Breast Cancer—Local / Regional / Adjuvant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nobel Prize in Medicine 1952 Was Awarded to Selman A
History of Мedicine of the Newest period (XX-XXI centuries). EHRLICH AND ARSPHENAMINE Paul Ehrlich In 1910, with his colleague Sahachiro Hata, conducted tests on arsphenamine, once sold under the commercial name Salvarsan. Salvarsan, a synthetic preparation containing arsenic, is lethal to the microorganism responsible for syphilis. SULFONAMIDE DRUGS In 1932 the German bacteriologist Gerhard Domagk announced that the red dye Prontosil is active against streptococcal infections in mice and humans. Soon afterward French workers showed that its active antibacterial agent is sulfanilamide. In 1928 ALEXANDER FLEMING noticed the PENICILLIN inhibitory activity of a stray mold on a plate culture of staphylococcus bacteria. In 1938 HOWARD FLORY, ERNEST CHAIN received pure penicillin. In 1945 ALEXANDER FLEMING, HOWARD FLORY, ERNEST CHAIN won the Noble Prize for the discovery of penicillin and its curative effect in various infectious diseases. ANTITUBERCULOSIS DRUGS •In 1944, SELMAN WAXMAN announced the discovery of STREPTOMYCIN from cultures of a soil organism Streptomyces griseus, and stated that it was active against M. tuberculosis. •Clinincal trials confirmed this claim. •The Nobel Prize in Medicine 1952 was awarded to Selman A. Waksman •In Paris, Élie Metchnikoff had already detected the role of white blood cells in the IMMUNOLOGY immune reaction, •Jules Bordet had identified antibodies in the blood serum. •The mechanisms of antibody activity were used to devise diagnostic tests for a number of diseases. •In 1906 August von Wassermann gave his name to the blood test for syphilis, and in 1908 the tuberculin test— the skin test for tuberculosis— came into use. INSULIN •In 1921, Frederick Banting and Charles H. -

SCIENTIFIC REPORT 2020 for the Years 2016 to 2019 Table of Contents
SCIENTIFIC REPORT 2020 For the years 2016 to 2019 Table of Contents 3 Foreword 4 Research in Numbers 7 Strategic Vision 9 Research Pillars 10 Pillar I: Dissecting Tumour Survival Mechanisms and Tumour Microenvironment 18 Pillar II: Tracking and Targeting Minimal Residual Disease 22 Pillar III: Next Generation Molecular Imaging to Better Personalise Treatment 27 Pillar IV: Accelerating Anticancer Drug Development 33 Pillar V: Developing New Approaches to Patient Empowerment and Well-being 40 New facilities will bring new opportunities for research 41 Organisation of Research Governance Research Support Units 48 Collaborations 51 Funding Les Amis de l’Institut Bordet Research Grants 54 Visiting Medical Research Fellows (2016-2019) 55 Awards 56 Publications 2016-2019 2016-2019 (Selected Papers) Publications 2019 79 Abbreviations 2 Foreword Dominique de Valeriola General Medical Director Institut Jules Bordet is a public and academic OECI*-certified comprehensive cancer center playing an important role in cancer care, research and education, both in Belgium and internationally. Entirely dedicated to adult cancer patients since its creation in 1939, it belongs to the City of Brussels and the Université Libre de Bruxelles. Both translational and clinical research are part of the Institute’s DNA, aiming to bring research discoveries to the patient’s bedside quickly. The present 2016-2019 scientific report reflects the spirit of commitment and collaboration of the Institute’s healthcare professionals, researchers, and administrative support teams and, above all, of the patients who trust our teams and volunteer to participate in clinical trials. A concerted and well-rewarded effort has been made during these recent years to build a stronger partnership with patients in developing our clinical trials, and to establish more efficient, centralised governance and operational support for our research activities. -

Balcomk41251.Pdf (558.9Kb)
Copyright by Karen Suzanne Balcom 2005 The Dissertation Committee for Karen Suzanne Balcom Certifies that this is the approved version of the following dissertation: Discovery and Information Use Patterns of Nobel Laureates in Physiology or Medicine Committee: E. Glynn Harmon, Supervisor Julie Hallmark Billie Grace Herring James D. Legler Brooke E. Sheldon Discovery and Information Use Patterns of Nobel Laureates in Physiology or Medicine by Karen Suzanne Balcom, B.A., M.L.S. Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin August, 2005 Dedication I dedicate this dissertation to my first teachers: my father, George Sheldon Balcom, who passed away before this task was begun, and to my mother, Marian Dyer Balcom, who passed away before it was completed. I also dedicate it to my dissertation committee members: Drs. Billie Grace Herring, Brooke Sheldon, Julie Hallmark and to my supervisor, Dr. Glynn Harmon. They were all teachers, mentors, and friends who lifted me up when I was down. Acknowledgements I would first like to thank my committee: Julie Hallmark, Billie Grace Herring, Jim Legler, M.D., Brooke E. Sheldon, and Glynn Harmon for their encouragement, patience and support during the nine years that this investigation was a work in progress. I could not have had a better committee. They are my enduring friends and I hope I prove worthy of the faith they have always showed in me. I am grateful to Dr. -
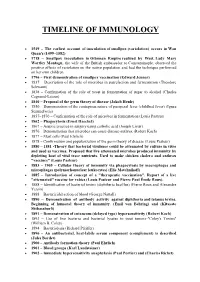
Timeline of Immunology
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins. -

Albert Claude, 1899-1983 with the Determined Intent to Fmd out Whatever There Was in It in Terms of Isolatable from Christian De Duve and George E
~·~-------------------------NME~W~S~AMNO~V~IE;vW~S:---------------------------- Obituary 'microsomes'. That was the beginning of a rather long side voyage that led him into the heart of the cell, not in search of a virus, but Albert Claude, 1899-1983 with the determined intent to fmd out whatever there was in it in terms of isolatable from Christian de Duve and George E. Palade particles, and to account for them in a careful quantitative manner. It was a ALBERT CLAUDE, who died in Brussels on Having failed in his first project, Claude glorious voyage during which he worked out Sunday 22 May, belonged to that small group went on to study the fate of the mouse sar his now classic cell-fractionation procedure. of truly exceptional individuals who, drawing coma S-37 when grafted in rats. The thesis Most of what we know today about the almost exclusively on their own resources and he wrote on his observations earned him a chemistry and activities of subcellular com following a vision far ahead of their time, government scholarship which he used to ponents is based on his quantitative ap opened single-handedly an entirely new field go to Berlin. There he frrst worked at the proach. Claude enjoyed isolating whatever of scientific investigation. Cancer Institute of the University, but was was isolatable: from microsomes to 'large He was born on 23 August 1899, in forced to leave prematurely after showing granules' (later recognized as mitochondria), Longlier, a hamlet of some 800 inhabitants that the bacterial theory of cancer genesis chromatin threads and zymogen granules. -

Federation Member Society Nobel Laureates
FEDERATION MEMBER SOCIETY NOBEL LAUREATES For achievements in Chemistry, Physiology/Medicine, and PHysics. Award Winners announced annually in October. Awards presented on December 10th, the anniversary of Nobel’s death. (-H represents Honorary member, -R represents Retired member) # YEAR AWARD NAME AND SOCIETY DOB DECEASED 1 1904 PM Ivan Petrovich Pavlov (APS-H) 09/14/1849 02/27/1936 for work on the physiology of digestion, through which knowledge on vital aspects of the subject has been transformed and enlarged. 2 1912 PM Alexis Carrel (APS/ASIP) 06/28/1873 01/05/1944 for work on vascular suture and the transplantation of blood vessels and organs 3 1919 PM Jules Bordet (AAI-H) 06/13/1870 04/06/1961 for discoveries relating to immunity 4 1920 PM August Krogh (APS-H) 11/15/1874 09/13/1949 (Schack August Steenberger Krogh) for discovery of the capillary motor regulating mechanism 5 1922 PM A. V. Hill (APS-H) 09/26/1886 06/03/1977 Sir Archibald Vivial Hill for discovery relating to the production of heat in the muscle 6 1922 PM Otto Meyerhof (ASBMB) 04/12/1884 10/07/1951 (Otto Fritz Meyerhof) for discovery of the fixed relationship between the consumption of oxygen and the metabolism of lactic acid in the muscle 7 1923 PM Frederick Grant Banting (ASPET) 11/14/1891 02/21/1941 for the discovery of insulin 8 1923 PM John J.R. Macleod (APS) 09/08/1876 03/16/1935 (John James Richard Macleod) for the discovery of insulin 9 1926 C Theodor Svedberg (ASBMB-H) 08/30/1884 02/26/1971 for work on disperse systems 10 1930 PM Karl Landsteiner (ASIP/AAI) 06/14/1868 06/26/1943 for discovery of human blood groups 11 1931 PM Otto Heinrich Warburg (ASBMB-H) 10/08/1883 08/03/1970 for discovery of the nature and mode of action of the respiratory enzyme 12 1932 PM Lord Edgar D. -

Jules Bordet (1870-1961): Pioneer of Immunology
Singapore Med J 2013; 54(9): 475-476 M edicine in S tamps doi:10.11622/smedj.2013166 Jules Bordet (1870-1961): Pioneer of immunology Jonathan Dworkin1, MD, Siang Yong Tan2, MD, JD t the time when Jules Bordet began his ground- THE TRANSFORMATION OF IMMUNOLOGY breaking experiments at the Pasteur Institute, the field Bordet began work at the Pasteur Institute in 1894, and of immunology was shrouded in pseudoscientific despite being part of Metchnikoff’s lab, he was more interested uncertainty. The lifting of this veil, through the in studying serum than white cells. The arrangement was Apersistent and patient process of experimentation, was Bordet’s an awkward one in which Bordet was compelled to put into great contribution to medicine in the 20th century. writing his research findings regarding the role of phagocytes, although in reality, his work had little to do with phagocytosis. BACKGROUND Jules Bordet was born in 1870 in Bordet possessed a reserved temperament and shunned the Soignies, a small town in Belgium. In 1874, his family moved to cult of personality that then existed around the brilliant but Brussels, and he attended a primary school in the Ecole unstable Metchnikoff. Given the contrast with his fiery Russian Moyenne, where his father taught. In secondary school, Bordet mentor, it was no surprise that Bordet evolved into a careful became interested in chemistry, and at the age of sixteen, he scientist, skeptical of broad principles derived from scant enrolled into medical school at the Free University of Brussels. data and content to draw conclusions on as narrow a basis as His early promise as a researcher earned him a scholarship the facts supported. -

Huangmei Opera in Anqing City,Anhui Province,China Meng
Huangmei Opera in Anqing City,Anhui Province,China Meng Liu A Thesis Submitted in Partial Fulfillment of Requirements for degree of Doctor of Philosophy in Music February 2021 Copyright of Mahasarakham University ฮวงเหมย่ โอเปร่า ในเมืองอนั ช่ิง จังหวัดอันฮุย ประเทศจีน วิทยานิพนธ์ ของ Meng Liu เสนอต่อมหาวทิ ยาลยั มหาสารคาม เพื่อเป็นส่วนหน่ึงของการศึกษาตามหลกั สูตร ปริญญาปรัชญาดุษฎีบัณฑิต สาขาวิชาดุริยางคศิลป์ กุมภาพันธ์ 2564 ลิขสิทธ์ิเป็นของมหาวทิ ยาลยั มหาสารคาม Huangmei Opera in Anqing City,Anhui Province,China Meng Liu A Thesis Submitted in Partial Fulfillment of Requirements for Doctor of Philosophy (Music) February 2021 Copyright of Mahasarakham University The examining committee has unanimously approved this Thesis, submitted by Ms. Meng Liu , as a partial fulfillment of the requirements for the Doctor of Philosophy Music at Mahasarakham University Examining Committee Chairman (Assoc. Prof. Wiboon Trakulhun , Ph.D.) Advisor (Prof. Arsenio Nicolas , Ph.D.) Committee (Asst. Prof. Sayam Chuangprakhon , Ph.D.) Committee (Asst. Prof. Khomkrit Karin , Ph.D.) Committee (Assoc. Prof. Phiphat Sornyai ) Mahasarakham University has granted approval to accept this Thesis as a partial fulfillment of the requirements for the Doctor of Philosophy Music (Asst. Prof. Khomkrit Karin , Ph.D.) (Assoc. Prof. Krit Chaimoon , Ph.D.) Dean of College of Music Dean of Graduate School D ABSTRACT TITLE Huangmei Opera in Anqing City,Anhui Province,China AUTHOR Meng Liu ADVISORS Professor Arsenio Nicolas , Ph.D. DEGREE Doctor of Philosophy MAJOR Music UNIVERSITY Mahasarakham University YEAR 2021 ABSTRACT This dissertation is a study of Huangmei opera in Anqing City, Anhui Province, China. It describes the characteristics of its music, its history, and its preservation, promotion and transmission in the context of contemporary times. Huangmei opera has a history of more than 200 years from the Qianlong period of the Qing Dynasty to the present. -
Nobel Laureates in Physiology Or Medicine
All Nobel Laureates in Physiology or Medicine 1901 Emil A. von Behring Germany ”for his work on serum therapy, especially its application against diphtheria, by which he has opened a new road in the domain of medical science and thereby placed in the hands of the physician a victorious weapon against illness and deaths” 1902 Sir Ronald Ross Great Britain ”for his work on malaria, by which he has shown how it enters the organism and thereby has laid the foundation for successful research on this disease and methods of combating it” 1903 Niels R. Finsen Denmark ”in recognition of his contribution to the treatment of diseases, especially lupus vulgaris, with concentrated light radiation, whereby he has opened a new avenue for medical science” 1904 Ivan P. Pavlov Russia ”in recognition of his work on the physiology of digestion, through which knowledge on vital aspects of the subject has been transformed and enlarged” 1905 Robert Koch Germany ”for his investigations and discoveries in relation to tuberculosis” 1906 Camillo Golgi Italy "in recognition of their work on the structure of the nervous system" Santiago Ramon y Cajal Spain 1907 Charles L. A. Laveran France "in recognition of his work on the role played by protozoa in causing diseases" 1908 Paul Ehrlich Germany "in recognition of their work on immunity" Elie Metchniko France 1909 Emil Theodor Kocher Switzerland "for his work on the physiology, pathology and surgery of the thyroid gland" 1910 Albrecht Kossel Germany "in recognition of the contributions to our knowledge of cell chemistry made through his work on proteins, including the nucleic substances" 1911 Allvar Gullstrand Sweden "for his work on the dioptrics of the eye" 1912 Alexis Carrel France "in recognition of his work on vascular suture and the transplantation of blood vessels and organs" 1913 Charles R. -

Elie Metchnikoff – Founder of Longevity Science – 2015
ISSN 20790570, Advances in Gerontology, 2015, Vol. 5, No. 4, pp. 201–208. © Pleiades Publishing, Ltd., 2015. Published in Russian in Uspekhi Gerontologii, 2015, Vol. 28, No. 2, pp. 207–217. Elie Metchnikoff—The Founder of Longevity Science and a Founder of Modern Medicine: In Honor of the 170th Anniversary1 Ilia Stambler Department of Science, Technology and Society, Bar Ilan University, Ramat Gan, Israel email: [email protected] Abstract—The years 2015–2016 mark a double anniversary—the 170th anniversary of birth and the 100th anni versary of death—of one of the greatest Russian scientists, a person that may be considered a founding figure of modern immunology, aging, and longevity science—Elie Metchnikoff (May 15, 1845–July 15, 1916). At this time of rapid aging of the world population and the rapid development of technologies that may amelio rate degenerative aging processes, Metchnikoff’s pioneering contribution to the search for antiaging and healthspanextending means should be recalled and honored. Keywords: Elie Metchnikoff, medical history, aging and longevity research DOI: 10.1134/S2079057015040219 ELIE1 METCHNIKOFF—THE FOUNDER OF GERONTOLOGY The world is rapidly aging, threatening grave con sequences for the global society and economy, while the rapid development of biomedical science and technology stand as the first line of defense against the potential threat. These two everincreasing forces bring gerontology, which describes the challenges of aging while at the same time seeking means to address those challenges, to the center stage of the global sci entific, technological, and political discourse. At this time, it may be fit to honor the persons who stood at the origin of gerontological discourse, not just as a sci entific field but as a social and intellectual movement. -

The Pluripotent History of Immunology a Review
AVANT Volume III, Number 1/2012 www.avant.edu.pl/en 37 The pluripotent history of immunology A review Neeraja Sankaran History of Science, Technology & Medicine Underwood International College, Yonsei University, Seoul, S. Korea Abstract The historiography of immunology since 1999 is reviewed, in part as a response to claims by historians such as Thomas Söderqvist the field was still immature at the time (Söderqvist & Stillwell 1999). First addressed are the difficulties, past and present, surrounding the disciplinary definition of immunology, which is followed by a commentary on the recent scholarship devoted to the concept of the immune self. The new literature on broad immunological topics is examined and assessed, and specific charges leveled against the paucity of certain types of histories, e.g. biographical and institutional histories, are evaluated. In conclusion, there are compelling indications that the history of immunology has moved past the initial tentative stages identified in the earlier reviews to become a bustling, pluripotent discipline, much like the subject of its scrutiny, and that it continues to develop in many new and exciting directions. Keywords: Biographical history; Continuity model; Danger Model; Historiography of Immunology; History of Immunology; Institutional history; Self vs. Non-self model. Introduction Two decades ago, in the summer of 1992, the Naples Zoological Station’s summer school in the history of the life sciences, a roughly biennial event since the mid- 1970s, chose to focus on the history of immunology. Whether the meeting achieved its stated purpose of facilitating dialogue and exchange between immunologists and historians appears to have been a matter of some contention among the atten- dees (Judson & Mackay 1992; Söderqvist 1993). -

Introduction
Notes Introduction 1. For general literature on the history of the receptor concept see the notes below and the first chapter of this book. 2. See Bowman (1999). 3. Drews (2002). 4. ‘World Health Organization Model List of Essential Medicines’, 15th edition (2007), http://www.who.int/medicines/publications/essentialmedicines/en/; NCPA report, Bartlett (2000), http://www.ncpa.org/oped/bartlett/sep0400. html; for US figures, see Hagist and Kotlikoff (2007), www.ncpa.org/pub/ st/st286. 5. Recent examples include Schüttler (2003) and Mould (1993). 6. See the example of the scientific genetics community in the United States and Germany (Harwood 1993). For a more recent example see Robert E. Kohler’s description and analysis of the community of geneticists working on the fruit-fly drosophila (‘fly group’) (Kohler 1994; 1999). 7. Stanton (2002, esp. pp. vii–x) and Löwy (1993a, pp. v–viii). See also Pickstone (1992). 8. Hagner (2001, esp. p. 23). 9. Daniel (2001). 10. Morrell (1993, esp. p. 124). 11. Morrell (1993; 1972). 12. Moraw (1988, p. 3). 13. For details see the list of archival sources at the end of the book. 14. Concerning oral history and its problems, see Benison (1971), Perks (1990), Thompson (1991; 2000), Thompson and Perks (1993), Ward (1995), Perks and Thompson (1997) and Singer (1997). 15. Ibid. 16. Stannard (1961) and Leake (1975, p. 59). 17. Harig (1974) and Debru (1997). 18. Galen, De simplicium medicamentorum temperamentis ac facultatibus 7.12 and 11.1. Thanks to Philip van der Eijk (Newcastle) for these references. 19. Stein (1997) and Watson (1966).