Multiple Technology Appraisal Avatrombopag and Lusutrombopag
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -
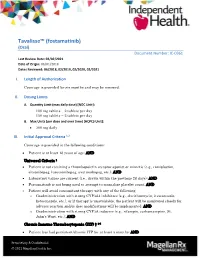
Tavalisse™ (Fostamatinib) (Oral) Document Number: IC-0361 Last Review Date: 02/02/2021 Date of Origin: 06/01/2018 Dates Reviewed: 06/2018, 02/2019, 02/2020, 02/2021
Tavalisse™ (fostamatinib) (Oral) Document Number: IC-0361 Last Review Date: 02/02/2021 Date of Origin: 06/01/2018 Dates Reviewed: 06/2018, 02/2019, 02/2020, 02/2021 I. Length of Authorization Coverage is provided for six months and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: 100 mg tablets – 2 tablets per day 150 mg tablets – 2 tablets per day B. Max Units (per dose and over time) [HCPCS Unit]: 300 mg daily III. Initial Approval Criteria 1,2 Coverage is provided in the following conditions: Patient is at least 18 years of age; AND Universal Criteria 1 Patient is not receiving a thrombopoietin receptor agonist or mimetic (e.g., romiplostim, eltrombopag, lusutrombopag, avatrombopag, etc.); AND Laboratory values are current (i.e., drawn within the previous 28 days); AND Fostamatinib is not being used to attempt to normalize platelet count; AND Patient will avoid concomitant therapy with any of the following: o Coadministration with strong CYP3A4 inhibitors (e.g., clarithromycin, itraconazole, ketoconazole, etc.), or if therapy is unavoidable, the patient will be monitored closely for adverse reaction and/or dose modifications will be implemented; AND o Coadministration with strong CYP3A inducers (e.g., rifampin, carbamazepine, St. John’s Wort, etc.); AND Chronic Immune Thrombocytopenia (ITP) † 1-5 Patient has had persistent/chronic ITP for at least 3 months; AND Proprietary & Confidential © 2021 Magellan Health, Inc. Patient has previously failed any of the following treatments for ITP: Patient has failed previous therapy with corticosteroids (i.e., patient had no response to at least a 3-month trial or is corticosteroid-dependent); OR Patient has failed previous therapy with immunoglobulins; OR Patient has had a splenectomy; OR Patient has failed previous therapy with a thrombopoietin receptor agonist; AND The patient is at increased risk for bleeding as indicated by platelet count of less than 30 × 109/L (30,000/mm³) † FDA Approved Indication(s) IV. -

The Potential Role of Recombinant Activated FVII in the Management of Critical Hemato-Oncological Bleeding: a Systematic Review
Bone Marrow Transplantation (2007) 39, 729–735 & 2007 Nature Publishing Group All rights reserved 0268-3369/07 $30.00 www.nature.com/bmt REVIEW The potential role of recombinant activated FVII in the management of critical hemato-oncological bleeding: a systematic review M Franchini1, D Veneri2 and G Lippi3 1Servizio di Immunoematologia e Trasfusione – Centro Emofilia, Azienda Ospedaliera di Verona, Verona, Italy; 2Dipartimento di Medicina Clinica e Sperimentale, Sezione di Ematologia, Universita` di Verona, Verona, Italy and 3Dipartimento di Scienze Biomediche e Morfologiche, Istituto di Chimica e Microscopia Clinica, Universita` di Verona, Verona, Italy Recombinant activated factor VII (rFVIIa) is an hemo- situations unresponsive to conventional therapy to control static agent that was originally developed for the excessive bleeding and reduce exposure to allogeneic blood. treatment of hemorrhage in patients with hemophilia and These include intracerebral hemorrhage, oral anticoagu- inhibitors.However, in the last few years rFVIIa has been lant-induced hemorrhage, thrombocytopenia, bleeding employed with success in a broad spectrum of congenital associated with hepatic failure, major surgery, trauma and acquired bleeding conditions.In this systematic review and life-threatening obstetrical, and gynecologic hemor- we present the current knowledge on the use of this drug in rhagic complications.5–9 patients suffering from hemato-oncological disorders, In this systematic review we have collected the available which are quite commonly complicated by severe hemor- data from the literature on the use of rFVIIa in hemato- rhage.On the whole, data in the literature suggest a oncological patients with severe bleeding, unresponsive to potential role for rFVIIa in the management of bleeding standard therapy. -

Tranexamic Acid in the Treatment of Residual Chronic Subdural Hematoma: a Single-Centre, Observer-Blinded, Randomized Controlled Trial (Trace)
TRANEXAMIC ACID IN THE TREATMENT OF RESIDUAL CHRONIC SUBDURAL HEMATOMA: A SINGLE-CENTRE, OBSERVER-BLINDED, RANDOMIZED CONTROLLED TRIAL (TRACE) by Adriana Micheline Workewych A thesis submitted in conformity with the requirements for the degree of Master of Science Institute of Medical Science University of Toronto © Copyright by Adriana Micheline Workewych 2018 TRANEXAMIC ACID IN THE TREATMENT OF RESIDUAL CHRONIC SUBDURAL HEMATOMA: A SINGLE-CENTRE, OBSERVER-BLINDED, RANDOMIZED CONTROLLED TRIAL (TRACE) Adriana Micheline Workewych Master of Science Institute of Medical Science University of Toronto 2018 ABSTRACT Chronic subdural hematoma (CSDH) is a frequent consequence of head trauma, particularly in older individuals. Given the aging of populations globally, its incidence is projected to increase substantially. Hyperfibrinolysis may be central to CSDH enlargement by causing excessive clot degradation and liquefaction, impeding resorption. The only current standard treatment for CSDH is surgery, however, up to 31% of residual hematomas enlarge, requiring reoperation. Tranexamic acid (TXA), an antifibrinolytic medication that prevents excessively rapid clot breakdown, may help prevent CSDH enlargement, potentially eliminating the need for repeat surgery. To evaluate the feasibility of conducting a trial investigating TXA efficacy in residual CSDH, we conducted an observer-blinded, pilot randomized controlled trial (RCT). We showed this trial was feasible and safe, reporting only minor to moderate AEs, and an attrition rate of 4%. The results from this study will inform the conduct of a double-blinded RCT investigating TXA efficacy in post-operative CSDH management. ii ACKNOWLEDGEMENTS First, I would like to thank my supervisor Dr. Michael Cusimano, my mentor for nearly six years. You have always given me more opportunity than I could have ever hoped for – I could not ask for a more dedicated teacher. -

No Benefit of Hemostatic Drugs on Acute Upper Gastrointestinal Bleeding in Cirrhosis
Hindawi BioMed Research International Volume 2020, Article ID 4097170, 11 pages https://doi.org/10.1155/2020/4097170 Research Article No Benefit of Hemostatic Drugs on Acute Upper Gastrointestinal Bleeding in Cirrhosis Yang An,1,2 Zhaohui Bai,1,2 Xiangbo Xu,1,2 Xiaozhong Guo ,1 Fernando Gomes Romeiro ,3 Cyriac Abby Philips,4 Yingying Li,5 Yanyan Wu,1,6 and Xingshun Qi 1 1Department of Gastroenterology, General Hospital of Northern Theater Command (formerly General Hospital of Shenyang Military Area), Shenyang 110840, China 2Postgraduate College, Shenyang Pharmaceutical University, Shenyang 110016, China 3Department of Internal Medicine, Botucatu Medical School, UNESP-Univ Estadual Paulista. Av. Prof. Mário Rubens Guimarães Montenegro, s/n Distrito de Rubião Jr, Botucatu, Brazil 4The Liver Unit and Monarch Liver Lab, Cochin Gastroenterology Group, Ernakulam Medical Center, Kochi, 682028 Kerala, India 5Department of Gastroenterology, The First People’s Hospital of Huainan, Huainan 232007, China 6Postgraduate College, Jinzhou Medical University, Jinzhou 121001, China Correspondence should be addressed to Xingshun Qi; [email protected] Received 28 February 2020; Revised 25 May 2020; Accepted 1 June 2020; Published 27 June 2020 Academic Editor: Hongqun Liu Copyright © 2020 Yang An et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Background and Aims. Acute upper gastrointestinal bleeding (AUGIB) is one of the most life-threatening emergency conditions. Hemostatic drugs are often prescribed to control AUGIB in clinical practice but have not been recommended by major guidelines and consensus. -

Blood Modifier Agents Policy #: Rx.01.208
Pharmacy Policy Bulletin Title: Blood Modifier Agents Policy #: Rx.01.208 Application of pharmacy policy is determined by benefits and contracts. Benefits may vary based on product line, group, or contract. Some medications may be subject to precertification, age, quantity, or formulary restrictions (ie limits on non-preferred drugs). Individual member benefits must be verified. This pharmacy policy document describes the status of pharmaceutical information and/or technology at the time the document was developed. Since that time, new information relating to drug efficacy, interactions, contraindications, dosage, administration routes, safety, or FDA approval may have changed. This Pharmacy Policy will be regularly updated as scientific and medical literature becomes available. This information may include new FDA-approved indications, withdrawals, or other FDA alerts. This type of information is relevant not only when considering whether this policy should be updated, but also when applying it to current requests for coverage. Members are advised to use participating pharmacies in order to receive the highest level of benefits. Intent: The intent of this policy is to communicate the medical necessity criteria for eltrombopag olamine (Promacta®), fostamatinib disodium (Tavalisse™), avatrombopag (Doptelet®), lusutrombopag (Mulpleta®) as provided under the member's prescription drug benefit. Description: Idiopathic thrombocytopenia purpura (ITP): ITP is an immune disorder in which the blood doesn't clot normally. ITP can cause excessive bruising and bleeding and can be characterized as an unusually low level of platelets, or thrombocytes, in the blood results in ITP. Thrombocytopenia in patients with hepatitis C: Thrombocytopenia can occur in patients with chronic hepatitis C virus (HCV) infection. -

Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Cr
Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Crizotinib (PF-02341066) 1 4 55 Docetaxel 1 5 98 Anastrozole 1 6 25 Cladribine 1 7 23 Methotrexate 1 8 -187 Letrozole 1 9 65 Entecavir Hydrate 1 10 48 Roxadustat (FG-4592) 1 11 19 Imatinib Mesylate (STI571) 1 12 0 Sunitinib Malate 1 13 34 Vismodegib (GDC-0449) 1 14 64 Paclitaxel 1 15 89 Aprepitant 1 16 94 Decitabine 1 17 -79 Bendamustine HCl 1 18 19 Temozolomide 1 19 -111 Nepafenac 1 20 24 Nintedanib (BIBF 1120) 1 21 -43 Lapatinib (GW-572016) Ditosylate 1 22 88 Temsirolimus (CCI-779, NSC 683864) 1 23 96 Belinostat (PXD101) 1 24 46 Capecitabine 1 25 19 Bicalutamide 1 26 83 Dutasteride 1 27 68 Epirubicin HCl 1 28 -59 Tamoxifen 1 29 30 Rufinamide 1 30 96 Afatinib (BIBW2992) 1 31 -54 Lenalidomide (CC-5013) 1 32 19 Vorinostat (SAHA, MK0683) 1 33 38 Rucaparib (AG-014699,PF-01367338) phosphate1 34 14 Lenvatinib (E7080) 1 35 80 Fulvestrant 1 36 76 Melatonin 1 37 15 Etoposide 1 38 -69 Vincristine sulfate 1 39 61 Posaconazole 1 40 97 Bortezomib (PS-341) 1 41 71 Panobinostat (LBH589) 1 42 41 Entinostat (MS-275) 1 43 26 Cabozantinib (XL184, BMS-907351) 1 44 79 Valproic acid sodium salt (Sodium valproate) 1 45 7 Raltitrexed 1 46 39 Bisoprolol fumarate 1 47 -23 Raloxifene HCl 1 48 97 Agomelatine 1 49 35 Prasugrel 1 50 -24 Bosutinib (SKI-606) 1 51 85 Nilotinib (AMN-107) 1 52 99 Enzastaurin (LY317615) 1 53 -12 Everolimus (RAD001) 1 54 94 Regorafenib (BAY 73-4506) 1 55 24 Thalidomide 1 56 40 Tivozanib (AV-951) 1 57 86 Fludarabine -

Advances in Hepatology and Robley Rex VAMC NAFLD/NASH
Luis S. Marsano, MD, FAASLD, FACG, AGAF, FASGE Professor of Medicine, Director of Hepatology University of Louisville Advances in Hepatology and Robley Rex VAMC NAFLD/NASH Coagulation in Cirrhosis Topics Hepatocellular Carcinoma Miscellaneous Definitions of NAFLD, NAFL and NASH Nonalcoholic fatty liver disease (NAFLD) a. Evidence of hepatic steatosis by imaging or histology b. Lack of secondary causes of hepatic fat accumulation Non-alcoholic steato-hepatitis (NASH) Nonalcoholic fatty liver (NAFL) ≥5% hepatic steatosis and ≥5% hepatic steatosis without inflammation with hepatocyte injury evidence of hepatocellular injury in (eg, ballooning), with or without any the form of hepatocyte ballooning fibrosis Chalasani N, et al. Hepatology. 2017. doi:10.1002/hep.29367 Estimated Global Prevalence of NAFLD: 25% 24% 24% 27% 32% 13% 31% Meta-analysis: NAFLD diagnosed by imaging (US, CT, MRI/SPECT; n=45 studies). Younossi ZM, et al. Hepatology. 2016;64:73-84. 4 Estimated Global NASH Prevalence 6-7% 7-8% 5-6% 8-10% 3-4% 8-9% NASH is Prevalent Globally *25-30% of NAFLD prevalence assumed to be NASH in the above map. 5 Younossi ZM, et al. Hepatology2016;64:73-84; Williams CD, et al. Gasteoenterology 2011;140:124-131. Estimated NASH Prevalence in the U.S. ~30% of U.S. adult population Non-Alcoholic estimated to have NAFLD Fatty Liver Disease NAFLD 83.1 Million Non-Alcoholic Steatohepatitis NASH 16.5 Million Disease Spectrum Disease NASH with 3.3 Million F3/F4 Fibrosis F3 = 2 M; F4 = 1.3 M Unmet Need Estes, et al. Hepatology. 2017. doi:10.1002/hep.29466. -

Immune Thrombocytopenia in Adults: Modern Approaches to Diagnosis and Treatment
Published online: 2019-12-12 275 Immune Thrombocytopenia in Adults: Modern Approaches to Diagnosis and Treatment Hanny Al-Samkari, MD1 David J. Kuter, MD, DPhil1 1 Division of Hematology, Massachusetts General Hospital, Harvard Address for correspondence Hanny Al-Samkari, MD, Division of Medical School, Boston, Massachusetts Hematology, Massachusetts General Hospital, Suite 118, Room 112, Zero Emerson Place, Boston, MA 02114 Semin Thromb Hemost 2020;46:275–288. (e-mail: [email protected]). Abstract Immune thrombocytopenia (ITP) is an autoimmune bleeding disorder affecting approximately 1 in 20,000 people. Patients typically present with clinically benign mucocutaneous bleeding, but morbid internal bleeding can occur. Diagnosis remains clinical, possible only after ruling out other causes of thrombocytopenia through history and laboratory testing. Many adult patients do not require treatment. For those requiring intervention, initial treatment of adult ITP is with corticosteroids, intravenous immunoglobulin, or intravenous anti-RhD immune globulin. These agents are rapid- acting but do not result in durable remissions in most patients. No corticosteroid has Keywords demonstrated superiority to others for ITP treatment. Subsequent treatment of adult ► platelets ITP is typically with thrombopoietin receptor agonists (TPO-RAs; romiplostim or ► immune eltrombopag), rituximab, or splenectomy. TPO-RAs are newer agents that offer an thrombocytopenia excellent response rate but may require prolonged treatment. The choice between ► diagnosis subsequent treatments involves consideration of operative risk, risk of asplenia, drug ► treatment side-effects, quality-of-life issues, and financial costs. Given the efficacy of medical ► corticosteroids therapies and the rate of spontaneous remission in the first year after diagnosis, ► intravenous splenectomy is frequently deferred in modern ITP treatment algorithms. -

Lusutrombopag for Treating Thrombocytopenia in People with Chronic Liver Disease Needing a Planned Invasive Procedure
Lusutrombopag for treating thrombocytopenia in people with chronic liver disease needing a planned invasive procedure Technology appraisal guidance Published: 8 January 2020 www.nice.org.uk/guidance/ta617 © NICE 2020. All rights reserved. Subject to Notice of rights (https://www.nice.org.uk/terms-and-conditions#notice-of- rights). Lusutrombopag for treating thrombocytopenia in people with chronic liver disease needing a planned invasive procedure (TA617) Your responsibility The recommendations in this guidance represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, health professionals are expected to take this guidance fully into account, alongside the individual needs, preferences and values of their patients. The application of the recommendations in this guidance are at the discretion of health professionals and their individual patients and do not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian. Commissioners and/or providers have a responsibility to provide the funding required to enable the guidance to be applied when individual health professionals and their patients wish to use it, in accordance with the NHS Constitution. They should do so in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Commissioners and providers have a responsibility to promote an environmentally sustainable health and care system and should assess and reduce the environmental impact of implementing NICE recommendations wherever possible. © NICE 2020. All rights reserved. -

WO 2014/153004 Al 25 September 2014 (25.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2014/153004 Al 25 September 2014 (25.09.2014) P O P C T (51) International Patent Classification: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, A61L 27/58 (2006.01) A61L 27/52 (2006.01) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (21) International Application Number: OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, PCT/US20 14/028622 SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, (22) International Filing Date: TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, 14 March 2014 (14.03.2014) ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (26) Publication Language: English GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (30) Priority Data: UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, 61/785,477 14 March 2013 (14.03.2013) US TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, LV, (71) Applicant: MEDICUS BIOSCIENCES LLC [US/US]; MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, SM, 2528 Qume Dr., Unit #1, San Jose, CA 95 13 1 (US).