Global Vaccination: Trends and U.S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gavi's Vaccine Investment Strategy
Gavi’s Vaccine Investment Strategy Deepali Patel THIRD WHO CONSULTATION ON GLOBAL ACTION PLAN FOR INFLUENZA VACCINES (GAP III) Geneva, Switzerland, 15-16 November 2016 www.gavi.org Vaccine Investment Strategy (VIS) Evidence-based approach to identifying new vaccine priorities for Gavi support Strategic investment Conducted every 5 years decision-making (rather than first-come- first-serve) Transparent methodology Consultations and Predictability of Gavi independent expert advice programmes for long- term planning by Analytical review of governments, industry evidence and modelling and donors 2 VIS is aligned with Gavi’s strategic cycle and replenishment 2011-2015 Strategic 2016-2020 Strategic 2021-2025 period period 2008 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021 2022 2023 2024 2025 RTS,S pilot funding decision VIS #1 VIS #2 VIS #3 MenA, YF mass campaigns, JE, HPV Cholera stockpile, Mid 2017 : vaccine ‘long list’ Rubella, Rabies/cholera studies, Oct 2017 : methodology Typhoid Malaria – deferred Jun 2018 : vaccine shortlist conjugate Dec 2018 : investment decisions 3 VIS process Develop Collect data Develop in-depth methodology and Apply decision investment decision framework for cases for framework with comparative shortlisted evaluation analysis vaccines criteria Phase I Narrow long list Phase II Recommend for Identify long list to higher priority Gavi Board of vaccines vaccines approval of selected vaccines Stakeholder consultations and independent expert review 4 Evaluation criteria (VIS #2 – 2013) Additional Health Implementation -

Safety of Immunization During Pregnancy a Review of the Evidence
Safety of Immunization during Pregnancy A review of the evidence Global Advisory Committee on Vaccine Safety © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. -
Pneumococcal Vaccine
Vaccines for Primary Care Pneumococcal, Shingles, Pertussis Devang Patel, M.D. Assistant Professor Chief of Service, MICU ID Service University of Maryland School of Medicine Pneumococcal Vaccine Pneumococcal Disease • 2nd most common cause of vaccine preventable death in the US • Major Syndromes – Pneumonia – Bacteremia – Meningitis Active Bacterial Core Surveillance (ABCs) Report Emerging Infections Program Network Streptococcus pneumoniae, 2010 (ORIG) Vaccine Target • Polysaccharide capsule allows bacteria to resist phagocytosis • Antibodies to capsule facilitate phagocytosis • >90 different pneumococcal capsular serotypes • Vaccines contain most common serotypes causing disease Pneumococcal Vaccines Pneumococcal Vaccines • Pneumococcal polysaccharide vaccine (PPSV23; Pneumovax) – Contains capsular polysaccharides – 23 most commonly infecting serotypes • Cause 60% of all pneumococcal infections in adults – Not recommended for children <2 due to poor immunogenicity of polysaccharides Pneumococcal Vaccines • Pneumococcal conjugate vaccine (PCV13, Prevnar) – Polysaccharides linked to nontoxic protein • higher antigenicity – Stimulates mucosal antibody • Eliminates nasal carriage in young children • Herd effect in adults – Reduction in PCV7 serotype disease >90% Prevnar 13 • 2000 - PCV7 approved for infants toddlers • 2010 - PCV13 recommended for infants and toddlers • 2012 – ACIP recommended PCV13 for high- risk adults • 2014 – recommended for adults >65 • 2018 – ACIP will revisit PCV13 use in adults – Childhood vaccines may eliminate -
Vaccination Certificate Information Version: 21 July 2021
معلومات عن شهادة التطعيم، بالعربية 中文疫苗接种凭证信息 Informations sur le certificat de vaccination en FRANÇAIS Информация о сертификате вакцинации на РУССКОМ ЯЗЫКЕ Información sobre el Certificado de Vacunación en ESPAÑOL UN SYSTEM-WIDE COVID-19 VACCINATION PROGRAMME VACCINATION CERTIFICATE INFORMATION VERSION: 21 JULY 2021 ABOUT THE UN SYSTEM-WIDE COVID-19 VACCINATION PROGRAMME The UN is committed to ensuring the protection of its personnel. Tasked by the Secretary-General, the Department of Operational Support (DOS) is leading a coordinated, UN-system-wide effort to ensure the availability of vaccine to UN personnel, their dependents and implementing partners. The roll-out of the UN System-wide COVID-19 Vaccination Programme (the “Programme”) for UN personnel will provide a significant boost to the ability of personnel to stay and deliver on the Organization's mandates, to support beneficiaries in the communities they serve, and to contribute to our on-going work to recover better together from the pandemic. Information about the Programme is available at: https://www.un.org/en/coronavirus/vaccination ABOUT THE VACCINATION CERTIFICATE Upon administration of the requisite vaccine dosage, a certificate of vaccination is generated through the Programme’s registration platform (the “Platform”). The certificate generated by the Platform uses a standardized format, similar to the one used by the WHO in its “International Certificate of Vaccination or Prophylaxis” (Yellow) vaccination booklet. Note: This certificate may not dispense with travel restrictions put in place by the country(ies) of destination. As the nature of the pandemic continues to rapidly evolve, it is highly advisable to check the latest travel regulations. -

Global Dynamics of a Vaccination Model for Infectious Diseases with Asymptomatic Carriers
MATHEMATICAL BIOSCIENCES doi:10.3934/mbe.2016019 AND ENGINEERING Volume 13, Number 4, August 2016 pp. 813{840 GLOBAL DYNAMICS OF A VACCINATION MODEL FOR INFECTIOUS DISEASES WITH ASYMPTOMATIC CARRIERS Martin Luther Mann Manyombe1;2 and Joseph Mbang1;2 Department of Mathematics, Faculty of Science University of Yaounde 1, P.O. Box 812 Yaounde, Cameroon 1;2;3; Jean Lubuma and Berge Tsanou ∗ Department of Mathematics and Applied Mathematics University of Pretoria, Pretoria 0002, South Africa (Communicated by Abba Gumel) Abstract. In this paper, an epidemic model is investigated for infectious dis- eases that can be transmitted through both the infectious individuals and the asymptomatic carriers (i.e., infected individuals who are contagious but do not show any disease symptoms). We propose a dose-structured vaccination model with multiple transmission pathways. Based on the range of the explic- itly computed basic reproduction number, we prove the global stability of the disease-free when this threshold number is less or equal to the unity. Moreover, whenever it is greater than one, the existence of the unique endemic equilibrium is shown and its global stability is established for the case where the changes of displaying the disease symptoms are independent of the vulnerable classes. Further, the model is shown to exhibit a transcritical bifurcation with the unit basic reproduction number being the bifurcation parameter. The impacts of the asymptomatic carriers and the effectiveness of vaccination on the disease transmission are discussed through through the local and the global sensitivity analyses of the basic reproduction number. Finally, a case study of hepatitis B virus disease (HBV) is considered, with the numerical simulations presented to support the analytical results. -

Yellow Fever 2016
Resident / Humanitarian Coordinator Report on the use of CERF funds RESIDENT / HUMANITARIAN COORDINATOR REPORT ON THE USE OF CERF FUNDS ANGOLA RAPID RESPONSE YELLOW FEVER 2016 RESIDENT/HUMANITARIAN COORDINATOR Pier Paolo Balladelli REPORTING PROCESS AND CONSULTATION SUMMARY a. Please indicate when the After Action Review (AAR) was conducted and who participated. Review agreed on 02/09/2016 and 07/09/2016. b. Please confirm that the Resident Coordinator and/or Humanitarian Coordinator (RC/HC) Report was discussed in the Humanitarian and/or UN Country Team and by cluster/sector coordinators as outlined in the guidelines. YES NO c. Was the final version of the RC/HC Report shared for review with in-country stakeholders as recommended in the guidelines (i.e. the CERF recipient agencies and their implementing partners, cluster/sector coordinators and members and relevant government counterparts)? YES NO Final version shared with UNICEF and UNDP, although this initiative was mainly implemented by WHO 2 I. HUMANITARIAN CONTEXT TABLE 1: EMERGENCY ALLOCATION OVERVIEW (US$) Total amount required for the humanitarian response: Source Amount CERF 3,000,000 Breakdown of total response COUNTRY-BASED POOL FUND (if applicable) 4,508,559 funding received by source OTHER (bilateral/multilateral) TOTAL 10,473,618 *The total amount does not match because this was considered an underfunded emergency. TABLE 2: CERF EMERGENCY FUNDING BY ALLOCATION AND PROJECT (US$) Allocation 1 – date of official submission: 06/04/2016- 05/10/2016 Agency Project code Cluster/Sector -
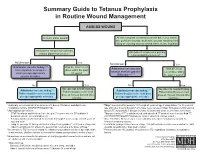
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -

YF-VAX® Rx Only AHFS Category
YF-VAX® Rx Only Laboratory Personnel AHFS Category: 80:12 Laboratory personnel who handle virulent yellow fever virus or concentrated preparations Rx only of the yellow fever vaccine virus strains may be at risk of exposure by direct or indirect Yellow Fever Vaccine contact or by aerosols. (14) DESCRIPTION CONTRAINDICATIONS ® Hypersensitivity YF-VAX , Yellow Fever Vaccine, for subcutaneous use, is prepared by culturing the YF-VAX is contraindicated in anyone with a history of acute hypersensitivity reaction to any 17D-204 strain of yellow fever virus in living avian leukosis virus-free (ALV-free) chicken component of the vaccine. (See DESCRIPTION section.) Because the yellow fever virus embryos. The vaccine contains sorbitol and gelatin as a stabilizer, is lyophilized, and is used in the production of this vaccine is propagated in chicken embryos, do not administer hermetically sealed under nitrogen. No preservative is added. Each vial of vaccine is YF-VAX to anyone with a history of acute hypersensitivity to eggs or egg products due to supplied with a separate vial of sterile diluent, which contains Sodium Chloride Injection a risk of anaphylaxis. Less severe or localized manifestations of allergy to eggs or to USP – without a preservative. YF-VAX is formulated to contain not less than 4.74 log10 feathers are not contraindications to vaccine administration and do not usually warrant plaque forming units (PFU) per 0.5 mL dose throughout the life of the product. Before vaccine skin testing. (See PRECAUTIONS section, Testing for Hypersensitivity Re- reconstitution, YF-VAX is a pinkish color. After reconstitution, YF-VAX is a slight pink-brown actions subsection.) Generally, persons who are able to eat eggs or egg products may suspension. -

Hanna Nohynek @Hnohynek
Biosketch Hanna Nohynek @hnohynek Hanna Nohynek is Chief Physician and Deputy Head of the Infectious Diseases Control and Vaccines Unit of the Department of Health Security at the Finnish Institute for Health and Welfare. She serves as secretary of the Finnish NITAG (KRAR), and leads the subgroup on Strategic development of the influenza vaccination programme and the subgroup on the SARS-CoV-2 vaccination strategy. She practices clinical medicine at a travel health clinic in Aava, Helsinki. She was instrumental in designing the first THL (KTL) health advisory for refugees and asylum seekers in Finland, studying the narcolepsy signal post pandemic vaccination, designing the introduction of the HPV vaccine to the national immunization programme, and the introduction of the live attenuated influenza vaccine for children. Her present research interests are register-based vaccine impact studies, evidence based policy/decision making, vaccine safety, hesitancy, SARS-CoV-2, RSV, influenza and pneumococcus. She coordinates the work packages on field studies and communication for IMI DRIVE on brand specific influenza vaccine effectiveness (www.drive-eu.org). She has authored more than 130 original articles (including the first scientific report on the association between pandemic influenza vaccination and narcolepsy), and she teaches, giving over 30 invited lectures annually and guiding elective, graduate and PhD students (presently Raija Auvinen and Idil Hussein). She belongs to the external faculty of the University of Tampere MSc course on Global Health. She has served on expert committees evaluating HBV, PCV and rota virus vaccines in Finland, and as an advisor to the EU, IMI, IVI, WHO, GAVI, SIDA/SRC, and the Finnish MOFA. -

Vaccines for Preteens
| DISEASES and the VACCINES THAT PREVENT THEM | INFORMATION FOR PARENTS Vaccines for Preteens: What Parents Should Know Last updated JANUARY 2017 Why does my child need vaccines now? to get vaccinated. The best time to get the flu vaccine is as soon as it’s available in your community, ideally by October. Vaccines aren’t just for babies. Some of the vaccines that While it’s best to be vaccinated before flu begins causing babies get can wear off as kids get older. And as kids grow up illness in your community, flu vaccination can be beneficial as they may come in contact with different diseases than when long as flu viruses are circulating, even in January or later. they were babies. There are vaccines that can help protect your preteen or teen from these other illnesses. When should my child be vaccinated? What vaccines does my child need? A good time to get these vaccines is during a yearly health Tdap Vaccine checkup. Your preteen or teen can also get these vaccines at This vaccine helps protect against three serious diseases: a physical exam required for sports, school, or camp. It’s a tetanus, diphtheria, and pertussis (whooping cough). good idea to ask the doctor or nurse every year if there are any Preteens should get Tdap at age 11 or 12. If your teen didn’t vaccines that your child may need. get a Tdap shot as a preteen, ask their doctor or nurse about getting the shot now. What else should I know about these vaccines? These vaccines have all been studied very carefully and are Meningococcal Vaccine safe. -
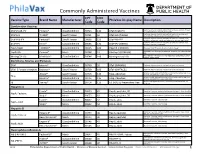
Commonly Administered Vaccines
Commonly Administered Vaccines CPT CVX Vaccine Type Brand Name Manufacturer PhilaVax Display Name Description Code Code Combination Vaccines Diptheria, tetanus toxoids and acellular pertussis vaccine, Hepati- DTaP-HepB-IPV Pediarix® GlaxoSmithKline 90723 110 DTaP-HepB-IPV tis B and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine and DTaP-Hib TriHIBit® Sanofi Pasteur 90721 50 DTaP-Hib (TriHIBit) Haemophilus influenzae type b conjugate vaccine Diptheria, tetanus toxoids and acellular pertussis vaccine, Hae- DTaP-Hib-IPV Pentacel® Sanofi Pasteur 90698 120 DTaP-Hib-IPV mophilus influenzae type b, and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine, and DTaP-IPV Kinrix® GlaxoSmithKline 90696 130 DTaP-IPV (KINRIX) poliovirus vaccine, inactivated HepA-HepB TWINRIX® GlaxoSmithKline 90636 104 HepA/B (TWINRIX) Hepatisis A and Hepatitis B vaccine, adult dosage Hepatitis B and Hemophilus influenza b vaccine, for intramuscular HepB-Hib Comvax® Merck 90748 51 Hib-Hep B (COMVAX) use Haemophilus influenza b and meningococcal sero groups C and Y MeningC/Y-Hib Menhibrix® GlaxoSmithKline 90644 148 Meningococcal-Hib vaccine, 4 dose series Diphtheria, Tetanus and Pertussis DTaP Infanrix® GlaxoSmithKline 90700 20 DTaP (INFANRIX) Diptheria, tetanus toxoids and acellular pertussis vaccine DTaP, 5 Pertussis Antigens Daptacel® Sanofi Pasteur 90700 106 DTaP (DAPTACEL) Diptheria, tetanus toxoids and acellular pertussis vaccine Tetanus toxoid, reduced diphtheria toxoid, and acellular -

UNEP Mercury Treaty Protects Access to Thiomersal-Containing Vaccines
UNEP mercury treaty protects access to thiomersal-containing vaccines United Nations Environment Program has developed a treaty on mercury in an effort to protect human health and the environment by limiting mercury releases. In the course of the negotiations, a proposal was made to restrict vaccines that contain the preservative thiomersal under a section of the treaty that prohibits trade of mercury-added products. The implications of restricting thiomersal, an ethyl mercury-containing preservative, would be significant. According to SAGE, “Thiomersal-containing vaccines [are] safe, essential, and irreplaceable components of immunization programs, especially in developing countries, and…removal of these products would disproportionately jeopardize the health and lives of the most disadvantaged children worldwide.” The treaty annex that describes prohibited products specifically excludes “vaccines containing thiomersal as preservatives” under a short list of products the authors intended to emphasize were to be protected. Protecting access to vaccines came as the result of a strong partnership between WHO, UNICEF, GAVI, and civil society advocates and experts around the world to educate country delegates, who predominantly came from ministries of environment. This was also a wonderful partnership with animal health experts, who similarly rely on thiomersal for veterinary vaccines. By facilitating communication between ministries of health and ministries of environment, strong statements are made by delegates about the essential role of thiomersal-containing vaccines in protecting human health. PATH will be collecting and disseminating additional information about how the community came together around this issue and lessons learned in the coming months. .