New General Manager for Raigmore Hospital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Contract Between Scottish Ministers
CONTRACT BETWEEN SCOTTISH MINISTERS AND GEOAMEY PECS LTD FOR THE SCOTTISH COURT CUSTODY AND PRISONER ESCORT SERVICE (SCCPES) REFERENCE: 01500 MARCH 2018 Official No part of this document may be disclosed orally or in writing, including by reproduction, to any third party without the prior written consent of SPS. This document, its associated appendices and any attachments remain the property of SPS and will be returned upon request. 1 | P a g e 01500 Scottish Court Custody and Prisoner Escort Service (SCCPES) FORM OF CONTRACT CONTRACT No. 01500 This Contract is entered in to between: The Scottish Ministers, referred to in the Scotland Act 1998, represented by the Scottish Prison Service at the: Scottish Prison Service Calton House 5 Redheughs Rigg Edinburgh EH12 9HW (hereinafter called the “Purchaser”) OF THE FIRST PART And GEOAmey PECS Ltd (07556404) The Sherard Building, Edmund Halley Road Oxford OX4 4DQ (hereinafter called the “Service Provider”) OF THE SECOND PART The Purchaser hereby appoints the Service Provider and the Service Provider hereby agrees to provide for the Purchaser, the Services (as hereinafter defined) on the Conditions of Contract set out in this Contract. The Purchaser agrees to pay to the Service Provider the relevant sums specified in Schedule C and due in terms of the Contract, in consideration of the due and proper performance by the Service Provider of its obligations under the Contract. The Service Provider agrees to look only to the Purchaser for the due performance of the Contract and the Purchaser will be entitled to enforce this Contract on behalf of the Scottish Ministers. -

Accident and Emergency: Performance Update
Accident and Emergency Performance update Prepared by Audit Scotland May 2014 Auditor General for Scotland The Auditor General’s role is to: • appoint auditors to Scotland’s central government and NHS bodies • examine how public bodies spend public money • help them to manage their finances to the highest standards • check whether they achieve value for money. The Auditor General is independent and reports to the Scottish Parliament on the performance of: • directorates of the Scottish Government • government agencies, eg the Scottish Prison Service, Historic Scotland • NHS bodies • further education colleges • Scottish Water • NDPBs and others, eg Scottish Police Authority, Scottish Fire and Rescue Service. You can find out more about the work of the Auditor General on our website: www.audit-scotland.gov.uk/about/ags Audit Scotland is a statutory body set up in April 2000 under the Public Finance and Accountability (Scotland) Act 2000. We help the Auditor General for Scotland and the Accounts Commission check that organisations spending public money use it properly, efficiently and effectively. Accident and Emergency | 3 Contents Summary 4 Key messages 7 Part 1. A&E waiting times 9 Part 2. Reasons for delays in A&E 20 Part 3. Action by the Scottish Government 37 Endnotes 41 Appendix 1. NHS Scotland A&E departments and minor injury units 43 Appendix 2. National context for A&E and unscheduled care, 2004 to 2014 45 Exhibit data When viewing this report online, you can access background data by clicking on the graph icon. The data file will -

NHS Highland Board November 2019 Item 6 CHIEF EXECUTIVE AND
NHS Highland Board November 2019 Item 6 CHIEF EXECUTIVE AND DIRECTORS REPORT – EMERGING ISSUES AND UPDATES Report by Iain Stewart, Chief Executive The Board is asked to: • Note the updates provided in the report. Introduction from CEO The engagement strategy which is helping to shape the ‘Culture Fit for the Future’ has been moving ahead. Fiona Hogg will be giving a detailed update on our progress with our Culture Programme later in the agenda. I am pleased with the progress which is being made, it’s a long-term piece of work which needs careful research and planning to make sure we understand the problems we need to address. There are some key milestones being achieved and presented at this Board meeting. A governance structure is in place and our revised plans are ready to be agreed and rolled out. Many of the actions planned have been shaped by our ongoing engagement with the Board and with our colleagues across North Highland and Argyll & Bute and I’m delighted that our impending review in Argyll & Bute is going to provide further valuable insights and information. In terms of the cost improvement programme, we continue to make good progress, with the current level of identified opportunities valued at £29M which when adjusted for the likelihood of delivery reduces to £22M. Of particular note is that 80% of the forecast savings are recurrent so the savings gain will benefit future financial years. Workstreams are ensuring the remaining plans in this financial year are approved, that ideas are progressed to plans and that changes already implemented go on to deliver the expected savings. -

8-12 Weeks Questionnaire
Scottish Government Maternal and Infant Nutrition Survey Investigating health care and early feeding choices and experiences in the first 12 weeks following the birth of your new baby This is a survey about your choices and experiences in the first 12 weeks following the birth of your new baby. Please complete this questionnaire with respect to your baby who was born between March and April 2017. The information you provide will help us to understand more about the choices new parents make and help health care professionals to better support new parents. All of the answers you provide will be entirely confidential. Please read the enclosed letter for more information about this survey. Instructions The survey takes around 15-20 minutes to complete. Please answer all questions, unless the instructions ask you to skip a question. For most questions, you will be asked to put a tick in the box next to the statement which most applies to you. For example, if your answer is yes, write in a tick as below: P Yes No Don’t worry if you make a mistake; just cross it out and tick the correct answer. Sometimes you will be asked to write in a number. Please enter numbers as figures rather than words. For example: 6 Weeks 2 Days If you prefer, you can complete this survey online at: survey.natcen.ac.uk/MINS5 You will be asked to enter the User Code that can be found on the letter that came with this survey. Alternatively, you can give your answers by calling the FREEPHONE survey helpline on 0800 652 4568. -

Emergency Departments
ED Site List 220711 v2.xls NHS Scotland - Emergency Departments Table 1: NHS Scotland - list of sites providing emergency care File NHS Board Site Type Location Name Location Address Comments Type Ayrshire & Arran ED Ayr Hospital DALMELLINGTON ROAD, AYR, KA6 6DX E Crosshouse Hospital KILMARNOCK ROAD, KILMARNOCK, AYRSHIRE, KA2 0BE E MIU/Other Arran War Memorial Hospital LAMLASH, ISLE OF ARRAN, KA27 8LF A Davidson Cottage Hospital THE AVENUE, GIRVAN, KA26 9DS A Closed from May-10 Girvan Community Hospital BRIDGEMILL, GIRVAN, AYRSHIRE, KA26 9HQ A Opened from May-10 Lady Margaret Hospital COLLEGE ST, MILLPORT, ISLE OF CUMBRAE, KA28 0HF A Opened from Oct-07 Borders ED Borders General Hospital MELROSE, TD6 9BS E MIU/Other Hawick Cottage Hospital VICTORIA ROAD, HAWICK, TD9 7AH A Hay Lodge Hospital NEIDPATH ROAD, PEEBLES, EH45 8JG A Kelso Hospital INCH ROAD, KELSO, TD5 7JP A Knoll Hospital STATION ROAD, DUNS, TD11 3EL A Dumfries & Galloway ED Dumfries & Galloway Royal Infirmary BANKEND ROAD, DUMFRIES, DG1 4AP E Galloway Community Hospital DALRYMPLE STREET, STRANRAER, DG9 7DQ E MIU/Other Castle Douglas Hospital ACADEMY STREET, CASTLE DOUGLAS, DG7 1EE A Kirkcudbright Hospital TOWNEND, KIRKCUDBRIGHT, DG6 4BE A Moffat Hospital HOLMEND, MOFFAT, DG10 9JY A Newton Stewart Hospital NEWTON STEWART, DG8 6LZ A Fife ED Victoria Hospital HAYFIELD ROAD, KIRKCALDY, KY2 5AH E MIU/Other Adamson Hospital BANK STREET, CUPAR, KY15 4JG A Queen Margaret Hospital WHITEFIELD ROAD, DUNFERMLINE, KY12 0SU E St Andrews Memorial Hospital ABBEY WALK, ST ANDREWS, KY16 9LG -

Emergency Departments
ED-site-list NHS Scotland - Emergency Departments Table 1: NHS Scotland - list of sites providing emergency care NHS Board Site Type Location Name Location Address File Type Comments Ayrshire & Arran ED Ayr Hospital DALMELLINGTON ROAD, AYR, KA6 6DX E Crosshouse Hospital KILMARNOCK ROAD, KILMARNOCK, AYRSHIRE, KA2 0BE E MIU/Other Arran War Memorial Hospital LAMLASH, ISLE OF ARRAN, KA27 8LF A Davidson Cottage Hospital THE AVENUE, GIRVAN, KA26 9DS A Closed from May-10 Girvan Community Hospital BRIDGEMILL, GIRVAN, AYRSHIRE, KA26 9HQ A Opened from May-10 Lady Margaret Hospital COLLEGE ST, MILLPORT, ISLE OF CUMBRAE, KA28 0HF A Opened from Oct-07 Borders ED Borders General Hospital MELROSE, TD6 9BS E MIU/Other Hawick Cottage Hospital VICTORIA ROAD, HAWICK, TD9 7AH A Hay Lodge Hospital NEIDPATH ROAD, PEEBLES, EH45 8JG A Kelso Hospital INCH ROAD, KELSO, TD5 7JP A Knoll Hospital STATION ROAD, DUNS, TD11 3EL A Dumfries & Galloway ED Dumfries & Galloway Royal Infirmary BANKEND ROAD, DUMFRIES, DG1 4AP E Galloway Community Hospital DALRYMPLE STREET, STRANRAER, DG9 7DQ E MIU/Other Castle Douglas Hospital ACADEMY STREET, CASTLE DOUGLAS, DG7 1EE A Kirkcudbright Hospital TOWNEND, KIRKCUDBRIGHT, DG6 4BE A Moffat Hospital HOLMEND, MOFFAT, DG10 9JY A Newton Stewart Hospital NEWTON STEWART, DG8 6LZ A Fife ED Queen Margaret Hospital WHITEFIELD ROAD, DUNFERMLINE, KY12 0SU E Victoria Hospital HAYFIELD ROAD, KIRKCALDY, KY2 5AH E MIU/Other Adamson Hospital BANK STREET, CUPAR, KY15 4JG A St Andrews Memorial Hospital ABBEY WALK, ST ANDREWS, KY16 9LG A Forth Valley -

Cowal Fellowship
FEBRUARY 2021 RURAL FELLOWSHIPS Fellowships available for: Skye and Lochalsh Lochaber Caithness and Sutherland Torrisdale Bay Three Unique Experiences These innovative one-year fellowships will link both with GP practices and established teams of Advanced Nurse Practitioners for a multi-disciplinary educational experience in a rural setting. Rural Fellows are usually allocated one base practice, plus two or three practices, where they will provide the majority of their service commitment. These practices will be agreed as the beginning of the rural fellow year, with a view to providing the opportunity to experience all aspects of rural General Practice. Assynt The Rural Support Team A unique feature of these fellowships is the connection with our Rural Support Teams. The teams in all three areas consist of a mix of healthcare professionals; GPs, Advanced Nurse Practitioners, Unscheduled Nurse Practitioners and Paramedic Practitioners, all these disciplines either work or will work together providing healthcare to the populations within the North & West Division. The fellow would be supported to engage with the teams, providing a completely new perspective on the provision of services in rural areas – for the benefit of both the fellow and the teams! More at bit.ly/2UuUYzq Torrisdale Bay 13 Weeks Education Educational opportunities are flexible and too many to list. The fellow's educational plan will be organised in conjunction with the service elements of the posts and with support from with the Rural Fellowship Co-ordinator. Fellows will have the opportunity to negotiate additional experience in secondary care, remote practices and to undertake specific course activity as available. -

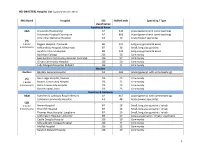
SAP Crystal Reports
10/02/2017 FOI Act Report - Asbestos Removal / Repair Works By Company and Year - Maximo 7.1 CARYMAR- Carymar Construction Services Limited 2012 Order Number Order Description Location GL Account Number Order Date Total Cost HES 10135 Removal of asbestos HAR 038-HE 039-3099 15/11/2012 £ 4,884.00 HES 10627 Refurbishment Survey - Islay Hospital H99999-H9997-A411-HCNH 0203 12/12/2012 £ 1,368.00 HES 8049 4 No Asbestos Samples HAR 038-HE 039-3019 19/07/2012 £ 180.00 2013 Order Number Order Description Location GL Account Number Order Date Total Cost HES 11462 Asbestos sample HAR 038-HE 039-3099 06/02/2013 £ 132.00 2015 Order Number Order Description Location GL Account Number Order Date Total Cost HES 27525 Asbestos Removal - VICC, Helensburgh CB -H42 HAC 038-HE 049-3019 09/09/2015 £ 6,936.00 NASBESTOS- NORTHERN ASBESTOS SERVICES LTD 2011 Order Number Order Description Location GL Account Number Order Date Total Cost HES 1279 Please take sample of dust from X-Ray extract fan and test for Asbestos RG -H28 HNC 113-H1901-3019 20/05/2011 £ 60.00 HES 1782 Take sample of dust from X-Ray extract fan & test for asbestos. RG -H28 HNC 113-H1901-3019 28/06/2011 £ 60.00 HES 2772 Removal of asbestos ceiling tiles, Room 8, Outpatients Clinic, Raigmore RG -H28 HNR 143-H4894-3019 15/09/2011 £ 4,895.60 2012 Order Number Order Description Location GL Account Number Order Date Total Cost HES 10854 To carry out asbestos Pre-demolition/Refurbishment Survey of X-Ray Room 3, Raigmore H99999-H9997-A411-HCNH 0194 27/12/2012 £ 1,729.78 HES 10854 To carry out asbestos -
MASTER) Hospital List (Updated October 2015
HEI (MASTER) Hospital List (updated October 2015) NHS Board Hospital ISD Staffed beds Speciality / Type classification Ayrshire & Arran A&A University Hospital Ayr A2 343 Acute (general with some teaching) University Hospital Crosshouse A2 666 Acute (general with some teaching) Arran War Memorial Hospital A3 19 Acute (mixed speciality) (9) 3 acute Biggart Hospital, Prestwick B6 121 Long stay geriatric & acute 6 community Kirklandside Hospital, Kilmarnock B7 36 Small, long stay geriatric Ayrshire Central Hospital B8 142 Long stay geriatric & acute Davidson Cottage J26 26 Community East Ayrshire Community Hospital, Cumnock J26 57 Community Girvan Community Hospital J26 20 Community Lady Margaret Hospital, Millport J26 9 Community Borders Borders Borders General Hospital A2 265 Acute (general, with some teaching) (5) Hay Lodge Hospital, Peebles J26 23 Community 1 acute Hawick Community Hospital J26 22 Community 4 community Kelso Community Hospital J26 23 Community Knoll Hospital, Duns J26 23 Community Dumfries & Galloway D&G Dumfries & Galloway Royal Infirmary A2 367 Acute (general, with some teaching) Galloway Community Hospital A3 48 Acute (mixed speciality) (10) 2 acute Annan Hospital B7 18 Small, long stay geriatric / rehab 8 community Thornhill Hospital B7 13 Small, long stay geriatric / rehab Thomas Hope Hospital, Langholm B7 10 Small, long stay geriatric / rehab Lochmaben Hospital, Lockerbie B9 17 Long stay geriatric / rehab / psychiatry Castle Douglas Hospital J26 19 Community Kirkcudbright Cottage Hospital J26 9 Community Moffat Hospital J26 12 Community Newton Stewart Hospital J26 19 Community 1 HEI (MASTER) Hospital List (updated October 2015) Fife Fife Victoria Hospital, Kirkcaldy A2 621 Acute (general with some teaching) (7) Queen Margaret Hospital, Dunfermline A3 196 Acute (mixed speciality) 2 acute 5 community Cameron Hospital, Leven B7 95 Small, long stay geriatric Adamson Hospital, Cupar J26 19 Community Glenrothes Hospital J26 74 Community Randolph Wemyss Memorial Hospital J26 16 Community St. -

North and West Operational Unit Occupational Therapy & Physiotherapy Leadership and Management Structure – January 2015
North and West Operational Unit Occupational Therapy & Physiotherapy Leadership and Management structure – January 2015 Within North and West Unit we have leads for both Occupational Therapy and Physiotherapy who have area wide governance roles for these professions and they link into the Highland wide governance networks for their profession. All Allied Health Professional staff are professionally led by those listed in the tables below and operationally managed via an integrated team structure within districts which sit under an area and Unit level management structure to the Director of Operations. Our only Mental Health Occupational Therapist is operationally managed in the Mental Health Integrated Team but professionally reports to the Lead Occupational Therapist within their area. Name Profession Post Base Dawn Mohun OT North Area Professional Migdale Hospital Lead Cherry Grove Bonar Bridge IV24 3ER Kerry Watson OT West Area Professional Kyle Health Centre, Lead Station Road Kyle of Lochalsh IV40 8AE Liz Morrison Physio Acting West Area Fort Willian Health Centre Professional Lead Fort William Lochaber PH33 7AQ Shona Paterson Physio North Area Professional Lawson Memorial Hospital Lead Golspie Sutherland KW10 6SS South and Mid Unit Management Structure Within South & Mid we have Unit Leads for both Occupational Therapy and Physiotherapy who have unit wide governance roles for these professions and they link into the Highland wide governance networks for their profession. Community Physiotherapy and Occupational Therapy sits within -

ISARIC (International Severe Acute Respiratory and Emerging Infections Consortium)
medRxiv preprint doi: https://doi.org/10.1101/2020.07.17.20155218; this version posted July 14, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-ND 4.0 International license . ISARIC Clinical Data Report issued: 14 July 2021 International Severe Acute Respiratory and emerging Infections Consortium ISARIC Clinical Characterisation Group*^ *group members, participating institutions and funders are listed at end of report and at https://isaric.org/research/covid-19-clinical- research-resources/covid-19-data-management-hosting/covid-19-clinical-data-contributors-list/ ^Correspondence to: [email protected] 1 1 ISARIC, Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK Abstract ISARIC (International Severe Acute Respiratory and emerging Infections Consortium) partnerships and outbreak preparedness initiatives enabled the rapid launch of standardised clinical data collection on COVID-19 in Jan 2020. Extensive global uptake of this resource has resulted in a large, standardised collection of comprehensive clinical data from hundreds of sites across dozens of countries. Data are analysed regularly and reported publicly to inform patient care and public health response. This report, our 15th report, is a part of a series and includes the results of data analysis for data captured before 26 May 2021. The report marks a significant milestone – the submission of clinical data from over half a million individuals hospitalised with COVID-19. We thank all of the data contributors for their ongoing support. -

Scotland) 15 June 2021
Version 1.6 (Scotland) 15 June 2021 ISARIC/WHO Clinical Characterisation Protocol UK (Scotland) Recruitment Procedures for FRONTLINE CLINICAL RESEARCH STAFF The most up to date versions of the protocol and case report form are available at isaric4c.net/protocols/ A virtual site visit is available at isaric4c.net/virtual_site_visit/ AIM: Please recruit the following patients only: • Vaccine failure (positive COVID test - rather than displaying symptoms – >28d after having received a vaccine) • Reinfection (proven after proven) • Co-infection (flu/RSV) • COVID associated hyper inflammation (MIS-A/MIS-C/PINS-TS) at any age • Samples from patients with pathogens of public health interest including people identified as infected with SARS-CoV “variants of concern” • All children CONSENT: once the form is signed by a participant it is hazardous. To record consent, we suggest an independent witness observes the completed form then signs a fresh copy outside of the isolation area. Consent can also be obtained by telephone from participants or from relatives for proxy consent. RECRUITMENT PACKS: Sample collection kits will be supplied to sites. Sample collections kits can be requested from: [email protected] Each kit will have a specific kit ID number, with each component within showing this kit ID and its own respective component ID for audit purposes. Pods and bio-bags for shipping will also be supplied to sites. These can be requested from [email protected] OBTAIN SAMPLES according to the schedule. You can find out which tier you are operating at in the front page of the site file. If you have capacity to recruit at TIER 2: Day 1 2 3 4 5 6 7 8 9 28 days after discharge Samples R S S C Sample priority 1 2 3 4 R: recruitment sample; S: serial sample; C: convalescent sample.