Characterisation of the First Specific Inhibitor of Ceramide Synthase 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

P53 and Ceramide As Collaborators in the Stress Response
Int. J. Mol. Sci. 2013, 14, 4982-5012; doi:10.3390/ijms14034982 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review p53 and Ceramide as Collaborators in the Stress Response Rouba Hage-Sleiman 1,2,*, Maria O. Esmerian 1,2, Hadile Kobeissy 2 and Ghassan Dbaibo 1,2 1 Department of Pediatrics and Adolescent Medicine, Division of Pediatric Infectious Diseases, Faculty of Medicine, American University of Beirut, P.O. Box 11-0236 Riad El Solh, 1107 2020 Beirut, Lebanon; E-Mails: [email protected] (M.O.E.); [email protected] (G.D.) 2 Department of Biochemistry and Molecular Genetics, Faculty of Medicine, American University of Beirut, P.O. Box 11-0236 Riad El Solh, 1107 2020 Beirut, Lebanon; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +961-1-350-000 (ext. 4883). Received: 26 December 2012; in revised form: 22 January 2013 / Accepted: 1 February 2013 / Published: 1 March 2013 Abstract: The sphingolipid ceramide mediates various cellular processes in response to several extracellular stimuli. Some genotoxic stresses are able to induce p53-dependent ceramide accumulation leading to cell death. However, in other cases, in the absence of the tumor suppressor protein p53, apoptosis proceeds partly due to the activity of this “tumor suppressor lipid”, ceramide. In the current review, we describe ceramide and its roles in signaling pathways such as cell cycle arrest, hypoxia, hyperoxia, cell death, and cancer. In a specific manner, we are elaborating on the role of ceramide in mitochondrial apoptotic cell death signaling. -
Combination of Photodynamic Therapy with Fenretinide and C6
Wayne State University Wayne State University Theses 1-1-2015 Combination Of Photodynamic Therapy With Fenretinide And C6-Pyridinium Ceramide Enhances Killing Of Scc17b Human Head And Neck Squamous Cell Carcinoma Cells Via The eD Novo Sphingolipid Biosynthesis And Mitochondrial Apoptosis Nithin Bhargava Boppana Wayne State University, Follow this and additional works at: https://digitalcommons.wayne.edu/oa_theses Part of the Medicinal Chemistry and Pharmaceutics Commons Recommended Citation Boppana, Nithin Bhargava, "Combination Of Photodynamic Therapy With Fenretinide And C6-Pyridinium Ceramide Enhances Killing Of Scc17b Human Head And Neck Squamous Cell Carcinoma Cells Via The eD Novo Sphingolipid Biosynthesis And Mitochondrial Apoptosis" (2015). Wayne State University Theses. 431. https://digitalcommons.wayne.edu/oa_theses/431 This Open Access Thesis is brought to you for free and open access by DigitalCommons@WayneState. It has been accepted for inclusion in Wayne State University Theses by an authorized administrator of DigitalCommons@WayneState. COMBINATION OF PHOTODYNAMIC THERAPY WITH FENRETINIDE AND C6-PYRIDINIUM CERAMIDE ENHANCES KILLING OF SCC17B HUMAN HEAD AND NECK SQUAMOUS CELL CARCINOMA CELLS VIA THE DE NOVO SPHINGOLIPID BIOSYNTHESIS AND MITOCHONDRIAL APOPTOSIS by NITHIN BHARGAVA BOPPANA THESIS Submitted to the Graduate School of Wayne State University, Detroit, Michigan in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE 2015 MAJOR: PHARMACEUTICAL SCIENCES Approved By: ________________________________ Advisor Date © COPYRIGHT BY NITHIN BHARGAVA BOPPANA 2015 All Rights Reserved DEDICATION Dedicated to my mom Rekha Vasireddy for always believing in me and helping me in becoming the person who I am today. ii ACKNOWLEDGEMENTS I am grateful to my advisor, Dr. Duska Separovic for her invaluable mentorship throughout the project. -

Targeting Cancer Metabolism to Resensitize Chemotherapy: Potential Development of Cancer Chemosensitizers from Traditional Chinese Medicines
cancers Review Targeting Cancer Metabolism to Resensitize Chemotherapy: Potential Development of Cancer Chemosensitizers from Traditional Chinese Medicines Wei Guo, Hor-Yue Tan, Feiyu Chen, Ning Wang and Yibin Feng * School of Chinese Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR 00000, China; [email protected] (W.G.); [email protected] (H.-Y.T.); [email protected] (F.C.); [email protected] (N.W.) * Correspondence: [email protected] Received: 22 December 2019; Accepted: 3 February 2020; Published: 10 February 2020 Abstract: Cancer is a common and complex disease with high incidence and mortality rates, which causes a severe public health problem worldwide. As one of the standard therapeutic approaches for cancer therapy, the prognosis and outcome of chemotherapy are still far from satisfactory due to the severe side effects and increasingly acquired resistance. The development of novel and effective treatment strategies to overcome chemoresistance is urgent for cancer therapy. Metabolic reprogramming is one of the hallmarks of cancer. Cancer cells could rewire metabolic pathways to facilitate tumorigenesis, tumor progression, and metastasis, as well as chemoresistance. The metabolic reprogramming may serve as a promising therapeutic strategy and rekindle the research enthusiasm for overcoming chemoresistance. This review focuses on emerging mechanisms underlying rewired metabolic pathways for cancer chemoresistance in terms of glucose and energy, lipid, amino acid, and nucleotide metabolisms, as well as other related metabolisms. In particular, we highlight the potential of traditional Chinese medicine as a chemosensitizer for cancer chemotherapy from the metabolic perspective. The perspectives of metabolic targeting to chemoresistance are also discussed. -

Inherited Monogenic Defects of Ceramide Metabolism Molecular
Clinica Chimica Acta 495 (2019) 457–466 Contents lists available at ScienceDirect Clinica Chimica Acta journal homepage: www.elsevier.com/locate/cca Review Inherited monogenic defects of ceramide metabolism: Molecular bases and diagnoses T ⁎⁎ Patricia Dubota,b, Frédérique Sabourdya,b, Jitka Rybovac,Jeffrey A. Medinc,d, , ⁎ Thierry Levadea,b, a Laboratoire de Biochimie Métabolique, Centre de Référence en Maladies Héréditaires du Métabolisme, Institut Fédératif de Biologie, CHU de Toulouse, Toulouse, France b INSERM UMR1037, CRCT (Cancer Research Center of Toulouse), Université Paul Sabatier, Toulouse, France c Department of Pediatrics, Medical College of Wisconsin, Milwaukee, WI, USA d Department of Biochemistry, Medical College of Wisconsin, Milwaukee, WI, USA ABSTRACT Ceramides are membrane lipids implicated in the regulation of numerous biological functions. Recent evidence suggests that specific subsets of molecular species of ceramide may play distinct physiological roles. The importance of this family of molecules in vertebrates is witnessed by the deleterious consequences of genetic alterations in ceramide metabolism. This brief review summarizes the clinical presentation of human disorders due to the deficiency of enzymes involved either in the biosynthesis or the degradation of ceramides. Information on the possible underlying pathophysiological mechanisms is also provided, based on knowledge gathered from animal models of these inherited rare conditions. When appropriate, tools for chemical and molecular diagnosis of these disorders and therapeutic options are also presented. 1. Introduction/foreword relationships that are relevant for unraveling the biological role of these genes and gene products in humans. Studies on ceramides and sphingolipid metabolism have attracted a lot of attention recently. This is largely related to the multiplicity of 2. -

Správa O Činnosti Organizácie SAV Za Rok 2013
Ústav normálnej a patologickej fyziológie SAV Správa o činnosti organizácie SAV za rok 2013 Bratislava január 2014 Obsah osnovy Správy o činnosti organizácie SAV za rok 2013 1. Základné údaje o organizácii 2. Vedecká činnosť 3. Doktorandské štúdium, iná pedagogická činnosť a budovanie ľudských zdrojov pre vedu a techniku 4. Medzinárodná vedecká spolupráca 5. Vedná politika 6. Spolupráca s VŠ a inými subjektmi v oblasti vedy a techniky 7. Spolupráca s aplikačnou a hospodárskou sférou 8. Aktivity pre Národnú radu SR, vládu SR, ústredné orgány štátnej správy SR a iné organizácie 9. Vedecko-organizačné a popularizačné aktivity 10. Činnosť knižnično-informačného pracoviska 11. Aktivity v orgánoch SAV 12. Hospodárenie organizácie 13. Nadácie a fondy pri organizácii SAV 14. Iné významné činnosti organizácie SAV 15. Vyznamenania, ocenenia a ceny udelené pracovníkom organizácie SAV 16. Poskytovanie informácií v súlade so zákonom o slobodnom prístupe k informáciám 17. Problémy a podnety pre činnosť SAV PRÍLOHY A Zoznam zamestnancov a doktorandov organizácie k 31.12.2013 B Projekty riešené v organizácii C Publikačná činnosť organizácie D Údaje o pedagogickej činnosti organizácie E Medzinárodná mobilita organizácie Správa o činnosti organizácie SAV 1. Základné údaje o organizácii 1.1. Kontaktné údaje Názov: Ústav normálnej a patologickej fyziológie SAV Riaditeľ: RNDr. Oľga Pecháňová, DrSc. Zástupca riaditeľa: MUDr. Fedor Jagla, CSc. Vedecký tajomník: RNDr. Iveta Bernátová, DrSc. Predseda vedeckej rady: RNDr. Iveta Bernátová, DrSc. Členovia snemu SAV: MUDr. Fedor Jagla, CSc., MUDr. Igor Riečanský, PhD. Adresa: Sienkiewiczova 1, 813 71 Bratislava http://www.unpf.sav.sk Tel.: 02/32296063 Fax: E-mail: [email protected] Názvy a adresy detašovaných pracovísk: nie sú Vedúci detašovaných pracovísk: nie sú Typ organizácie: Rozpočtová od roku 1953 1.2. -

Acute and Chronic Complications
Uniwersytet Medyczny w Łodzi Medical University of Lodz https://publicum.umed.lodz.pl Higher Blood Glucose Variability is Associated with Increased Risk of Hypoglycemia Publikacja / Publication in Well or Poorly Controlled Type 1 or Type 2 Diabetes, Czupryniak Leszek, Borkowska Anna, Szymańska-Garbacz Elektra DOI wersji wydawcy / Published http://dx.doi.org/10.2337/db17-381-663 version DOI Adres publikacji w Repozytorium URL / Publication address in https://publicum.umed.lodz.pl/info/article/AML063ddbabfba14480a6e45b1d944e1ccd/ Repository Data opublikowania w Repozytorium 2020-08-31 / Deposited in Repository on Rodzaj licencji / Type of licence Other open licence Czupryniak Leszek, Borkowska Anna, Szymańska-Garbacz Elektra : Higher Blood Glucose Variability is Associated with Increased Risk of Hypoglycemia in Well or Cytuj tę wersję / Cite this version Poorly Controlled Type 1 or Type 2 Diabetes, Diabetes, vol. 66, no. Suppl. 1, 2017, pp. 103-104, DOI:10.2337/db17-381-663 COMPLICATIONS—HYPOGLYCEMIA COMPLICATIONS—HYPOGLYCEMIA an activating role of SAMSN1, L-triiodothyronine, IFNA4, JAK1 and mTORC1, and an inhibitory action of BDNF, POR, ESR1, CTNNB1 and ERG on the gene networks identified in our samples. Moderated Poster Discussion: Hypoglycemia—Novel Concepts Our study for the first time characterizes the transcriptional responses (Posters: 381-P to 386-P), see page 19. of the BBB compartment to recurrent hypoglycemia exposure and may help identify novel therapeutic targets to restore the impaired responses against 381‑P hypoglycemia in patients with type 1 diabetes. & Supported By: National Institutes of Health; JDRF Hypoglycemia‑Associated Autonomic Failure Is Associated with POSTERS Complications Coordinated miRNA‑mRNA Network Changes in the Ventromedial Acute and Chronic Hypothalamus & 383‑P RAHUL AGRAWAL, CASEY TAYLOR, ADRIANA VIEIRA-DE-ABREU, SIMON J. -

Enhancing Skin Health: by Oral Administration of Natural Compounds and Minerals with Implications to the Dermal Microbiome
Review Enhancing Skin Health: By Oral Administration of Natural Compounds and Minerals with Implications to the Dermal Microbiome David L. Vollmer 1, Virginia A. West 1 and Edwin D. Lephart 2,* 1 4Life Research, Scientific Research Division, Sandy, Utah 84070, USA; [email protected] (D.L.V.); [email protected] (V.A.W) 2 Department of Physiology, Developmental Biology and The Neuroscience Center, Brigham Young University, Provo, Utah 84602, USA * Correspondence: [email protected]; Tel.: +1-801-422-2006 Received: 23 August 2018; Accepted: 1 October 2018; Published: 7 October 2018 Abstract: The history of cosmetics goes back to early Egyptian times for hygiene and health benefits while the history of topical applications that provide a medicinal treatment to combat dermal aging is relatively new. For example, the term cosmeceutical was first coined by Albert Kligman in 1984 to describe topical products that afford both cosmetic and therapeutic benefits. However, beauty comes from the inside. Therefore, for some time scientists have considered how nutrition reflects healthy skin and the aging process. The more recent link between nutrition and skin aging began in earnest around the year 2000 with the demonstrated increase in peer-reviewed scientific journal reports on this topic that included biochemical and molecular mechanisms of action. Thus, the application of: (a) topical administration from outside into the skin and (b) inside by oral consumption of nutritionals to the outer skin layers is now common place and many journal reports exhibit significant improvement for both on a variety of dermal parameters. Therefore, this review covers, where applicable, the history, chemical structure, and sources such as biological and biomedical properties in the skin along with animal and clinical data on the oral applications of: (a) collagen, (b) ceramide, (c) β-carotene, (d) astaxanthin, (e) coenzyme Q10, (f) colostrum, (g) zinc, and (h) selenium in their mode of action or function in improving dermal health by various quantified endpoints. -
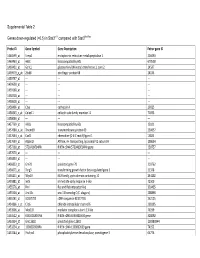
0.5) in Stat3∆/∆ Compared with Stat3flox/Flox
Supplemental Table 2 Genes down-regulated (<0.5) in Stat3∆/∆ compared with Stat3flox/flox Probe ID Gene Symbol Gene Description Entrez gene ID 1460599_at Ermp1 endoplasmic reticulum metallopeptidase 1 226090 1460463_at H60c histocompatibility 60c 670558 1460431_at Gcnt1 glucosaminyl (N-acetyl) transferase 1, core 2 14537 1459979_x_at Zfp68 zinc finger protein 68 24135 1459747_at --- --- --- 1459608_at --- --- --- 1459168_at --- --- --- 1458718_at --- --- --- 1458618_at --- --- --- 1458466_at Ctsa cathepsin A 19025 1458345_s_at Colec11 collectin sub-family member 11 71693 1458046_at --- --- --- 1457769_at H60a histocompatibility 60a 15101 1457680_a_at Tmem69 transmembrane protein 69 230657 1457644_s_at Cxcl1 chemokine (C-X-C motif) ligand 1 14825 1457639_at Atp6v1h ATPase, H+ transporting, lysosomal V1 subunit H 108664 1457260_at 5730409E04Rik RIKEN cDNA 5730409E04Rik gene 230757 1457070_at --- --- --- 1456893_at --- --- --- 1456823_at Gm70 predicted gene 70 210762 1456671_at Tbrg3 transforming growth factor beta regulated gene 3 21378 1456211_at Nlrp10 NLR family, pyrin domain containing 10 244202 1455881_at Ier5l immediate early response 5-like 72500 1455576_at Rinl Ras and Rab interactor-like 320435 1455304_at Unc13c unc-13 homolog C (C. elegans) 208898 1455241_at BC037703 cDNA sequence BC037703 242125 1454866_s_at Clic6 chloride intracellular channel 6 209195 1453906_at Med13l mediator complex subunit 13-like 76199 1453522_at 6530401N04Rik RIKEN cDNA 6530401N04 gene 328092 1453354_at Gm11602 predicted gene 11602 100380944 1453234_at -

Table SI. Primer List of Genes Used for Reverse Transcription‑Quantitative PCR Validation
Table SI. Primer list of genes used for reverse transcription‑quantitative PCR validation. Genes Forward (5'‑3') Reverse (5'‑3') Length COL1A1 AGTGGTTTGGATGGTGCCAA GCACCATCATTTCCACGAGC 170 COL6A1 CCCCTCCCCACTCATCACTA CGAATCAGGTTGGTCGGGAA 65 COL2A1 GGTCCTGCAGGTGAACCC CTCTGTCTCCTTGCTTGCCA 181 DCT CTACGAAACCAGGATGACCGT ACCATCATTGGTTTGCCTTTCA 192 PDE4D ATTGCCCACGATAGCTGCTC GCAGATGTGCCATTGTCCAC 181 RP11‑428C19.4 ACGCTAGAAACAGTGGTGCG AATCCCCGGAAAGATCCAGC 179 GPC‑AS2 TCTCAACTCCCCTCCTTCGAG TTACATTTCCCGGCCCATCTC 151 XLOC_110310 AGTGGTAGGGCAAGTCCTCT CGTGGTGGGATTCAAAGGGA 187 COL1A1, collagen type I alpha 1; COL6A1, collagen type VI, alpha 1; COL2A1, collagen type II alpha 1; DCT, dopachrome tautomerase; PDE4D, phosphodiesterase 4D cAMP‑specific. Table SII. The differentially expressed mRNAs in the ParoAF_Control group. Gene ID logFC P‑Value Symbol Description ENSG00000165480 ‑6.4838 8.32E‑12 SKA3 Spindle and kinetochore associated complex subunit 3 ENSG00000165424 ‑6.43924 0.002056 ZCCHC24 Zinc finger, CCHC domain containing 24 ENSG00000182836 ‑6.20215 0.000817 PLCXD3 Phosphatidylinositol‑specific phospholipase C, X domain containing 3 ENSG00000174358 ‑5.79775 0.029093 SLC6A19 Solute carrier family 6 (neutral amino acid transporter), member 19 ENSG00000168916 ‑5.761 0.004046 ZNF608 Zinc finger protein 608 ENSG00000134343 ‑5.56371 0.01356 ANO3 Anoctamin 3 ENSG00000110400 ‑5.48194 0.004123 PVRL1 Poliovirus receptor‑related 1 (herpesvirus entry mediator C) ENSG00000124882 ‑5.45849 0.022164 EREG Epiregulin ENSG00000113448 ‑5.41752 0.000577 PDE4D Phosphodiesterase -
HCC and Cancer Mutated Genes Summarized in the Literature Gene Symbol Gene Name References*
HCC and cancer mutated genes summarized in the literature Gene symbol Gene name References* A2M Alpha-2-macroglobulin (4) ABL1 c-abl oncogene 1, receptor tyrosine kinase (4,5,22) ACBD7 Acyl-Coenzyme A binding domain containing 7 (23) ACTL6A Actin-like 6A (4,5) ACTL6B Actin-like 6B (4) ACVR1B Activin A receptor, type IB (21,22) ACVR2A Activin A receptor, type IIA (4,21) ADAM10 ADAM metallopeptidase domain 10 (5) ADAMTS9 ADAM metallopeptidase with thrombospondin type 1 motif, 9 (4) ADCY2 Adenylate cyclase 2 (brain) (26) AJUBA Ajuba LIM protein (21) AKAP9 A kinase (PRKA) anchor protein (yotiao) 9 (4) Akt AKT serine/threonine kinase (28) AKT1 v-akt murine thymoma viral oncogene homolog 1 (5,21,22) AKT2 v-akt murine thymoma viral oncogene homolog 2 (4) ALB Albumin (4) ALK Anaplastic lymphoma receptor tyrosine kinase (22) AMPH Amphiphysin (24) ANK3 Ankyrin 3, node of Ranvier (ankyrin G) (4) ANKRD12 Ankyrin repeat domain 12 (4) ANO1 Anoctamin 1, calcium activated chloride channel (4) APC Adenomatous polyposis coli (4,5,21,22,25,28) APOB Apolipoprotein B [including Ag(x) antigen] (4) AR Androgen receptor (5,21-23) ARAP1 ArfGAP with RhoGAP domain, ankyrin repeat and PH domain 1 (4) ARHGAP35 Rho GTPase activating protein 35 (21) ARID1A AT rich interactive domain 1A (SWI-like) (4,5,21,22,24,25,27,28) ARID1B AT rich interactive domain 1B (SWI1-like) (4,5,22) ARID2 AT rich interactive domain 2 (ARID, RFX-like) (4,5,22,24,25,27,28) ARID4A AT rich interactive domain 4A (RBP1-like) (28) ARID5B AT rich interactive domain 5B (MRF1-like) (21) ASPM Asp (abnormal -
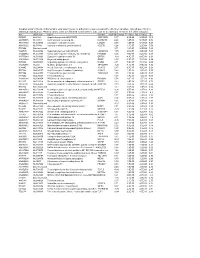
Supplementary File 2A Revised
Supplementary file 2A. Differentially expressed genes in aldosteronomas compared to all other samples, ranked according to statistical significance. Missing values were not allowed in aldosteronomas, but to a maximum of five in the other samples. Acc UGCluster Name Symbol log Fold Change P - Value Adj. P-Value B R99527 Hs.8162 Hypothetical protein MGC39372 MGC39372 2,17 6,3E-09 5,1E-05 10,2 AA398335 Hs.10414 Kelch domain containing 8A KLHDC8A 2,26 1,2E-08 5,1E-05 9,56 AA441933 Hs.519075 Leiomodin 1 (smooth muscle) LMOD1 2,33 1,3E-08 5,1E-05 9,54 AA630120 Hs.78781 Vascular endothelial growth factor B VEGFB 1,24 1,1E-07 2,9E-04 7,59 R07846 Data not found 3,71 1,2E-07 2,9E-04 7,49 W92795 Hs.434386 Hypothetical protein LOC201229 LOC201229 1,55 2,0E-07 4,0E-04 7,03 AA454564 Hs.323396 Family with sequence similarity 54, member B FAM54B 1,25 3,0E-07 5,2E-04 6,65 AA775249 Hs.513633 G protein-coupled receptor 56 GPR56 -1,63 4,3E-07 6,4E-04 6,33 AA012822 Hs.713814 Oxysterol bining protein OSBP 1,35 5,3E-07 7,1E-04 6,14 R45592 Hs.655271 Regulating synaptic membrane exocytosis 2 RIMS2 2,51 5,9E-07 7,1E-04 6,04 AA282936 Hs.240 M-phase phosphoprotein 1 MPHOSPH -1,40 8,1E-07 8,9E-04 5,74 N34945 Hs.234898 Acetyl-Coenzyme A carboxylase beta ACACB 0,87 9,7E-07 9,8E-04 5,58 R07322 Hs.464137 Acyl-Coenzyme A oxidase 1, palmitoyl ACOX1 0,82 1,3E-06 1,2E-03 5,35 R77144 Hs.488835 Transmembrane protein 120A TMEM120A 1,55 1,7E-06 1,4E-03 5,07 H68542 Hs.420009 Transcribed locus 1,07 1,7E-06 1,4E-03 5,06 AA410184 Hs.696454 PBX/knotted 1 homeobox 2 PKNOX2 1,78 2,0E-06 -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase