Facility Based Assessment for Reproductive Health Commodities and Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Food Security Bulletin 29
Nepal Food Security Bulletin Issue 29, October 2010 The focus of this edition is on the Mid and Far Western Hill and Mountain region Situation summary Figure 1. Percentage of population food insecure* 26% This Food Security Bulletin covers the period July-September and is focused on the Mid and Far Western Hill and Mountain (MFWHM) 24% region (typically the most food insecure region of the country). 22% July – August is an agricultural lean period in Nepal and typically a season of increased food insecurity. In addition, flooding and 20% landslides caused by monsoon regularly block transportation routes and result in localised crop losses. 18 % During the 2010 monsoon 1,600 families were reportedly 16 % displaced due to flooding, the Karnali Highway and other trade 14 % routes were blocked by landslides and significant crop losses were Oct -Dec Jan-M ar Apr-Jun Jul-Sep Oct -Dec Jan-M ar Apr-Jun Jul-Sep reported in Kanchanpur, Dadeldhura, western Surkhet and south- 08 09 09 09 09 10 10 10 eastern Udayapur. NeKSAP District Food Security Networks in MFWHM districts Rural Nepal Mid-Far-Western Hills&Mountains identified 163 VDCs in 12 districts that are highly food insecure. Forty-four percent of the population in Humla and Bajura are reportedly facing a high level of food insecurity. Other districts with households that are facing a high level of food insecurity are Mugu, Kalikot, Rukum, Surkhet, Achham, Doti, Bajhang, Baitadi, Dadeldhura and Darchula. These households have both very limited food stocks and limited financial resources to purchase food. Most households are coping by reducing consumption, borrowing money or food and selling assets. -

Feasibility Study of Kailash Sacred Landscape
Kailash Sacred Landscape Conservation Initiative Feasability Assessment Report - Nepal Central Department of Botany Tribhuvan University, Kirtipur, Nepal June 2010 Contributors, Advisors, Consultants Core group contributors • Chaudhary, Ram P., Professor, Central Department of Botany, Tribhuvan University; National Coordinator, KSLCI-Nepal • Shrestha, Krishna K., Head, Central Department of Botany • Jha, Pramod K., Professor, Central Department of Botany • Bhatta, Kuber P., Consultant, Kailash Sacred Landscape Project, Nepal Contributors • Acharya, M., Department of Forest, Ministry of Forests and Soil Conservation (MFSC) • Bajracharya, B., International Centre for Integrated Mountain Development (ICIMOD) • Basnet, G., Independent Consultant, Environmental Anthropologist • Basnet, T., Tribhuvan University • Belbase, N., Legal expert • Bhatta, S., Department of National Park and Wildlife Conservation • Bhusal, Y. R. Secretary, Ministry of Forest and Soil Conservation • Das, A. N., Ministry of Forest and Soil Conservation • Ghimire, S. K., Tribhuvan University • Joshi, S. P., Ministry of Forest and Soil Conservation • Khanal, S., Independent Contributor • Maharjan, R., Department of Forest • Paudel, K. C., Department of Plant Resources • Rajbhandari, K.R., Expert, Plant Biodiversity • Rimal, S., Ministry of Forest and Soil Conservation • Sah, R.N., Department of Forest • Sharma, K., Department of Hydrology • Shrestha, S. M., Department of Forest • Siwakoti, M., Tribhuvan University • Upadhyaya, M.P., National Agricultural Research Council -

MISP) of Reproductive Health Services for Internally Displaced Persons in Kathmandu and Sindhupalchowk Districts, Nepal
Women’s Refugee Commission Research. Rethink. Resolve. Evaluation of the Minimum Initial Services Package (MISP) of Reproductive Health Services for Internally Displaced Persons in Kathmandu and Sindhupalchowk Districts, Nepal Literature Review Focus Group Discussions Key Informant Interviews Health Facility Assessments May 2016 Research. Rethink. Resolve. The Women’s Refugee Commission improves the lives and protects the rights of women, children, and youth displaced by conflict and crisis. We research their needs, identify solutions, and advocate for programs and policies to strengthen their resilience and drive change in humanitarian practice. Acknowledgments This evaluation could not have been undertaken without the support of the Family Health Division (FHD), Department of Health Services (DoHS) Nepal the United Nations Population Fund Nepal (UNFPA), International Planned Parenthood Foun- dation (IPPF), and the Family Planning Association of Nepal (FPAN). We greatly appreciate the time taken by Dr. Shilu Aryal, FHD and Dr. Shilu Adhikari UNFPA in particular for supporting the Internal Review Board submission to the Nepal Research Council; hosting the Nepal RH sub-cluster MISP evaluation debriefing and support throughout the evaluation. We also deeply appreciate the time of Mr. Hari Kari UNFPA for scheduling and accompanying the evaluation team on key informant interviews; Dr. Nirmal Rimal, UNFPA for scheduling health facility assessments, and the overall support of UNFPA Country Director, Ms. Giulia Vallese. We also thank the IPPF for supporting administration and logistics for the evaluation including Ms. Nimisha Goswami and Mr. Rajrattan Lokhande, and at FPAN Mr. Subhash Shreshtha and Mr. Prabin Khadka. Thanks to Research Input and Development Action (RIDA) for conducting the focus group discussions; and FPAN for coordinating, scheduling, logistics, and overseeing recruitment of participants. -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -

Environmental Assessment Document
Social Monitoring Report Semi Annual Social Monitoring Report July to December 2020 Project Number: 44219-014 Loan/ Grant Number: 3139/0397 (NEP) March 2021 Nepal: South Asia Subregional Economic Cooperation Power System Enhancement Project Prepared by the Nepal Electricity Authority (NEA) for Asian Development Bank. This Social Monitoring Report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. 8th Semiannual Social Monitoring Report July-December 2020 ACRONYMS AND ABBREVIATIONS ADB Asian Development Bank AP Angle Point APs Affected Peoples CDC Compensation Determination Committee CDO Chief District Officer CF Community Forest CFUGs Community Forest User Groups CSR Corporate Social Responsibility CTEVT Council for Technical Education and Vocational Training DKTLP Dana-Kushma 220kV Transmission Line Project EIB European Investment Bank EM Entitlement Matrix ESMU Environmental and Social Management Unit ESSD Environment and Social Studies Department GoN Government of Nepal GRC Grievance Redress Committee ha hectare HH Household IEE Initial Environmental Examination IP Indigenous People IPP Indigenous People’s Plan IR Involuntary -

Krishna Bahadur Shahi
CV-Krishna Krishna Bahadur Shahi Born: 29 May 1983 Address: Tilagupha Municipality-6, Kalikot, Nepal Contact No.: Mobile: 9848305151/9858320505 Email: [email protected]/[email protected] Academic Qualifications: 2014 M. A. in Sociology, Faculty of Humanities and Social Science, Birendranagar Multiple Campus Surkhet (T.U.) 2005 Bachelor in Education, Education Campus Surkhet (T.U.) 2002 Intermediate (+2) in Education, Birendranagar Multiple Campus, Surkhet (HSEB) 2000 S.L.C., Satya Devi H.S. School Jubitha, Kalikot Major Trainings Received: 2nd to 11th Sep. 2006 Professional Report Writing and Proposal Writing by SNV/Nepal 13th to 19th Oct. 2006 Social Mobilization TOT by PAF, Nepal 2008 Start and Improve Your Business SIYB-Level-1 International Labor Organization (ILO)s Two week Training of Trainers' Program by MEDEP, Nepal 21st to 23rd Feb. 2009 Institutional Development (TOT) by PAF, Nepal 25th June to 9th July 2009 Development of Trainers (DOT) by UNICEF/VDRC, Nepal 23rd Aug. to 2nd Sep. 2009 Professional Arc GIS Training by Sea Gate Company, Lalitpur 15th to 22nd Sep. 2009 Tourism Based Micro-Enterprises Development Training by MEDEP, Nepal 11th to 15th Nov. 2009 Transparency, Accountability and Good Governance by SNV/nepal 28th Nov. to 2nd Dec. 2009 Appreciate Inquiry Training by PAF, Nepal 29th Aug. to 2nd Sep. 2013 Value Chain Based GESI (TOT) by HVAP, Surkhet 25th Oct. to 1st Nov. 2013 Cooperative Development, Procurement System and Business Plan Preparation Training by PCU/WUPAP 30th May to 3rd June 2014 Participatory Monitoring, -
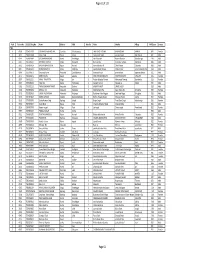
VBST Short List
1 आिेदकको दर्ा ा न륍बर नागररकर्ा न륍बर नाम थायी जि쥍ला गा.वि.स. बािुको नाम ईभेꅍट ID 10002 2632 SUMAN BHATTARAI KATHMANDU KATHMANDU M.N.P. KEDAR PRASAD BHATTARAI 136880 10003 28733 KABIN PRAJAPATI BHAKTAPUR BHAKTAPUR N.P. SITA RAM PRAJAPATI 136882 10008 271060/7240/5583 SUDESH MANANDHAR KATHMANDU KATHMANDU M.N.P. SHREE KRISHNA MANANDHAR 136890 10011 9135 SAMERRR NAKARMI KATHMANDU KATHMANDU M.N.P. BASANTA KUMAR NAKARMI 136943 10014 407/11592 NANI MAYA BASNET DOLAKHA BHIMESWOR N.P. SHREE YAGA BAHADUR BASNET136951 10015 62032/450 USHA ADHIJARI KAVRE PANCHKHAL BHOLA NATH ADHIKARI 136952 10017 411001/71853 MANASH THAPA GULMI TAMGHAS KASHER BAHADUR THAPA 136954 10018 44874 RAJ KUMAR LAMICHHANE PARBAT TILAHAR KRISHNA BAHADUR LAMICHHANE136957 10021 711034/173 KESHAB RAJ BHATTA BAJHANG BANJH JANAK LAL BHATTA 136964 10023 1581 MANDEEP SHRESTHA SIRAHA SIRAHA N.P. KUMAR MAN SHRESTHA 136969 2 आिेदकको दर्ा ा न륍बर नागररकर्ा न륍बर नाम थायी जि쥍ला गा.वि.स. बािुको नाम ईभेꅍट ID 10024 283027/3 SHREE KRISHNA GHARTI LALITPUR GODAWARI DURGA BAHADUR GHARTI 136971 10025 60-01-71-00189 CHANDRA KAMI JUMLA PATARASI JAYA LAL KAMI 136974 10026 151086/205 PRABIN YADAV DHANUSHA MARCHAIJHITAKAIYA JAYA NARAYAN YADAV 136976 10030 1012/81328 SABINA NAGARKOTI KATHMANDU DAANCHHI HARI KRISHNA NAGARKOTI 136984 10032 1039/16713 BIRENDRA PRASAD GUPTABARA KARAIYA SAMBHU SHA KANU 136988 10033 28-01-71-05846 SURESH JOSHI LALITPUR LALITPUR U.M.N.P. RAJU JOSHI 136990 10034 331071/6889 BIJAYA PRASAD YADAV BARA RAUWAHI RAM YAKWAL PRASAD YADAV 136993 10036 071024/932 DIPENDRA BHUJEL DHANKUTA TANKHUWA LOCHAN BAHADUR BHUJEL 136996 10037 28-01-067-01720 SABIN K.C. -
TSLC PMT Result
Page 62 of 132 Rank Token No SLC/SEE Reg No Name District Palika WardNo Father Mother Village PMTScore Gender TSLC 1 42060 7574O15075 SOBHA BOHARA BOHARA Darchula Rithachaupata 3 HARI SINGH BOHARA BIMA BOHARA AMKUR 890.1 Female 2 39231 7569013048 Sanju Singh Bajura Gotree 9 Gyanendra Singh Jansara Singh Manikanda 902.7 Male 3 40574 7559004049 LOGAJAN BHANDARI Humla ShreeNagar 1 Hari Bhandari Amani Bhandari Bhandari gau 907 Male 4 40374 6560016016 DHANRAJ TAMATA Mugu Dhainakot 8 Bali Tamata Puni kala Tamata Dalitbada 908.2 Male 5 36515 7569004014 BHUVAN BAHADUR BK Bajura Martadi 3 Karna bahadur bk Dhauli lawar Chaurata 908.5 Male 6 43877 6960005019 NANDA SINGH B K Mugu Kotdanda 9 Jaya bahadur tiruwa Muga tiruwa Luee kotdanda mugu 910.4 Male 7 40945 7535076072 Saroj raut kurmi Rautahat GarudaBairiya 7 biswanath raut pramila devi pipariya dostiya 911.3 Male 8 42712 7569023079 NISHA BUDHa Bajura Sappata 6 GAN BAHADUR BUDHA AABHARI BUDHA CHUDARI 911.4 Female 9 35970 7260012119 RAMU TAMATATA Mugu Seri 5 Padam Bahadur Tamata Manamata Tamata Bamkanda 912.6 Female 10 36673 7375025003 Akbar Od Baitadi Pancheswor 3 Ganesh ram od Kalawati od Kalauti 915.4 Male 11 40529 7335011133 PRAMOD KUMAR PANDIT Rautahat Dharhari 5 MISHRI PANDIT URMILA DEVI 915.8 Male 12 42683 7525055002 BIMALA RAI Nuwakot Madanpur 4 Man Bahadur Rai Gauri Maya Rai Ghodghad 915.9 Female 13 42758 7525055016 SABIN AALE MAGAR Nuwakot Madanpur 4 Raj Kumar Aale Magqar Devi Aale Magar Ghodghad 915.9 Male 14 42459 7217094014 SOBHA DHAKAL Dolakha GhangSukathokar 2 Bishnu Prasad Dhakal -

SASEC) Power System Expansion Project (SPEP
Environmental Impact Assessment February 2014 NEP: South Asia Subregional Economic Cooperation (SASEC) Power System Expansion Project (SPEP) Prepared by Nepal Electricity Authority for the Asian Development Bank. This environmental impact assessment is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” section of this website. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Asian Development Bank Nepal: South Asia Subregional Economic Cooperation (SASEC) Power System Expansion Project (SPEP) On-grid Components ENVIRONMENTAL IMPACT ASSESSMENT Draft – February 2014 i ADB TA 8272-NEP working draft – February 2014 TABLE OF CONTENTS Section Page 1 Executive Summary 1 2 Policy, Legal, and Administrative Framework 4 3 Description of the Project 19 4 Description of the Environment 28 Anticipated Environmental Impacts and Mitigation 5 96 Measures Information Disclosure, Consultation, and 6 112 Participation 7 Environmental Management Program 115 8 Conclusions and Recommendations 12 8 Appendices 1 Important Flora and Fauna 13 7 2 Habitat Maps 15 9 3 Summary of Offsetting Activities 16 9 Routing Maps in Annapurna Conservation Area -

NEPAL: Sindhupalchok District - Technical Assistance: Short Training Coverage by VDC (As of 25 April 2017) HRRP
NEPAL: Sindhupalchok District - Technical Assistance: Short Training Coverage by VDC (as of 25 April 2017) HRRP No. of Trained Masons through DUDBC Curriculum by POs Legend Rasuwa JICA/TCN 1459 NRCS 866 SABAL/UCEP-N 474 District Boundary CARE-N/CSRC 452 VDC/Municipality Boundary SCI/TUKI CHINA 428 ARSOW-ASF 366 No. of masons trained PLAN 239 OXFAM/MANK/Janahit 217 549 CA 192 201 - 400 UNDP 184 101 - 200 MC/CDECF 179 CARITAS-N 160 Upto 100 PWJ/ISAP 121 No masons trained BC/ARSOW 83 HELP/TUKI 66 Gumba INCLUSIVE 51 Helumbu Baruwa Motang 86 LWF/GMSP 30 Total trained masons: 5,567 Remaining planned figure: 235 0 82 89 Gloche 90 Note: Tatopani This map highlights the number of masons trained 28 through short training curriculum in Sindhupalchok district. The figure of masons trained was sourced form Thanpalkot HRRP 4W-R30. Further, the labels in the map (Example Nuwakot 154 :Baramchi - 55) means that 55 masons have been trained in the respective VDC/Municipality. Ichok Kiwool Listikot 0 27 ThampalChhap Sindhupalchok 40 155 Gunsakot 97 Banskharka 55 Pangtang Map Doc Name: Short_T_Sindhupalchok_R30 Palchok Fulpingkatti GLIDE Number: EQ-2015-000048-NPL Mahankal BhoteNamlang 30 0 0 Creation Date: 25 Apr 2017 0 30 Dubachour Lagarche Baramchi 114 59 55 Map Data Source: HRRP 4W-R25 (as of 25 Apr 2017) Thakani Dhuyang Marming Selang Hagam 30 Geo Data Source: DoS, MoFALD; 123 40 Web Resource: www.hrrpnepal.org SipalKavre 0 78 65 SyauleBazar Jalbire Melamchi N.P. Gati Haibung 97 0 Nawalpur 59 81 549 Batase 186 91 Maneswor Karthali Bahrabise Bhotechaur 90 84 Fulpingkot 88 ¯ Ghorthali 60 32 Badegau Kunchok 31 (1 : 250,000) 307 375 Chautara N.P. -

Chairperson's Word
Chairperson’s Word I feel proud to make a note that Sansthagat Bikas Sanjal has prevention in Kailali and Achham District. Migrant spouses successfully completed its’ 8th year of operation promoting and PLHAs have formed self- help groups and started income good governance, peacebuilding and rural community generation activities for their livelihood. They have been development through capacity development of NGO. maintaining adherence to ART. Since the country has been threatened by political instability Rural Education Project is producing significant results with and natural disaster (earthquake), Sanjal too is facing the high pass rate in SLC. Due to the commendable effort in consequences. Particularly project execution and monitoring improving education, Janjagriti Higher Secondary School in of the projects have been partly affected by the unexpected Dhading is recognised as model school by DEO. The school occurrences. Despite this, Sanjal is able to make progresses with was awarded Rs.500,000 grants from DEO this year. Similarly, its continual effort and interventions. Executive committee Sagma Secondary School, Morang has made tremendous of Sanjal is now more inclusive with participation of Janjati progress in achieving tangible results in SLC exam in women from Kosis Nepal- Okhaldhunga. Newly commenced comparison to other school in northern hilly areas of Morang practice of holding Sanjal executive committee meeting in the district. constituencies of EC members has significantly contributed to Food security projects in Morang, Achham, Banke and Surkhet mutual learning and sharing. Sanjal was able to have meetings have been implementation in partnership with 4 member of Eastern region and Western region in Okhaldhunga and organizations to improve the food and nutrition security of Kailali exploring new capacities and strengths of MOs for marginalized, vulnerable, landless and economically poor collaborative ventures. -
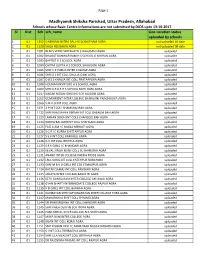
Center Information Not Updated by DIOS 13102017.Xlsx
Page 1 Madhyamik Shiksha Parishad, Uttar Pradesh, Allahabad Schools whose Basic Centre Informations are not submitted by DIOS upto 13-10-2017 Sl Dist Sch sch_name Geo-Location status uploaded by schools 1 01 1352 S NEKRAM NETRA PAL H S SCH KITHAM AGRA not uploaded till date 2 01 1620 SHILA HSS BAGIA AGRA not uploaded till date 3 01 1001 BENI S VEDIC VIDYAVATI I C BALUGANJ AGRA uploaded 4 01 1002 BHAGAT KANWAR RAM H S SCHOOL G M KHAN AGRA uploaded 5 01 1003 BAPTIST H S SCHOOL AGRA uploaded 6 01 1004 CHITRA GUPTA H S SCHOOL SHAHGANJ AGRA uploaded 7 01 1005 SHRI C P PUBLIC INTER COLLEGE AGRA uploaded 8 01 1006 SHRI D J INT COLL DHULIA GANJ AGRA uploaded 9 01 1007 D B S S KHALSA INT COLL PRATAPPURA AGRA uploaded 10 01 1008 HOLMAN INSTITUTE H S SCHOOL AGRA uploaded 11 01 1009 SHRI K R B R H S SCHOOL MOTI GANJ AGRA uploaded 12 01 1037 NAGAR NIGAM GIRLS HS SCH TAJGANJ AGRA uploaded 13 01 1052 GOVERMENT INTER COLLEGE SHAHGANJ PNACHKUIYA AGRA uploaded 14 01 1066 S M A O INT COLL AGRA uploaded 15 01 1071 A P INT COLL SHAMSHADBAD AGRA uploaded 16 01 1122 SHRI RAM SAHAY VERMA INT COLL BASAUNI BAH AGRA uploaded 17 01 1123 LAKHAN SINGH INT COLL CHANGOLI BAH AGRA uploaded 18 01 1124 RADHA BALLABH INT COLL SHAHGANJ AGRA uploaded 19 01 1125 FAIZ A AM I C NAGLA MEWATI AGRA uploaded 20 01 1126 S G R I C KURRA CHITTARPUR AGRA uploaded 21 01 1127 S S V INT COLL KARKAULI AGRA uploaded 22 01 1128 G V INT COLL BRITHLA AGRA uploaded 23 01 1129 S R K GIRLS I C KHANDARI AGRA uploaded 24 01 1130 KEVAL SINGH M INT COLL SUTHARI BAH AGRA uploaded 25 01 1131 ANAND INTER