Annexure‐ I : Specifications of FDA Approved Drug Library
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Summary of Product Characteristics
SUMMARY OF PRODUCT CHARACTERISTICS 1 NAME OF THE MEDICINAL PRODUCT *IPERTEN/ARTEDIL/MANYPER 10mg tablets IPERTEN/ARTEDIL/MANYPER 20mg tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION IPERTEN/ARTEDIL/MANYPER 10 mg tablets Each tablet contains: Manidipine hydrochloride 10mg Excipient with known effect: 119,61 mg lactose monohydrate/tablet IPERTEN/ARTEDIL/MANYPER 20 mg tablets Each tablet contains: Manidipine hydrochloride 20mg Excipient with known effect: 131,80 mg lactose monohydrate/tablet For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Tablet IPERTEN/ARTEDIL/MANYPER 10mg: pale yellow, round, scored tablet; IPERTEN/ARTEDIL/MANYPER 20mg: yellow-orange, oblong, scored tablet. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Mild to moderate essential hypertension 4.2 Posology and method of administration The recommended starting dose is 10 mg once a day. Should the antihypertensive effect be still insufficient after 2-4 weeks of treatment, it is advisable to increase the dosage to the usual maintenance dose of 20 mg once a day. Elderly In view of the slowing down of metabolism in the elderly, the recommended dose is 10mg once daily. This dosage is sufficient in most elderly patients; the risk/benefit of any dose increase should be considered with caution on an individual basis. Renal impairment In patients with mild to moderate renal dysfunction care should be taken when increasing the dosage from 10 to 20mg once a day. Hepatic impairment Due to the extensive hepatic metabolisation of manidipine, patients with mild hepatic dysfunction should not exceed 10mg once a day (see also Section 4.3 Contraindications). Tablet must be swallowed in the morning after breakfast, without chewing it, with a few liquid. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Galeterone for the Treatment of Castration- Resistant Prostate Cancer Bruce Montgomery1, Mario A
Published OnlineFirst November 2, 2015; DOI: 10.1158/1078-0432.CCR-15-1432 Cancer Therapy: Clinical Clinical Cancer Research Androgen Receptor Modulation Optimized for Response (ARMOR) Phase I and II Studies: Galeterone for the Treatment of Castration- Resistant Prostate Cancer Bruce Montgomery1, Mario A. Eisenberger2, Matthew B. Rettig3, Franklin Chu4, Roberto Pili5, Joseph J. Stephenson6, Nicholas J. Vogelzang7, Alan J. Koletsky8, Luke T. Nordquist9, William J. Edenfield10, Khalid Mamlouk11, Karen J. Ferrante11, and Mary-Ellen Taplin12 Abstract Purpose: Galeterone is a selective, multitargeted agent that Results: In ARMOR1, across all doses, 49.0% (24/49) achieved a inhibits CYP17, antagonizes the androgen receptor (AR), and 30% decline in prostate-specific antigen (PSA; PSA30) and reduces AR expression in prostate cancer cells by causing an 22.4% (11/49) demonstrated a 50% PSA decline (PSA50). In increase in AR protein degradation. These open-label phase I ARMOR2 part 1, across all doses, PSA30 was 64.0% (16/25) and and II studies [Androgen Receptor Modulation Optimized PSA50 was 48.0% (12/25). In the 2,550-mg dose cohort, PSA30 for Response-1 (ARMOR1) and ARMOR2 part 1] evaluated was 72.7% (8/11) and PSA50 was 54.5% (6/11). Galeterone was the efficacy and safety of galeterone in patients with treat- well tolerated; the most common adverse events were fatigue, ment-naive nonmetastatic or metastatic castration-resistant increased liver enzymes, gastrointestinal events, and pruritus. Most prostate cancer (CRPC) and established a dose for further were mild or moderate in severity and required no action and there study. were no apparent mineralocorticoid excess (AME) events. -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -

The Repurposing Drugs in Oncology Database
ReDO_DB: the repurposing drugs in oncology database Pan Pantziarka1,2, Ciska Verbaanderd1,3, Vidula Sukhatme4, Rica Capistrano I1, Sergio Crispino1, Bishal Gyawali1,5, Ilse Rooman1,6, An MT Van Nuffel1, Lydie Meheus1, Vikas P Sukhatme4,7 and Gauthier Bouche1 1The Anticancer Fund, Brussels, 1853 Strombeek-Bever, Belgium 2The George Pantziarka TP53 Trust, London, UK 3Clinical Pharmacology and Pharmacotherapy, Department of Pharmaceutical and Pharmacological Sciences, KU Leuven, Leuven, Belgium 4GlobalCures Inc., Newton, MA 02459 USA 5Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02115 USA 6Oncology Research Centre, Vrije Universiteit Brussel, Brussels, Belgium 7Emory University School of Medicine, Atlanta, GA 30322 USA Correspondence to: Pan Pantziarka. Email: [email protected] Abstract Repurposing is a drug development strategy that seeks to use existing medications for new indications. In oncology, there is an increased level of activity looking at the use of non-cancer drugs as possible cancer treatments. The Repurposing Drugs in Oncology (ReDO) project has used a literature-based approach to identify licensed non-cancer drugs with published evidence of anticancer activity. Data from 268 drugs have been included in a database (ReDO_DB) developed by the ReDO project. Summary results are outlined and an assessment Research of clinical trial activity also described. The database has been made available as an online open-access resource (http://www.redo-project. org/db/). Keywords: drug repurposing, repositioning, ReDO project, cancer drugs, online database Published: 06/12/2018 Received: 27/09/2018 ecancer 2018, 12:886 https://doi.org/10.3332/ecancer.2018.886 Copyright: © the authors; licensee ecancermedicalscience. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

Tranexamic Acid in the Treatment of Residual Chronic Subdural Hematoma: a Single-Centre, Observer-Blinded, Randomized Controlled Trial (Trace)
TRANEXAMIC ACID IN THE TREATMENT OF RESIDUAL CHRONIC SUBDURAL HEMATOMA: A SINGLE-CENTRE, OBSERVER-BLINDED, RANDOMIZED CONTROLLED TRIAL (TRACE) by Adriana Micheline Workewych A thesis submitted in conformity with the requirements for the degree of Master of Science Institute of Medical Science University of Toronto © Copyright by Adriana Micheline Workewych 2018 TRANEXAMIC ACID IN THE TREATMENT OF RESIDUAL CHRONIC SUBDURAL HEMATOMA: A SINGLE-CENTRE, OBSERVER-BLINDED, RANDOMIZED CONTROLLED TRIAL (TRACE) Adriana Micheline Workewych Master of Science Institute of Medical Science University of Toronto 2018 ABSTRACT Chronic subdural hematoma (CSDH) is a frequent consequence of head trauma, particularly in older individuals. Given the aging of populations globally, its incidence is projected to increase substantially. Hyperfibrinolysis may be central to CSDH enlargement by causing excessive clot degradation and liquefaction, impeding resorption. The only current standard treatment for CSDH is surgery, however, up to 31% of residual hematomas enlarge, requiring reoperation. Tranexamic acid (TXA), an antifibrinolytic medication that prevents excessively rapid clot breakdown, may help prevent CSDH enlargement, potentially eliminating the need for repeat surgery. To evaluate the feasibility of conducting a trial investigating TXA efficacy in residual CSDH, we conducted an observer-blinded, pilot randomized controlled trial (RCT). We showed this trial was feasible and safe, reporting only minor to moderate AEs, and an attrition rate of 4%. The results from this study will inform the conduct of a double-blinded RCT investigating TXA efficacy in post-operative CSDH management. ii ACKNOWLEDGEMENTS First, I would like to thank my supervisor Dr. Michael Cusimano, my mentor for nearly six years. You have always given me more opportunity than I could have ever hoped for – I could not ask for a more dedicated teacher. -
Download Product Insert (PDF)
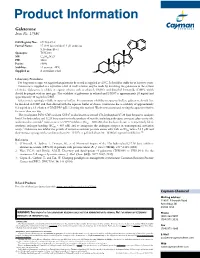
Product Information Galeterone Item No. 17586 N CAS Registry No.: 851983-85-2 Formal Name: 17-(1H-benzimidazol-1-yl)-androsta- 5,16-dien-3β-ol N Synonym: TOK-001 MF: C26H32N2O FW: 388.6 H Purity: ≥98% H H Stability: ≥2 years at -20°C Supplied as: A crystalline solid HO Laboratory Procedures For long term storage, we suggest that galeterone be stored as supplied at -20°C. It should be stable for at least two years. Galeterone is supplied as a crystalline solid. A stock solution may be made by dissolving the galeterone in the solvent of choice. Galeterone is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF), which should be purged with an inert gas. The solubility of galeterone in ethanol and DMSO is approximately 20 mg/ml and approximately 30 mg/ml in DMF. Galeterone is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, galeterone should first be dissolved in DMF and then diluted with the aqueous buffer of choice. Galeterone has a solubility of approximately 0.2 mg/ml in a 1:3 solution of DMF:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. The cytochrome P450 (CYP) isoform CYP17 is also known as steroid 17α-hydroxylase/17,20 lyase because it catalyzes both 17α-hydroxylase and 17,20 lyase reactions in the synthesis of steroids, including androgens, estrogens, glucocorticoids, 1 and mineralocorticoids. Galeterone is a CYP17 inhibitor (IC50 = 300 nM) that has been shown to competitively block synthetic androgen binding (EC50 = 845 nM) and to antagonize the androgen receptor in transcriptional activation 2 assays. -

No Benefit of Hemostatic Drugs on Acute Upper Gastrointestinal Bleeding in Cirrhosis
Hindawi BioMed Research International Volume 2020, Article ID 4097170, 11 pages https://doi.org/10.1155/2020/4097170 Research Article No Benefit of Hemostatic Drugs on Acute Upper Gastrointestinal Bleeding in Cirrhosis Yang An,1,2 Zhaohui Bai,1,2 Xiangbo Xu,1,2 Xiaozhong Guo ,1 Fernando Gomes Romeiro ,3 Cyriac Abby Philips,4 Yingying Li,5 Yanyan Wu,1,6 and Xingshun Qi 1 1Department of Gastroenterology, General Hospital of Northern Theater Command (formerly General Hospital of Shenyang Military Area), Shenyang 110840, China 2Postgraduate College, Shenyang Pharmaceutical University, Shenyang 110016, China 3Department of Internal Medicine, Botucatu Medical School, UNESP-Univ Estadual Paulista. Av. Prof. Mário Rubens Guimarães Montenegro, s/n Distrito de Rubião Jr, Botucatu, Brazil 4The Liver Unit and Monarch Liver Lab, Cochin Gastroenterology Group, Ernakulam Medical Center, Kochi, 682028 Kerala, India 5Department of Gastroenterology, The First People’s Hospital of Huainan, Huainan 232007, China 6Postgraduate College, Jinzhou Medical University, Jinzhou 121001, China Correspondence should be addressed to Xingshun Qi; [email protected] Received 28 February 2020; Revised 25 May 2020; Accepted 1 June 2020; Published 27 June 2020 Academic Editor: Hongqun Liu Copyright © 2020 Yang An et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Background and Aims. Acute upper gastrointestinal bleeding (AUGIB) is one of the most life-threatening emergency conditions. Hemostatic drugs are often prescribed to control AUGIB in clinical practice but have not been recommended by major guidelines and consensus. -

Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Cr
Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Crizotinib (PF-02341066) 1 4 55 Docetaxel 1 5 98 Anastrozole 1 6 25 Cladribine 1 7 23 Methotrexate 1 8 -187 Letrozole 1 9 65 Entecavir Hydrate 1 10 48 Roxadustat (FG-4592) 1 11 19 Imatinib Mesylate (STI571) 1 12 0 Sunitinib Malate 1 13 34 Vismodegib (GDC-0449) 1 14 64 Paclitaxel 1 15 89 Aprepitant 1 16 94 Decitabine 1 17 -79 Bendamustine HCl 1 18 19 Temozolomide 1 19 -111 Nepafenac 1 20 24 Nintedanib (BIBF 1120) 1 21 -43 Lapatinib (GW-572016) Ditosylate 1 22 88 Temsirolimus (CCI-779, NSC 683864) 1 23 96 Belinostat (PXD101) 1 24 46 Capecitabine 1 25 19 Bicalutamide 1 26 83 Dutasteride 1 27 68 Epirubicin HCl 1 28 -59 Tamoxifen 1 29 30 Rufinamide 1 30 96 Afatinib (BIBW2992) 1 31 -54 Lenalidomide (CC-5013) 1 32 19 Vorinostat (SAHA, MK0683) 1 33 38 Rucaparib (AG-014699,PF-01367338) phosphate1 34 14 Lenvatinib (E7080) 1 35 80 Fulvestrant 1 36 76 Melatonin 1 37 15 Etoposide 1 38 -69 Vincristine sulfate 1 39 61 Posaconazole 1 40 97 Bortezomib (PS-341) 1 41 71 Panobinostat (LBH589) 1 42 41 Entinostat (MS-275) 1 43 26 Cabozantinib (XL184, BMS-907351) 1 44 79 Valproic acid sodium salt (Sodium valproate) 1 45 7 Raltitrexed 1 46 39 Bisoprolol fumarate 1 47 -23 Raloxifene HCl 1 48 97 Agomelatine 1 49 35 Prasugrel 1 50 -24 Bosutinib (SKI-606) 1 51 85 Nilotinib (AMN-107) 1 52 99 Enzastaurin (LY317615) 1 53 -12 Everolimus (RAD001) 1 54 94 Regorafenib (BAY 73-4506) 1 55 24 Thalidomide 1 56 40 Tivozanib (AV-951) 1 57 86 Fludarabine