Gavi's Vaccine Investment Strategy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Yellow Fever 2016
Resident / Humanitarian Coordinator Report on the use of CERF funds RESIDENT / HUMANITARIAN COORDINATOR REPORT ON THE USE OF CERF FUNDS ANGOLA RAPID RESPONSE YELLOW FEVER 2016 RESIDENT/HUMANITARIAN COORDINATOR Pier Paolo Balladelli REPORTING PROCESS AND CONSULTATION SUMMARY a. Please indicate when the After Action Review (AAR) was conducted and who participated. Review agreed on 02/09/2016 and 07/09/2016. b. Please confirm that the Resident Coordinator and/or Humanitarian Coordinator (RC/HC) Report was discussed in the Humanitarian and/or UN Country Team and by cluster/sector coordinators as outlined in the guidelines. YES NO c. Was the final version of the RC/HC Report shared for review with in-country stakeholders as recommended in the guidelines (i.e. the CERF recipient agencies and their implementing partners, cluster/sector coordinators and members and relevant government counterparts)? YES NO Final version shared with UNICEF and UNDP, although this initiative was mainly implemented by WHO 2 I. HUMANITARIAN CONTEXT TABLE 1: EMERGENCY ALLOCATION OVERVIEW (US$) Total amount required for the humanitarian response: Source Amount CERF 3,000,000 Breakdown of total response COUNTRY-BASED POOL FUND (if applicable) 4,508,559 funding received by source OTHER (bilateral/multilateral) TOTAL 10,473,618 *The total amount does not match because this was considered an underfunded emergency. TABLE 2: CERF EMERGENCY FUNDING BY ALLOCATION AND PROJECT (US$) Allocation 1 – date of official submission: 06/04/2016- 05/10/2016 Agency Project code Cluster/Sector -

Package Insert
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------------- CONTRAINDICATIONS ------------------------------------- These highlights do not include all the information needed to use ® • History of severe allergic reactions (e.g., anaphylaxis) to egg proteins, or any FLUVIRIN (Influenza Virus Vaccine) safely and effectively. See full ® ® component of FLUVIRIN , or life-threatening reactions to previous influenza prescribing information for FLUVIRIN . vaccinations. (4.1, 11) FLUVIRIN® (Influenza Virus Vaccine) Suspension for Intramuscular Injection ---------------------- WARNINGS AND PRECAUTIONS ------------------------------ 2017-2018 Formula • If Guillain-Barré syndrome has occurred within 6 weeks of receipt of prior Initial US Approval: 1988 influenza vaccine, the decision to give FLUVIRIN® should be based on -------------------------- INDICATIONS AND USAGE ---------------------------------- careful consideration of the potential benefits and risks. (5.1) ® • FLUVIRIN is an inactivated influenza virus vaccine indicated for active • Immunocompromised persons may have a reduced immune response to immunization of persons 4 years of age and older against influenza disease FLUVIRIN®. (5.2) caused by influenza virus subtypes A and type B contained in the vaccine (1). • The tip caps of the FLUVIRIN® prefilled syringes may contain natural rubber • FLUVIRIN® is not indicated for children less than 4 years of age because latex which may cause allergic reactions in latex sensitive individuals. there is evidence of diminished immune response -

Hanna Nohynek @Hnohynek
Biosketch Hanna Nohynek @hnohynek Hanna Nohynek is Chief Physician and Deputy Head of the Infectious Diseases Control and Vaccines Unit of the Department of Health Security at the Finnish Institute for Health and Welfare. She serves as secretary of the Finnish NITAG (KRAR), and leads the subgroup on Strategic development of the influenza vaccination programme and the subgroup on the SARS-CoV-2 vaccination strategy. She practices clinical medicine at a travel health clinic in Aava, Helsinki. She was instrumental in designing the first THL (KTL) health advisory for refugees and asylum seekers in Finland, studying the narcolepsy signal post pandemic vaccination, designing the introduction of the HPV vaccine to the national immunization programme, and the introduction of the live attenuated influenza vaccine for children. Her present research interests are register-based vaccine impact studies, evidence based policy/decision making, vaccine safety, hesitancy, SARS-CoV-2, RSV, influenza and pneumococcus. She coordinates the work packages on field studies and communication for IMI DRIVE on brand specific influenza vaccine effectiveness (www.drive-eu.org). She has authored more than 130 original articles (including the first scientific report on the association between pandemic influenza vaccination and narcolepsy), and she teaches, giving over 30 invited lectures annually and guiding elective, graduate and PhD students (presently Raija Auvinen and Idil Hussein). She belongs to the external faculty of the University of Tampere MSc course on Global Health. She has served on expert committees evaluating HBV, PCV and rota virus vaccines in Finland, and as an advisor to the EU, IMI, IVI, WHO, GAVI, SIDA/SRC, and the Finnish MOFA. -

UNEP Mercury Treaty Protects Access to Thiomersal-Containing Vaccines
UNEP mercury treaty protects access to thiomersal-containing vaccines United Nations Environment Program has developed a treaty on mercury in an effort to protect human health and the environment by limiting mercury releases. In the course of the negotiations, a proposal was made to restrict vaccines that contain the preservative thiomersal under a section of the treaty that prohibits trade of mercury-added products. The implications of restricting thiomersal, an ethyl mercury-containing preservative, would be significant. According to SAGE, “Thiomersal-containing vaccines [are] safe, essential, and irreplaceable components of immunization programs, especially in developing countries, and…removal of these products would disproportionately jeopardize the health and lives of the most disadvantaged children worldwide.” The treaty annex that describes prohibited products specifically excludes “vaccines containing thiomersal as preservatives” under a short list of products the authors intended to emphasize were to be protected. Protecting access to vaccines came as the result of a strong partnership between WHO, UNICEF, GAVI, and civil society advocates and experts around the world to educate country delegates, who predominantly came from ministries of environment. This was also a wonderful partnership with animal health experts, who similarly rely on thiomersal for veterinary vaccines. By facilitating communication between ministries of health and ministries of environment, strong statements are made by delegates about the essential role of thiomersal-containing vaccines in protecting human health. PATH will be collecting and disseminating additional information about how the community came together around this issue and lessons learned in the coming months. . -
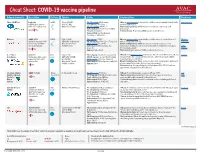
Cheat Sheet: COVID-19 Vaccine Pipeline
Cheat Sheet: COVID-19 vaccine pipeline Primary sponsor(s) Description Platform Funders Status Considerations Read more Pfizer / BioNTech Comirnaty mRNA Pfizer ($500M) Ph. I/II ongoing: 456/Germany Efficacy: Interim analysis shows that the candidate was safe and well-tolerated with New York Times mRNA that encodes for USG ($1.9M) Ph. II planned: 960/China an efficacy rate of 95%. SARS-CoV-2 spike protein. Warp Speed Finalist Ph. II/III ongoing: 44K US +5 Manufacturing/delivery: mRNA vaccines are relatively easy to scale and Authorization: EUA in EU, US, +9; WHO manufacture. Emergency Validation Platform history: No previous mRNA vaccines licensed for use. Approval: Bahrain, New Zealand, Saudi Arabia, Switzerland Moderna mRNA-1273 mRNA USG ($2.48B) Ph. I ongoing: 155/US Efficacy: Interim analysis shows that the candidate was safe and well-tolerated Moderna Synthetic messenger RNA CEPI/GAVI (Undisclosed) Ph. II/III ongoing: 3000 (12 to 17 years)/ US with an efficacy rate of 94.5%. Statement that encodes for SARS- Warp Speed Finalist Ph. III ongoing: 30,000/US Manufacturing/delivery: mRNA vaccines are relatively easy to scale and CoV-2 spike protein. COVAX Portfolio Authorization: EUA in Canada, EU, manufacture (potential for 1B doses by 2022); likely to require two doses, but a AVAC Israel, US third may be necessary. Webinar Approval: Switzerland Platform history: No previous mRNA vaccines licensed for use. U. of Oxford AZD1222 Viral USG ($1.2B) Ph. II ongoing: 300 vols (6-17 years)/ UK Efficacy: Ph. III interim analysis shows vaccine was safe and well-tolerated, efficacy Science AstraZeneca Chimpanzee Adeno vector vector CEPI/GAVI ($750M) Ph. -

Global Challenges in Seasonal Influenza Vaccine Supply, Use, and Policy
Intersect, Vol 12, No. 1 (2018) Global Challenges in Seasonal Influenza Vaccine Supply, Use, and Policy Kaitlin Schroeder Stanford University Abstract Seasonal influenza outbreaks occur on every continent, infecting millions and killing around 500,000 patients each year. The 2018 influenza season has been a vicious one—the H3N2 strain is a fast-mutating, aggressive form of the virus, and we have had difficulty immunizing against it. Decreasing the devastation of seasonal influenza starts with smart vaccine systems: a greater supply of doses distributed to the right people. In this review, we evaluate the global threat of seasonal influenza and explore the availability of vaccines as an essential prevention mechanism. We first identify key stakeholders in global influenza policy, vaccine supply, and regional public health governance. Next, we define the extent of the need for vaccines by examining surveillance systems and assessing the current disease burden of seasonal influenza. We examine current challenges in vaccine availability and allocation, and their respective impacts on health outcomes. Finally, we discuss policy implications of supply and allocation studies; we particularly note the promising outlook of communication programs, the advantages of optimized dose distribution, and the need to concentrate on infrastructure in low-income countries. Schroeder, Global Influenza Vaccine Challenges Introduction “Vaccines are miracles.” Professor Pedro Alonso of the Institute of Global Health, Barcelona explains that just a few dollars spent on immunization can protect an individual from severe disease and disability, making vaccines “one of the best investments in health” (Robert, n.d.). Among the recognized vaccine-preventable diseases (VPDs) is seasonal influenza, an acute viral infection that affects millions of people worldwide every year. -

Yellow Fever Vaccine
Yellow Fever Vaccine: Current Supply Outlook UNICEF Supply Division May 2016 0 Yellow Fever Vaccine - Current Supply Outlook May 2016 This update provides revised information on yellow fever vaccine supply availability and increased demand. Despite slight improvements in availability and the return of two manufacturers from temporary suspension, a constrained yellow fever vaccine market will persist through 2017, exacerbated by current emergency outbreak response requirements. 1. Summary Yellow fever vaccine (YFV) supply through UNICEF remains constrained due to limited production capacity. Despite the return of two manufacturers from temporary suspension, the high demand currently generated from the yellow fever (YF) outbreak in Angola, in addition to potential increased outbreak response requirements in other geographic regions, outweigh supply. The demand in response to the current YF outbreak in Angola could negatively impact the supply availability for some routine immunization programme activities. UNICEF anticipates a constrained global production capacity to persist through 2017. UNICEF has long-term arrangements (LTAs) with four YFV suppliers to cover emergency stockpile, routine immunization, and preventative campaign requirements. During 2015, UNICEF increased total aggregate awards to suppliers to reach approximately 98 million doses for 2016- 2017. However, whereas supply can meet emergency stockpile and routine requirements, it is insufficient to meet all preventive campaign demands, which increased the total demand through UNICEF to 109 million doses. The weighted average price (WAP) per dose for YFV increased 7% a year on average since 2001, from US$ 0.39 to reach US$ 1.04 in 2015. Given the continued supply constraints, UNICEF anticipates a YFV WAP per dose of US$1.10 in the near-term. -

An Overview of COVID Vaccine Clinical Trial Results & Some Challenges
An overview of COVID vaccine clinical trial results & some challenges DCVMN Webinar December 8th, 2020 Access to COVID-19 tools ACCESSACCESS TO TOCOVID-19 COVID-19 TOOLS TOOLS (ACT) (ACT) ACCELERATOR ACCELERATOR (ACT) accelerator A GlobalA GlobalCollaboration Collaboration to Accelerate tothe AccelerateDevelopment, the Production Development, and Equitable Production Access to New and Equitable AccessCOVID-19 to New diagnostics, COVID-19 therapeutics diagnostics, and vaccines therapeutics and vaccines VACCINES DIAGNOSTICS THERAPEUTICS (COVAX) Development & Manufacturing Led by CEPI, with industry Procurement and delivery at scale Led by Gavi Policy and allocation Led by WHO Key players SOURCE: (ACT) ACCELERATOR Commitment and Call to Action 24th April 2020 ACT-A / COVAX governance COVAX COORDINATION MEETING CEPI Board Co-Chair: Jane Halton Co-Chair: Dr. Ngozi Gavi Board Workstream leads + DCVMN and IFPMA-selected Reps As needed – R&D&M Chair; COVAX IPG Chair Development & Manufacturing Procurement and delivery Policy and allocation (COVAX) at scale Led by (with industry) Led by Led by R&D&M Investment Committee COVAX Independent Product Group Technical Review Group Portfolio Group Vaccine Teams SWAT teams RAG 3 COVAX SWAT teams are being set up as a joint platform to accelerate COVID- 19 Vaccine development and manufacturing by addressing common challenges together Timely and targeted Multilateral Knowledge-based Resource-efficient Addresses specific cross- Establishes a dialogue Identifies and collates Coordinates between developer technical and global joint effort most relevant materials different organizations/ challenges as they are across different COVID-19 and insights across the initiatives to limit raised and/or identified vaccines organizations broader COVID-19 duplications and ensure on an ongoing basis (incl. -

Recommended Adult Immunization Schedule
Recommended Adult Immunization Schedule UNITED STATES for ages 19 years or older 2021 Recommended by the Advisory Committee on Immunization Practices How to use the adult immunization schedule (www.cdc.gov/vaccines/acip) and approved by the Centers for Disease Determine recommended Assess need for additional Review vaccine types, Control and Prevention (www.cdc.gov), American College of Physicians 1 vaccinations by age 2 recommended vaccinations 3 frequencies, and intervals (www.acponline.org), American Academy of Family Physicians (www.aafp. (Table 1) by medical condition and and considerations for org), American College of Obstetricians and Gynecologists (www.acog.org), other indications (Table 2) special situations (Notes) American College of Nurse-Midwives (www.midwife.org), and American Academy of Physician Assistants (www.aapa.org). Vaccines in the Adult Immunization Schedule* Report y Vaccines Abbreviations Trade names Suspected cases of reportable vaccine-preventable diseases or outbreaks to the local or state health department Haemophilus influenzae type b vaccine Hib ActHIB® y Clinically significant postvaccination reactions to the Vaccine Adverse Event Hiberix® Reporting System at www.vaers.hhs.gov or 800-822-7967 PedvaxHIB® Hepatitis A vaccine HepA Havrix® Injury claims Vaqta® All vaccines included in the adult immunization schedule except pneumococcal 23-valent polysaccharide (PPSV23) and zoster (RZV) vaccines are covered by the Hepatitis A and hepatitis B vaccine HepA-HepB Twinrix® Vaccine Injury Compensation Program. Information on how to file a vaccine injury Hepatitis B vaccine HepB Engerix-B® claim is available at www.hrsa.gov/vaccinecompensation. Recombivax HB® Heplisav-B® Questions or comments Contact www.cdc.gov/cdc-info or 800-CDC-INFO (800-232-4636), in English or Human papillomavirus vaccine HPV Gardasil 9® Spanish, 8 a.m.–8 p.m. -

Human Papillomavirus Vaccine
Human Papillomavirus Vaccine: Supply and Demand Update UNICEF Supply Division October 2020 0 Human Papillomavirus Vaccine Supply and Demand Update - October 2020 This update provides information on human papillomavirus vaccine, including supply, demand, and pricing trends. It highlights continued supply constraints foreseen over 2020 and 2021, which also affects countries procuring through UNICEF. UNICEF requests self-financing middle-income countries to consolidate credible multi-year demand and to submit multi-year commitments through UNICEF. 1. Summary • UNICEF’s strategic plan for 2018-2021 seeks to ensure that at least 24 countries nationally introduce human papillomavirus (HPV) vaccine into their immunization programmes.1 As of to date, 20 countries supplied through UNICEF, of which 15 supported by Gavi, the Vaccine Alliance (Gavi) and five countries having transitioned from Gavi support and self-finance their procurement, have introduced HPV vaccines since 2013. Fourteen middle-income countries (MICs) are also procuring HPV vaccines through UNICEF. From 2013 to 2019, UNICEF’s total HPV vaccine procurement reached 30.9 million doses in support of girls. There is currently no gender-neutral programmes in countries supplied through UNICEF. Of the 30.9 million doses, UNICEF procured 28.3 million doses (91 per cent) for countries supported by Gavi, including those that transitioned from Gavi support and still access Gavi prices, and 2.6 million doses (9 per cent) on behalf of self-financing MICs. • In December 2016, Gavi revised its programme strategy to support full-scale national HPV vaccine introductions with multi-age cohort (MAC) vaccinations. This substantially increased HPV vaccine demand through UNICEF from 2017. -

'Astrazeneca' Covid-19 Vaccine
Medicines Law & Policy How the ‘Oxford’ Covid-19 vaccine became the ‘AstraZeneca’ Covid-19 vaccine By Christopher Garrison 1. Introduction. The ‘Oxford / AstraZeneca’ vaccine is one of the world’s leading hopes in the race to end the Covid-19 pandemic. Its history is not as clear, though, as it may first seem. The media reporting about the vaccine tends to focus either on the very small (non-profit, academic) Jenner Institute at Oxford University, where the vaccine was first invented, or the very large (‘Big Pharma’ firm) AstraZeneca, which is now responsible for organising its (non-profit) world-wide development, manufacture and distribution. However, examining the intellectual property (IP) path of the vaccine from invention to manufacture and distribution reveals a more complex picture that involves other important actors (with for-profit perspectives). Mindful of the very large sums of public money being used to support Covid-19 vaccine development, section 2 of this note will therefore contextualise the respective roles of the Jenner Institute, AstraZeneca and these other actors, so that their share of risk and (potential) reward in the project can be better understood. Section 3 provides comments as well as raising some important questions about what might yet be done better and what lessons can be learned for the future. 2. History of the ‘Oxford / AstraZeneca’ vaccine. 2.1 Oxford University and Oxford University Innovation Ltd. The Bayh-Dole Act (1980) was hugely influential in the United States and elsewhere in encouraging universities to commercially exploit the IP they were generating by setting up ‘technology transfer’ offices. -

UNICEF Deep-Dive 2020, Vaccine Industry Consultation UNICEF’S Tentative Vaccine Tender Calendar for the Upcoming Period INFLUENZA Deep-Dive Agenda
UNICEF Deep-dive 2020, Vaccine Industry Consultation UNICEF’s Tentative Vaccine Tender Calendar for the upcoming period INFLUENZA Deep-dive Agenda • Background and challenges • Feedback from the industry • Gavi learning agenda for seasonal influenza • Tender timelines • Key takeaways 4 Background & Challenges • Immunization programmes, vaccines, and auxiliary supplies for seasonal influenza are primarily funded through a country’s own health budget. • Due to limited funding, seasonal influenza programmes are often not implemented in LICs and MICs. • Historically, UNICEF has procured limited quantities of influenza vaccine on behalf of countries. • UNICEF often receives requests for supply of seasonal influenza vaccine late and after suppliers have determined the production volume for the global market. • Due to COVID-19, the demand for seasonal influenza vaccines through UNICEF has increased during 2020, and realized late which let to constrained availability for countries procuring through UNICEF. UNICEF plans to tender earlier to counter this risk. Feedback from the industry What should UNICEF do differently to incentivize your participation in the future tenders for seasonal influenza vaccines? Feedback from the industry Measures taken by UNICEF • Tender one year in advance to block the • Advance tender timelines doses for UNICEF. • Stakeholders reminded of: • Multi-year tender and LTA o the short window for production planning and supply • UNICEF take risks and commit to pay for o importance of timely and accurate the doses even they are not materialised forecasting into orders. • Published a Supply Note on Seasonal Influenza Vaccines in English & French. • Working with countries to improve longer- term forecast accuracy. 6 Gavi learning agenda for seasonal influenza • Background: only 8% of Gavi eligible • Duration of the project: 2021 – 2022 countries have seasonal influenza immunization programmes, and most • Targeted countries: Cote d’Ivoire, Kenya & countries in the African region do not have Uganda national influenza immunization policies.