1 Cannabis-Based Medicine Reduces Multiple
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Table 1.Xlsx
SUPPLEMENTARY APPENDIX Chromothripsis is linked to TP53 alteration, cell cycle impairment, and dismal outcome in acute myeloid leukemia with complex karyotype Frank G. Rücker, 1 Anna Dolnik, 1 Tamara J. Blätte, 1 Veronica Teleanu, 1 Aurélie Ernst, 2 Felicitas Thol, 3 Michael Heuser, 3 Arnold Ganser, 3 Hartmut Döhner, 1 Konstanze Döhner *1 and Lars Bullinger *1,4 1Department of Internal Medicine III, University Hospital of Ulm, Albert-Einstein-Allee 23; 2Division of Molecular Genetics, German Cancer Consor - tium (DKTK), German Cancer Research Center (DKFZ), Heidelberg; 3Department of Hematology, Hemostasis, Oncology, and Stem Cell Transplanta - tion, Hannover Medical School and 4Department of Hematology, Oncology and Tumor Immunology, Charité-University Medicine Berlin, Campus Virchow Klinikum, Berlin, Germany *KD and LB contributed equally to this work. Correspondence: [email protected] doi:10.3324/haematol.2017.180497 Supplementary Table 1 Top 200 differentially expressed genes in chromothripsis‐positive (n=13) vs –negative (n=14) CK‐AML (p‐value <.05) Symbol ID LogFC p value PSMB10 5699 ‐1,652 4,81E‐05 ADAMTS6 11174 ‐1,736 1,50E‐04 SLC7A6 9057 ‐1,317 6,80E‐04 VANGL1 81839 2,403 6,94E‐04 ZNF197 10168 1,409 7,30E‐04 TAS2R62P 338399 ‐1,404 9,22E‐04 PLA2G15 23659 ‐1,455 0,001 CBFB 865 ‐1,453 0,001 CNOT8 9337 ‐1,449 0,001 ACD 65057 ‐1,329 0,001 CKLF 51192 ‐1,657 0,002 CMTM3 123920 ‐1,48 0,002 FAM192A 80011 ‐1,408 0,002 SSH3 54961 ‐1,279 0,002 ZNF415 55786 1,425 0,002 BEX2 84707 1,57 0,002 GCNT2 2651 1,732 0,002 PIM1 5292 1,935 -

Single Cell Derived Clonal Analysis of Human Glioblastoma Links
SUPPLEMENTARY INFORMATION: Single cell derived clonal analysis of human glioblastoma links functional and genomic heterogeneity ! Mona Meyer*, Jüri Reimand*, Xiaoyang Lan, Renee Head, Xueming Zhu, Michelle Kushida, Jane Bayani, Jessica C. Pressey, Anath Lionel, Ian D. Clarke, Michael Cusimano, Jeremy Squire, Stephen Scherer, Mark Bernstein, Melanie A. Woodin, Gary D. Bader**, and Peter B. Dirks**! ! * These authors contributed equally to this work.! ** Correspondence: [email protected] or [email protected]! ! Supplementary information - Meyer, Reimand et al. Supplementary methods" 4" Patient samples and fluorescence activated cell sorting (FACS)! 4! Differentiation! 4! Immunocytochemistry and EdU Imaging! 4! Proliferation! 5! Western blotting ! 5! Temozolomide treatment! 5! NCI drug library screen! 6! Orthotopic injections! 6! Immunohistochemistry on tumor sections! 6! Promoter methylation of MGMT! 6! Fluorescence in situ Hybridization (FISH)! 7! SNP6 microarray analysis and genome segmentation! 7! Calling copy number alterations! 8! Mapping altered genome segments to genes! 8! Recurrently altered genes with clonal variability! 9! Global analyses of copy number alterations! 9! Phylogenetic analysis of copy number alterations! 10! Microarray analysis! 10! Gene expression differences of TMZ resistant and sensitive clones of GBM-482! 10! Reverse transcription-PCR analyses! 11! Tumor subtype analysis of TMZ-sensitive and resistant clones! 11! Pathway analysis of gene expression in the TMZ-sensitive clone of GBM-482! 11! Supplementary figures and tables" 13" "2 Supplementary information - Meyer, Reimand et al. Table S1: Individual clones from all patient tumors are tumorigenic. ! 14! Fig. S1: clonal tumorigenicity.! 15! Fig. S2: clonal heterogeneity of EGFR and PTEN expression.! 20! Fig. S3: clonal heterogeneity of proliferation.! 21! Fig. -

Sex-Specific Transcriptome Differences in Human Adipose
G C A T T A C G G C A T genes Article Sex-Specific Transcriptome Differences in Human Adipose Mesenchymal Stem Cells 1, 2, 3 1,3 Eva Bianconi y, Raffaella Casadei y , Flavia Frabetti , Carlo Ventura , Federica Facchin 1,3,* and Silvia Canaider 1,3 1 National Laboratory of Molecular Biology and Stem Cell Bioengineering of the National Institute of Biostructures and Biosystems (NIBB)—Eldor Lab, at the Innovation Accelerator, CNR, Via Piero Gobetti 101, 40129 Bologna, Italy; [email protected] (E.B.); [email protected] (C.V.); [email protected] (S.C.) 2 Department for Life Quality Studies (QuVi), University of Bologna, Corso D’Augusto 237, 47921 Rimini, Italy; [email protected] 3 Department of Experimental, Diagnostic and Specialty Medicine (DIMES), University of Bologna, Via Massarenti 9, 40138 Bologna, Italy; fl[email protected] * Correspondence: [email protected]; Tel.: +39-051-2094114 These authors contributed equally to this work. y Received: 1 July 2020; Accepted: 6 August 2020; Published: 8 August 2020 Abstract: In humans, sexual dimorphism can manifest in many ways and it is widely studied in several knowledge fields. It is increasing the evidence that also cells differ according to sex, a correlation still little studied and poorly considered when cells are used in scientific research. Specifically, our interest is on the sex-related dimorphism on the human mesenchymal stem cells (hMSCs) transcriptome. A systematic meta-analysis of hMSC microarrays was performed by using the Transcriptome Mapper (TRAM) software. This bioinformatic tool was used to integrate and normalize datasets from multiple sources and allowed us to highlight chromosomal segments and genes differently expressed in hMSCs derived from adipose tissue (hADSCs) of male and female donors. -

WO 2019/068007 Al Figure 2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2019/068007 Al 04 April 2019 (04.04.2019) W 1P O PCT (51) International Patent Classification: (72) Inventors; and C12N 15/10 (2006.01) C07K 16/28 (2006.01) (71) Applicants: GROSS, Gideon [EVIL]; IE-1-5 Address C12N 5/10 (2006.0 1) C12Q 1/6809 (20 18.0 1) M.P. Korazim, 1292200 Moshav Almagor (IL). GIBSON, C07K 14/705 (2006.01) A61P 35/00 (2006.01) Will [US/US]; c/o ImmPACT-Bio Ltd., 2 Ilian Ramon St., C07K 14/725 (2006.01) P.O. Box 4044, 7403635 Ness Ziona (TL). DAHARY, Dvir [EilL]; c/o ImmPACT-Bio Ltd., 2 Ilian Ramon St., P.O. (21) International Application Number: Box 4044, 7403635 Ness Ziona (IL). BEIMAN, Merav PCT/US2018/053583 [EilL]; c/o ImmPACT-Bio Ltd., 2 Ilian Ramon St., P.O. (22) International Filing Date: Box 4044, 7403635 Ness Ziona (E.). 28 September 2018 (28.09.2018) (74) Agent: MACDOUGALL, Christina, A. et al; Morgan, (25) Filing Language: English Lewis & Bockius LLP, One Market, Spear Tower, SanFran- cisco, CA 94105 (US). (26) Publication Language: English (81) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of national protection available): AE, AG, AL, AM, 62/564,454 28 September 2017 (28.09.2017) US AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, 62/649,429 28 March 2018 (28.03.2018) US CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, (71) Applicant: IMMP ACT-BIO LTD. -
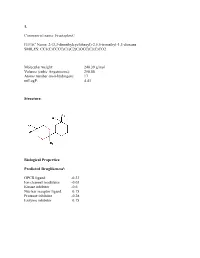
Sean Raspet – Molecules
1. Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Molecular weight: 240.39 g/mol Volume (cubic Angstroems): 258.88 Atoms number (non-hydrogen): 17 miLogP: 4.43 Structure: Biological Properties: Predicted Druglikenessi: GPCR ligand -0.23 Ion channel modulator -0.03 Kinase inhibitor -0.6 Nuclear receptor ligand 0.15 Protease inhibitor -0.28 Enzyme inhibitor 0.15 Commercial name: Fructaplex© IUPAC Name: 2-(3,3-dimethylcyclohexyl)-2,5,5-trimethyl-1,3-dioxane SMILES: CC1(C)CCCC(C1)C2(C)OCC(C)(C)CO2 Predicted Olfactory Receptor Activityii: OR2L13 83.715% OR1G1 82.761% OR10J5 80.569% OR2W1 78.180% OR7A2 77.696% 2. Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Molecular weight: 239.36 Volume (cubic Angstroems): 252.83 Atoms number (non-hydrogen): 17 miLogP: 4.33 Structure: Biological Properties: Predicted Druglikeness: GPCR ligand -0.6 Ion channel modulator -0.41 Kinase inhibitor -0.93 Nuclear receptor ligand -0.17 Protease inhibitor -0.39 Enzyme inhibitor 0.01 Commercial name: Sylvoxime© IUPAC Name: N-[4-(1-ethoxyethenyl)-3,3,5,5tetramethylcyclohexylidene]hydroxylamine SMILES: CCOC(=C)C1C(C)(C)CC(CC1(C)C)=NO Predicted Olfactory Receptor Activity: OR52D1 71.900% OR1G1 70.394% 0R52I2 70.392% OR52I1 70.390% OR2Y1 70.378% 3. Commercial name: Hyperflor© IUPAC Name: 2-benzyl-1,3-dioxan-5-one SMILES: O=C1COC(CC2=CC=CC=C2)OC1 Molecular weight: 192.21 g/mol Volume -

Genetic Characterization of Greek Population Isolates Reveals Strong Genetic Drift at Missense and Trait-Associated Variants
ARTICLE Received 22 Apr 2014 | Accepted 22 Sep 2014 | Published 6 Nov 2014 DOI: 10.1038/ncomms6345 OPEN Genetic characterization of Greek population isolates reveals strong genetic drift at missense and trait-associated variants Kalliope Panoutsopoulou1,*, Konstantinos Hatzikotoulas1,*, Dionysia Kiara Xifara2,3, Vincenza Colonna4, Aliki-Eleni Farmaki5, Graham R.S. Ritchie1,6, Lorraine Southam1,2, Arthur Gilly1, Ioanna Tachmazidou1, Segun Fatumo1,7,8, Angela Matchan1, Nigel W. Rayner1,2,9, Ioanna Ntalla5,10, Massimo Mezzavilla1,11, Yuan Chen1, Chrysoula Kiagiadaki12, Eleni Zengini13,14, Vasiliki Mamakou13,15, Antonis Athanasiadis16, Margarita Giannakopoulou17, Vassiliki-Eirini Kariakli5, Rebecca N. Nsubuga18, Alex Karabarinde18, Manjinder Sandhu1,8, Gil McVean2, Chris Tyler-Smith1, Emmanouil Tsafantakis12, Maria Karaleftheri16, Yali Xue1, George Dedoussis5 & Eleftheria Zeggini1 Isolated populations are emerging as a powerful study design in the search for low-frequency and rare variant associations with complex phenotypes. Here we genotype 2,296 samples from two isolated Greek populations, the Pomak villages (HELIC-Pomak) in the North of Greece and the Mylopotamos villages (HELIC-MANOLIS) in Crete. We compare their genomic characteristics to the general Greek population and establish them as genetic isolates. In the MANOLIS cohort, we observe an enrichment of missense variants among the variants that have drifted up in frequency by more than fivefold. In the Pomak cohort, we find novel associations at variants on chr11p15.4 showing large allele frequency increases (from 0.2% in the general Greek population to 4.6% in the isolate) with haematological traits, for example, with mean corpuscular volume (rs7116019, P ¼ 2.3 Â 10 À 26). We replicate this association in a second set of Pomak samples (combined P ¼ 2.0 Â 10 À 36). -
Get High-Res Image
150 100 50 163 169 313 # mutations Non syn. Syn. E">)->(A/T: E">6A/C/T)->(A/T) flip A->6";): indel+null double_null # mutations/Mb 0 20 40 60 80 2% 6% 4% 5% 1% 3% 3% 5% 4% 1% 3% 2% 10% 8% 5% 2% 3% 5% 7% 2% 4% 1% 5% 2% 4% 4% 6% 4% 5% 2% 2% 5% 4% 3% 6% 3% 17% 2% 1% 1% 6% 3% 1% 4% 1% 2% 3% 8% 2% 2% 5% 3% 2% 1% 6% 5% 2% 2% 4% 3% 6% 3% 1% 3% 3% 5% 1% 4% 2% 0% 5% 3% 5% 4% 1% 3% 15% 4% 2% 10% 7% 7% 3% 10% 3% 6% 4% 3% 11% 4% 3% 6% 21% 3% 3% 4% 8% 2% 6% 5% 4% 8% 3% 3% 6% 1% 6% 3% 2% 5% 7% 5% 3% 3% 2% 10% 3% 17% 6% 6% 4% 6% 12% 9% 5% 6% 5% 4% 3% 2% 21% 5% 4% 4% 17% 5% 3% 4% 3% 4% 4% 7% 7% 6% 6% 6% 4% 6% 6% 6% 8% 6% 1% 2% 2% 2% 3% 4% 8% 13% 17% 30% 54% 15% 0 (0A$205243952TP (0A$297281792TP(0A$273246702TP (0A$299280252TP(0A$255282992TP (0A$2MP2A4T&2TP(0A$250259392TP (0A$205254252TP(0A$244267792TP (0A$255279132TP(0A$275251462TP (0A$2622A4712TP(0A$255275742TP (0A$205244322TP(0A$244281202TP (0A$2442A4792TP(0A$249244872TP (0A$2N-2A4'&2TP(0A$286282802TP (0A$278275352TP(0A$255215962TP (0A$235236152TP(0A$244261442TP (0A$2N-2A55!2TP(0A$278271662TP (0A$244267762TP(0A$244276712TP (0A$2-2281942TP(0A$267237742TP (0A$2N-2A4'P2TP(0A$255282032TP (0A$205244172TP(0A$255285082TP (0A$286283592TP(0A$286277132TP (0A$2MP2A4TE2TP(0A$280256082TP (0A$299280322TP(0A$255286152TP (0A$2622A46S2TP(0A$250259322TP (0A$2N-2A55*2TP(0A$278271612TP (0A$2952A4VP2TP(0A$249245072TP (0A$249244862TP(0A$291268492TP (0A$2622A46P2TP(0A$2622A4702TP (0A$205244222TP(0A$250250722TP (0A$2MP2A4TH2TP(0A$275270312TP (0A$299280332TP(0A$255280942TP (0A$295270392TP(0A$255283022TP (0A$249245052TP(0A$293280672TP -

Supplemental Files 1-5.Pdf
Supplemental file 1: The whole list of tumor aberrations by time tumor biopsy ctDNA 2002 (T1) 2012 (M1) 2015 (M2) 08/2015 09/2015 11/2015 02/2016 05/2016 07/2016 11/2016 02/2017 05/2017 07/2017 11/2017 PIK3CA Q546R PIK3CA Q546R PIK3CA Q546R PIK3CA Q546R 0.30% PIK3CA Q546R 1.30% PIK3CA Q546R 5.40% PIK3CA Q546R 12.50% PIK3CA Q546R 9.50% PIK3CA Q546R 32.58% PIK3CA Q546R 44.30% PIK3CA Q546R 15.40% PIK3CA Q546R 41.00% TP53 E180K TP53 E180K TP53 E180K TP53 E180K 0.30% TP53 E180K 1.00% TP53 E180K 4.80% PIK3CA M1043I 0.20% PIK3CA M1043I 0.70% PIK3CA E453K 0.69% PIK3CA E453K 3.20% PIK3CA E453K 0.55% PIK3CA M1043I 0.20% PIK3R2 S688* PIK3R2 S688* ATR E2579K VHL E173Q 0.40% PTEN Q245* 0.20% PTEN Q245* 0.30% PIK3CA E726K 1.50% PIK3CA E245Q 0.10% PIK3CA M1043I 0.36% PIK3CA M1043I 1.20% TP53 E180K 11.80% PIK3CA E453K 0.25% PLCG2 P737T PLCG2 P737T PIK3CA E726K VHL E173Q 1.10% RB1 R556* 3.10% TP53 E180K 11.00% PIK3CA E726K 0.20% PIK3CA E726K 0.23% PIK3CA E726K 0.44% TP53 I195F 1.20% PIK3CA E39Q 0.53% CDKN1B Q163* PIK3CA M1004I MET S1061F MET L229F 0.30% CCND1 E9K 0.10% PTEN Q245* 0.80% TP53 E180K 7.30% TP53 E180K 24.28% TP53 E180K 35.40% TP53 L137Q 1.30% TP53 E180K 38.40% ERBB2 R487W PTEN S229* TBX3 S435* MET W112C 1.20% NF1 D1556N 1.30% TP53 I195F 0.20% TP53 R175G 0.20% TP53 I195F 1.70% ESR1 E380Q 7.10% TP53 I195F 0.56% ALK E1407K RB1 Q217* SPEN Q743* NF1 R1176T 1.00% NF1 E76K 0.30% ESR1 E380Q 0.90% TP53 I195F 1.37% TP53 L137Q 2.10% ESR1 L391V 0.41% TP53 I254M 0.25% APC E2637K PIK3CA D1017N PTEN I253M VHL E173Q 1.20% RB1 R556* 7.20% NF1 R1176T 0.50% TP53 -

Clinical, Molecular, and Immune Analysis of Dabrafenib-Trametinib
Supplementary Online Content Chen G, McQuade JL, Panka DJ, et al. Clinical, molecular and immune analysis of dabrafenib-trametinib combination treatment for metastatic melanoma that progressed during BRAF inhibitor monotherapy: a phase 2 clinical trial. JAMA Oncology. Published online April 28, 2016. doi:10.1001/jamaoncol.2016.0509. eMethods. eReferences. eTable 1. Clinical efficacy eTable 2. Adverse events eTable 3. Correlation of baseline patient characteristics with treatment outcomes eTable 4. Patient responses and baseline IHC results eFigure 1. Kaplan-Meier analysis of overall survival eFigure 2. Correlation between IHC and RNAseq results eFigure 3. pPRAS40 expression and PFS eFigure 4. Baseline and treatment-induced changes in immune infiltrates eFigure 5. PD-L1 expression eTable 5. Nonsynonymous mutations detected by WES in baseline tumors This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/30/2021 eMethods Whole exome sequencing Whole exome capture libraries for both tumor and normal samples were constructed using 100ng genomic DNA input and following the protocol as described by Fisher et al.,3 with the following adapter modification: Illumina paired end adapters were replaced with palindromic forked adapters with unique 8 base index sequences embedded within the adapter. In-solution hybrid selection was performed using the Illumina Rapid Capture Exome enrichment kit with 38Mb target territory (29Mb baited). The targeted region includes 98.3% of the intervals in the Refseq exome database. Dual-indexed libraries were pooled into groups of up to 96 samples prior to hybridization. -
An Analysis About Heterogeneity Among Cancers Based on the DNA Methylation Patterns
An analysis about heterogeneity among cancers based on the DNA Methylation Patterns Yang Liu Harbin Institute of Technology Yue Gu Harbin Medical University Mu Su Harbin Institute of Technology Hui Liu Harbin Institute of Technology Shumei Zhang Harbin Medical University Yan Zhang ( [email protected] ) Harbin Institute of Technology https://orcid.org/0000-0002-5307-2484 Research article Keywords: DNA methylation, cancer, epigenetic heterogeneity, survival analysis Posted Date: July 17th, 2019 DOI: https://doi.org/10.21203/rs.2.11636/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published at BMC Cancer on December 1st, 2019. See the published version at https://doi.org/10.1186/s12885-019-6455-x. Page 1/28 Abstract Background: The occurrence of cancer is usually the result of a co-effect of genetic and environmental factors. It is generally believed that the main cause of cancer is the accumulation of genetic mutations, and DNA methylation, as one of the epigenetic modications closely related to environmental factors, participates in the regulation of gene expression and cell differentiation and plays an important role in the development of cancer. Methods: This article discusses the epigenetic heterogeneity of cancer in detail. Firstly DNA methylation data of 7 cancer types were obtained from Illumina Innium HumanMethylation 450K platform of TCGA database. Diagnostic markers of each cancer were obtained by t-test and absolute difference of DNA differencial methylation analysis. Enrichment analysis of these specic markers indicated that they were involved in different biological functions. -

AKT-Mtor Signaling in Human Acute Myeloid Leukemia Cells and Its Association with Adverse Prognosis
Cancers 2018, 10, 332 S1 of S35 Supplementary Materials: Clonal Heterogeneity Reflected by PI3K- AKT-mTOR Signaling in Human Acute Myeloid Leukemia Cells and its Association with Adverse Prognosis Ina Nepstad, Kimberley Joanne Hatfield, Tor Henrik Anderson Tvedt, Håkon Reikvam and Øystein Bruserud Figure S1. Detection of clonal heterogeneity for 49 acute myeloid leukemia (AML) patients; the results from representative flow cytometric analyses of phosphatidylinositol-3-kinase-Akt-mechanistic target of rapamycin (PI3K-Akt-mTOR) activation. For each patient clonal heterogeneity was detected by analysis Cancers 2018, 10, 332 S2 of S35 of at least one mediator in the PI3K-Akt-mTOR pathway. Patient ID is shown in the upper right corner of each histogram. The figure documents the detection of dual populations for all patients, showing the results from one representative flow cytometric analysis for each of these 49 patients. The Y-axis represents the amount of cells, and the X-axis represents the fluorescence intensity. The stippled line shows the negative/unstained controls. Figure S2. Cell preparation and gating strategy. Flow cytometry was used for examination of the constitutive expression of the mediators in the PI3K-Akt-mTOR pathway/network in primary AML cells. Cryopreserved cells were thawed and washed before suspension cultures were prepared as described in Materials and methods. Briefly, cryopreserved and thawed primary leukemic cells were incubated for 20 minutes in RPMI-1640 (Sigma-Aldrich) before being directly fixed in 1.5% paraformaldehyde (PFA) and permeabilized with 100% ice-cold methanol. The cells were thereafter rehydrated by adding 2 mL phosphate buffered saline (PBS), gently re-suspended and then centrifuged. -

The Hypothalamus As a Hub for SARS-Cov-2 Brain Infection and Pathogenesis
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.08.139329; this version posted June 19, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. The hypothalamus as a hub for SARS-CoV-2 brain infection and pathogenesis Sreekala Nampoothiri1,2#, Florent Sauve1,2#, Gaëtan Ternier1,2ƒ, Daniela Fernandois1,2 ƒ, Caio Coelho1,2, Monica ImBernon1,2, Eleonora Deligia1,2, Romain PerBet1, Vincent Florent1,2,3, Marc Baroncini1,2, Florence Pasquier1,4, François Trottein5, Claude-Alain Maurage1,2, Virginie Mattot1,2‡, Paolo GiacoBini1,2‡, S. Rasika1,2‡*, Vincent Prevot1,2‡* 1 Univ. Lille, Inserm, CHU Lille, Lille Neuroscience & Cognition, DistAlz, UMR-S 1172, Lille, France 2 LaBoratorY of Development and PlasticitY of the Neuroendocrine Brain, FHU 1000 daYs for health, EGID, School of Medicine, Lille, France 3 Nutrition, Arras General Hospital, Arras, France 4 Centre mémoire ressources et recherche, CHU Lille, LiCEND, Lille, France 5 Univ. Lille, CNRS, INSERM, CHU Lille, Institut Pasteur de Lille, U1019 - UMR 8204 - CIIL - Center for Infection and ImmunitY of Lille (CIIL), Lille, France. # and ƒ These authors contriButed equallY to this work. ‡ These authors directed this work *Correspondence to: [email protected] and [email protected] Short title: Covid-19: the hypothalamic hypothesis 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.06.08.139329; this version posted June 19, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity.