institute for Social and Environmental Transition-Nepal (ISET-N) ISET-Nepal GPO Box: 3971; Tel: 977-1-4720667, 4720744; Fax: 977-1-5542354 E-mail: [email protected]; and Ajaya Dixit Institute for Social and Environmental Transition (ISET) 948 North Dipak Gyawali Street, Ste. 9, Boulder, CO 80304, USA Tel: 720-564-0650, Fax: 720-564-0653, www.i-s-e-t.org Madhukar Upadhya Anil Pokhrel 2nd reprint with some improvements and corrections. Disclaimer This report was prepared for the Kathmandu to Copenhagen 2009: The ISET Way Forward for Nepal conference in Kathmandu on 2nd September 2009. Its primary purpose is to bring the voices from the grassroots to Fawad Khan the fore, to assemble together the knowns and the unknowns on Dr Sarah Opitz-Stapleton climate change in the Nepal Himalaya, and to explore potential directions for future research as well as adaptive development activities. -
ANNUAL PROGRESS REPORT (Fiscal Year 2017/18)
LoanLoan No.: No.: 796−NP 796−NP GrantGrant No.: No.: DSF−8050−NP DSF−8050−NP Government of Nepal Ministry of Agriculture and Livestock Development High Value Agriculture Project in Hill and Mountain Areas (HVAP) ANNUAL PROGRESS REPORT (Fiscal Year 2017/18) Implementing Partners Connecting People’s Capacities Project Management Unit (PMU) Birendranagar, Surkhet, Nepal Phone No.: 977-83-520038, Fax No.: 977-83-525403 Email: [email protected] Website: www.hvap.gov.np September 2018 September, £017 Government of Nepal Ministry of Agriculture and Livestock Development ANNUAL PROGRESS REPORT 2017/18 (16 July 2017 to 17 July 2018) HIGH VALUE AGRICULTURE PROJECT IN HILL AND MOUNTAIN AREAS (HVAP) Project Management Unit Birendranagar, Surkhet, Nepal Phone No.:977-83-520038, Fax No.:977-83-525403 Email: [email protected] www.hvap.gov.np September, 2018 (Annual Progress Report 2017/18) September 2018 Project at a Glance Country Nepal Title of the Report Annual Progress Report 2017/18 High Value Agriculture Project In Hill and Mountain Areas Project Title (HVAP) Project Number Loan No.: 796-NP; Grant No.: DSF-8050-NP Donor Agency International Fund for Agricultural Development (IFAD) Ministry of Agriculture and LIvestock Development, Executing Agency Government of Nepal Partners SNV-Nepal and Agro Enterprise Centre Location of the Project 6 Districts from Province 6 and 1 District from Privince 7 Fiscal Year/Reporting Year 2017/18 Reporting Period 16July 2017 to 17July 2018 Year of Implementation 8th Year Total Project Budget (US$) 18.87 Million Date of Loan Effectiveness 5 July 2010 Date of Project Start 6 Feb 2011 Project Duration 7.5 Years Date of Project Completion 30 September 2018 Date of Financing Closing 31 March 2019 Budget of FY 2016/17 Year NRs. -
Decentralized Rural Infrastructure and Livelihoods Project
Environmental Assessment Report Initial Environmental Examination Project Number: 30232 July 2008 NEP: Decentralized Rural Infrastructure and Livelihoods Project Prepared by [Author(s)] [Firm] [City, Country] Prepared by District Development Committee, Jajarkot for the Asian Development Bank (ADB). Prepared for [Executing Agency] [Implementing Agency] The views expressed herein are those of the consultant and do not necessarily represent those of ADB’s The initial environmental examination is a document of the borrower. The views expressed herein do not members, Board of Directors, Management, or staff, and may be preliminary in nature. necessarily represent those of ADB’s Board of Directors, Management, or staff, and may be preliminary in nature. TABLE OF CONTENTS ABBREVIATIONS i EXECUTIVE SUMMARY (NEPALI) iii EXECUTIVE SUMMARY vi 1.0 INTRODUCTION 1 1.1 Background 1 1.2 Relevancy of the proposal 1 1.3 Name and address of the proponent 2 1.4 Description of the proposal 2 1.5 Salient features of the proposal 5 1.6 Construction approach 6 1.7 Purpose and objectives of IEE 6 1.8 Methodology adopted 7 2.0 REVIEW OF RELEVANT ACTS, REGULATIONS AND GUIDELINES 11 3.0 EXISTING ENVIRONMENTAL CONDITION 15 3.1 Physical environment 15 3.2 Biological environment 22 3.3 Socio-economic and cultural environment 26 4.0 PROJECT ALTERNATIVES 31 4.1 No project alternative 31 4.2 Project alternatives 31 4.3 Alternative Route 32 4.4 Alternative design and construction approach 32 4.5 Alternative Construction schedule 33 4.6 Alternative resources 33 5.0 IDENTIFICATION -

Karnali Province Tourism Master Plan 2076/77 - 2085/86 BS (2020/21-2029/30)
Karnali Province Ministry of Industry, Tourism, Forest and Environment Surkhet, Nepal Karnali Province Tourism Master Plan 2076/77 - 2085/86 BS (2020/21-2029/30) January 2020 i Karnali Province Ministry of Industry, Tourism, Forest and Environment (MoITFE) Surkhet, Nepal, 2020 KARNALI PROVINCE TOURISM MASTER PLAN 2076/77 - 2085/086 BS (2020/21-2029/30) Technical Assistance WWF Nepal, Kathmandu Office, Nepal Consulting Services Mountain Heritage, Kathmandu, Nepal Advisors Hon. Nanda Singh Budha : Minister; Ministry of Industry, Tourism, Forest and Environment/Karnali Province Dr. Krishna Prasad Acharya : Secretary; Ministry of Industry, Tourism, Forest and Environment/Karnali Province Mr. Dhirendra Pradhan : Ex- Secretary; Ministry of Industry, Tourism, Forest and Environment/Karnali Province Dr. Ghana Shyam Gurung : Country Representative, WWF Nepal Mr. Santosh Mani Nepal : Senior Director, WWF Nepal Focal Persons Ms. Anju Chaudhary : MoITFE/Karnali Province Mr. Eak Raj Sigdel : WWF Nepal Planning Expert Team Members Ms. Lisa Choegyel : Senior Tourism Marketing Advisor Mr. Ram Chandra Sedai : Team Leader/Tourism Expert Dr. Roshan Sherchan : Biodiversity Expert Mr. Jailab K. Rai : Socio-Economist and Gender Specialist Er. Krishna Gautam : Environmental Engineer Mr. Harihar Neupane : Institutional and Governance Expert Mr. Yuba Raj Lama : Culture Expert Cover Photo Credit Ram C.Sedai (All, except mentioned as other's), Bharat Bandhu Thapa (Halji Gomba & Ribo Bumpa Gomba), Chhewang N. Lama (Saipal Base Camp), Dr. Deependra Rokaya (Kailash View Dwar), www.welcometorukum.org (Kham Magar), Google Search (Snow Leopard, Musk Deer, Patal Waterfall, Red Panda). ii ACKNOWLEDGEMENTS The Consultant Team would like to acknowledge following institutions and individuals for their meaningful contribution towards the formulation of Karnali Province Tourism Development Master Plan. -

Saath-Saath Project
Saath-Saath Project Saath-Saath Project THIRD ANNUAL REPORT August 2013 – July 2014 September 2014 0 Submitted by Saath-Saath Project Gopal Bhawan, Anamika Galli Baluwatar – 4, Kathmandu Nepal T: +977-1-4437173 F: +977-1-4417475 E: [email protected] FHI 360 Nepal USAID Cooperative Agreement # AID-367-A-11-00005 USAID/Nepal Country Assistance Objective Intermediate Result 1 & 4 1 Table of Contents List of Acronyms .................................................................................................................................................i Executive Summary ............................................................................................................................................ 1 I. Introduction ........................................................................................................................................... 4 II. Program Management ........................................................................................................................... 6 III. Technical Program Elements (Program by Outputs) .............................................................................. 6 Outcome 1: Decreased HIV prevalence among selected MARPs ...................................................................... 6 Outcome 2: Increased use of Family Planning (FP) services among MARPs ................................................... 9 Outcome 3: Increased GON capacity to plan, commission and use SI ............................................................ 14 Outcome -

Facility Based Assessment for Reproductive Health Commodities and Services
Facility Based Assessment for Reproductive Health Commodities and Services FINAL REPORT United Nations Population Fund (UNFPA) Shanta Bhawan Road, Jhamsikhel Lalitpur, Nepal Submitted By Nepal Development Research Institute Shree Durbar Tole, Pulchowk, Lalitpur, Nepal Submission date: 16th March 2015 i This report is a product of research on "Facility Based Assessment for Reproductive Health Commodities and Services “carried out by Nepal Development Research Institute with the financial support of United Nations Population Fund (UNFPA) from October 2014 to January 2015 Study Team • Dr. Basu Dev Pandey, Team Leader • Prof. Naveen Shrestha, Senior Consultant Expert • Dr. Jaya Kumar Gurung, Project Coordinator • Dr. Rabita Mulmi, Field Survey Coordinator • Ms. Saruna Ghimire, Consultant Expert • Ms. Sona Shakya , Senior Research Associate Report By: Nepal Development Research Institute Shree Durbar Tole, Pulchowk, Lalitpur www.ndri.org.np ii Acknowledgement It is a great pleasure for Nepal Development Research Institute (NDRI) to accomplish this research in collaboration with concern departments of Government of Nepal and UNFPA/Nepal. We thank UNFPA for entrusting NDRI and making congenial environment for this research work. It's immense pleasure to acknowledge the representatives of Nepal Government's agencies particularly Dr. Senendra Raj Upreti, Director General , Department of Health services, Dr. Bhim Singh Tinkari, Director of Logistic Management Division (LMD), Dr. Pushpa Chaudhari, Director, Family Health Division (FHD), Bhogendra Raj Dotel, Senior Public Health Administrator, Mr. Gyan Bahadur BC, Planning Officer (LMD), Krishna Ghimire, Joint Secretary (LMD), Upendra Dhungana (LMD) for their invaluable cooperation into various ways; valuable inputs in the inception phase of project, important contribution in training to field researchers, arranging the district and regional level health facilities for their cooperation, and providing suggestions in the draft report. -

January 13, 2014 0900 Hrs. Nepal Time Deadline for Pre
Issuance Date: November 20, 2013 Closing Date and Time: January 13, 2014 0900 Hrs. Nepal time Deadline for Pre-Proposal Conference Registration: December 9, 2013 0900 Hrs Nepal time MANDATORY Pre-proposal Conference: December 13, 2013 Deadline for Questions: December 23, 2013 1600 Hrs. Nepal Oral Presentations, if required TBDtime Subject: Request for Proposals (RFP) No. SOL-367-14-000001 USAID/Nepal Business Literacy Program Dear Potential Offerors: The United States Government, represented by the U.S. Agency for International Development (USAID), is seeking proposals from qualified local Nepali organizations interested in providing the services as described in the attached solicitation. The justification for the use of other than full and open competition which limits competition to the local Nepali market for this contract has been approved by the Contracting Officer. To be considered a local Nepali organization, an Offeror must: (1) be legally organized under the laws of Nepal; (2) have as its principal place of business or operations in Nepal; and (3) either is (A) majority owned by individuals who are citizens or lawful permanent residents of Nepal; or (B) managed by a governing body the majority of whom are citizens or lawful permanent residents of Nepal. “Majority owned" and "managed by" include, without limitation, beneficiary interests and the power, either directly or indirectly, whether exercised or exercisable, to control the election, appointment, or tenure of the organization's managers or a majority of the organization's governing body by any means. USAID plans to award a Firm Fixed Price (FFP) Type Contract for a performance period of three years, subject to the availability of funds.