Incontinence Patient Guide Table of Contents Urology Care Foundation Bladder Health Committee
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urinary Incontinence: Impact on Long Term Care
Urinary Incontinence: Impact on Long Term Care Muhammad S. Choudhury, MD, FACS Professor and Chairman Department of Urology New York Medical College Director of Urology Westchester Medical Center 1 Urinary Incontinence: Overview • Definition • Scope • Anatomy and Physiology of Micturition • Types • Diagnosis • Management • Impact on Long Term Care 2 Urinary Incontinence: Definition • Involuntary leakage of urine which is personally and socially unacceptable to an individual. • It is a multifactorial syndrome caused by a combination of: • Genito urinary pathology. • Age related changes. • Comorbid conditions that impair normal micturition. • Loss of functional ability to toilet oneself. 3 Urinary Incontinence: Scope • Prevalence of Urinary incontinence increase with age. • Affects more women than men (2:1) up to age 80. • After age 80, both women and men are equally affected. • Urinary Incontinence affect 15% to 30% of the general population > 65 years. • > 50% of 1.5 million Long Term Care residents may be incontinent. • The cost to care for this group is >5 billion per year. • The total cost of care for Urinary Incontinence in the U.S. is estimated to be over $36 billion. Ehtman et al., 2012. 4 Urinary Incontinence: Impact on Quality of Life • Loss of self esteem. • Avoidance of social activity and interaction. • Decreased ability to maintain independent life style. • Increased dependence on care givers. • One of the most common reason for long term care placement. Grindley et al. Age Aging. 1998; 22: 82-89/Harris T. Aging in the eighties. NCHS # 121 1985. Noelker L. Gerontologist 1987; 27: 194-200. 5 Health related consequences of Urinary Incontinence • Increased propensity for fall/fracture. -

CMS Manual System Human Services (DHHS) Pub
Department of Health & CMS Manual System Human Services (DHHS) Pub. 100-07 State Operations Centers for Medicare & Provider Certification Medicaid Services (CMS) Transmittal 8 Date: JUNE 28, 2005 NOTE: Transmittal 7, of the State Operations Manual, Pub. 100-07 dated June 27, 2005, has been rescinded and replaced with Transmittal 8, dated June 28, 2005. The word “wound” was misspelled in the Interpretive Guidance section. All other material in this instruction remains the same. SUBJECT: Revision of Appendix PP – Section 483.25(d) – Urinary Incontinence, Tags F315 and F316 I. SUMMARY OF CHANGES: Current Guidance to Surveyors is entirely replaced by the attached revision. The two tags are being combined as one, which will become F315. Tag F316 will be deleted. The regulatory text for both tags will be combined, followed by this revised guidance. NEW/REVISED MATERIAL - EFFECTIVE DATE*: June 28, 2005 IMPLEMENTATION DATE: June 28, 2005 Disclaimer for manual changes only: The revision date and transmittal number apply to the red italicized material only. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual not updated.) (R = REVISED, N = NEW, D = DELETED) – (Only One Per Row.) R/N/D CHAPTER/SECTION/SUBSECTION/TITLE R Appendix PP/Tag F315/Guidance to Surveyors – Urinary Incontinence D Appendix PP/Tag F316/Urinary Incontinence III. FUNDING: Medicare contractors shall implement these instructions within their current operating budgets. IV. ATTACHMENTS: Business Requirements x Manual Instruction Confidential Requirements One-Time Notification Recurring Update Notification *Unless otherwise specified, the effective date is the date of service. -

Urinary Tract Infection (UTI): Western and Ayurvedic Diagnosis and Treatment Approaches
Urinary tract infection (UTI): Western and Ayurvedic Diagnosis and Treatment Approaches. By: Mahsa Ranjbarian Urinary system Renal or Urinary system is one of the 10 body systems that we have. This system is the body drainage system. The urinary system is composed of kidneys (vrikka), ureters (mutravaha nadis), bladder(mutrashaya) and urethra(mutramarga). The kidneys are a pair of bean-shaped, fist size organs that lie in the middle of the back, just below the rib cage, one on each side of the spine. Ureters are tubes that carry the wastes or urine from the kidneys to the bladder. The urine finally exit the body from the urethra when the bladder is full.1 Urethras length is shorter in women than men due to the anatomical differences. Major function of the urinary system is to remove wastes and water from our body through urination. Other important functions of the urinary system are as follows. 1. Prevent dehydration and at the same time prevent the buildup of extra fluid in the body 2. Cleans the blood of metabolic wastes 3. Removing toxins from the body 4. Maintaining the homeostasis of many factors including blood PH and blood pressure 5. Producing erythrocytes 6. make hormones that help regulate blood pressure 7. keep bones strong 8. keep levels of electrolytes, such as potassium and phosphate, stable 2 The Urinary system like any other systems of our body is working under the forces of three doshas, subdoshas. Mutravaha srotas, Ambuvahasrota and raktavahasrota are involved in formation and elimination of the urine. Urine gets separated from the rasa by maladhara kala with the help of pachaka pitta and samana vayu and then through the mutravaha srota(channels carrying the urine) it is taken to the bladder. -

Urinary Incontinence Embarrassing but Treatable 2015 Rev
This information provides a general overview on this topic and may not apply to Health Notes everyone. To find out if this information applies to you and to get more information on From Your Family Doctor this subject, talk to your family doctor. Urinary incontinence Embarrassing but treatable 2015 rev. What is urinary incontinence? Are there different types Urinary incontinence means that you can’t always of incontinence? control when you urinate, or pee. The amount of leakage Yes. There are five types of urinary incontinence. can be small—when you sneeze, cough, or laugh—or large, due to very strong urges to urinate that are hard to Stress incontinence is when urine leaks because of control. This can be embarrassing, but it can be treated. sudden pressure on your lower stomach muscles, such as when you cough, sneeze, laugh, rise from a Millions of adults in North America have urinary chair, lift something, or exercise. Stress incontinence incontinence. It’s most common in women over 50 years usually occurs when the pelvic muscles are weakened, of age, but it can also affect younger people, especially sometimes by childbirth, or by prostate or other pelvic women who have just given birth. surgery. Stress incontinence is common in women. Be sure to talk to your doctor if you have this problem. Urge incontinence is when the need to urinate comes on If you hide your incontinence, you risk getting rashes, too fast—before you can get to a toilet. Your body may only sores, and skin and urinary tract (bladder) infections. -

Review of Systems
code: GF004 REVIEW OF SYSTEMS First Name Middle Name / MI Last Name Check the box if you are currently experiencing any of the following : General Skin Respiratory Arthritis/Rheumatism Abnormal Pigmentation Any Lung Troubles Back Pain (recurrent) Boils Asthma or Wheezing Bone Fracture Brittle Nails Bronchitis Cancer Dry Skin Chronic or Frequent Cough Diabetes Eczema Difficulty Breathing Foot Pain Frequent infections Pleurisy or Pneumonia Gout Hair/Nail changes Spitting up Blood Headaches/Migraines Hives Trouble Breathing Joint Injury Itching URI (Cold) Now Memory Loss Jaundice None Muscle Weakness Psoriasis Numbness/Tingling Rash Obesity Skin Disease Osteoporosis None Rheumatic Fever Weight Gain/Loss None Cardiovascular Gastrointestinal Eyes - Ears - Nose - Throat/Mouth Awakening in the night smothering Abdominal Pain Blurring Chest Pain or Angina Appetite Changes Double Vision Congestive Heart Failure Black Stools Eye Disease or Injury Cyanosis (blue skin) Bleeding with Bowel Movements Eye Pain/Discharge Difficulty walking two blocks Blood in Vomit Glasses Edema/Swelling of Hands, Feet or Ankles Chrohn’s Disease/Colitis Glaucoma Heart Attacks Constipation Itchy Eyes Heart Murmur Cramping or pain in the Abdomen Vision changes Heart Trouble Difficulty Swallowing Ear Disease High Blood Pressure Diverticulosis Ear Infections Irregular Heartbeat Frequent Diarrhea Ears ringing Pain in legs Gallbladder Disease Hearing problems Palpitations Gas/Bloating Impaired Hearing Poor Circulation Heartburn or Indigestion Chronic Sinus Trouble Shortness -

Overactive Bladder
Overactive Bladder Introduction Symptoms You Might Notice “Overactive bladder” (OAB) or “unstable bladder” • A strong urge to urinate with little warning. refers to the feeling of needing to urinate much more • More frequent urination. often than is average. Since a medical name for the • Possible dribbling or loss of a large amount of urine. bladder muscle is the “detrusor,” you may also hear this • Difficulty postponing urination. This becomes a major condition called names like “detrusor overactivity” or issue for people with OAB, and can limit activities and “detrusor instability.” travel. OAB is a complex problem, but generally, the • Usually, no physical pain is associated with this bladder may contract/squeeze prematurely and hard problem, but it can be very emotionally and socially enough to make urine leak out before you can make it to disturbing. the bathroom. This type of urine loss is called “urge • Need to get up more than once at night to urinate. incontinence.” • Some people may experience an uncomfortable OAB can occur at any age. Some people are born sensation of urgency. with conditions that affect nerve and muscle signals, resulting in frequent urination, accidents, and bed Possible Causes Your Health Care Provider wetting in children. Other people may not develop OAB May Look For until they are older. The body and its muscles change • Usually no outward physical signs of OAB. with aging, making OAB quite common in older adults. • In older men, this type of bladder problem may be Additionally, certain disease processes or treatments associated with prostate enlargement. may change the bladder to be more sensitive, leading to • In older women, OAB may be related to skin, blood OAB symptoms. -
Urinary System
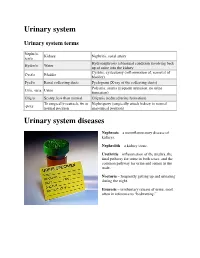
Urinary system Urinary system terms Nephr/o, Kidney Nephritis, renal artery ren/o Hydronephrosis (abnormal condition involving back Hydro/o Water up of urine into the kidney Cystitis, cystectomy (inflammation of, removal of Cyst/o Bladder bladder) Pyel/o Renal collecting ducts Pyelogram (X-ray of the collecting ducts) Polyuria, anuria (frequent urination, no urine Ur/o, -uria Urine formation) Olig/o Scanty, less than normal Oliguria (reduced urine formation) To surgically reattach, fix in Nephropexy (surgically attach kidney in normal -pexy normal position anatomical position) Urinary system diseases Nephrosis – a noninflammatory disease of kidneys. Nephrolith – a kidney stone. Urethritis – inflammation of the urethra, the final pathway for urine in both sexes, and the common pathway for urine and semen in the male. Nocturia – frequently getting up and urinating during the night. Enuresis – involuntary release of urine, most often in reference to “bedwetting.” Urinary system procedures Nephrologist – I am hoping by now, you would know this is a physician specializing in kidney diseases. Urologist – a physician specializing in the genitourinary tract, which includes kidneys, urinary bladder and urethra of both men and women and the prostate and testes in men. Cystoscopy – looking into the urinary bladder with a fiberoptic instrument. Intravenous pyelogram – special X-rays showing the drainage pattern of the kidneys. A dye opaque to X-rays is injected into a vein. After a waiting period for the blood and dye to pass through the kidneys, X-rays can be taken of the collecting system of the kidney, ureter and bladder. Retrograde pyelogram – personally, I prefer the former procedure! In this procedure a dye opaque to X-rays is flushed backwards up the urethra and bladder and up the ureters to the kidneys. -

Frequently Asked Questions About Overactive Bladder
ABOUT OAB Frequently Asked Questions about Overactive Bladder What is Overactive Bladder (OAB)? If you live with OAB, you may also: Overactive Bladder (OAB) isn’t a disease. It’s the u Leak urine (incontinence): Sometimes people name of a group of urinary symptoms. The most with OAB also have “urgency incontinence.” common symptom of OAB is a sudden urge to This means that urine leaks when you feel urinate that you can’t control. Some people will the sudden urge to go. This isn’t the same as leak urine when they feel this urge. Having to “stress urinary incontinence” or “SUI.” People urinate many times during the day and night is with SUI leak urine while sneezing, laughing or another symptom of OAB. doing other physical activities. (You can learn more about SUI at UrologyHealth.org/SUI.) How common is OAB? u Urinate frequently: You may also need to go OAB is common. It affects millions of Americans. to the bathroom many times during the day. As many as 30 percent of men and 40 percent The number of times someone urinates varies of women in the United States live with OAB from person to person. But many experts symptoms. agree that going to the bathroom more than eight times in 24 hours is “frequent urination.” Who is at risk for OAB? u Wake up at night to urinate: Waking from As you grow older, you’re at higher risk for sleep to go to the bathroom more than once a OAB. But no matter what your age, there are night is another symptom of OAB. -

Guide to Treating Your Child's Daytime Or Nighttime Accidents
A GUIDE TO TREATING YOUR CHILD’S Daytime or Nighttime Accidents, Urinary Tract Infections and Constipation UCSF BENIOFF CHILDREN’S HOSPITALS UROLOGY DEPARTMENT This booklet contains information that will help you understand more about your child’s bladder problem(s) and provides tips you can use at home before your first visit to the urology clinic. www.childrenshospitaloakland.org | www.ucsfbenioffchildrens.org 2 | UCSF BENIOFF CHILDREN’S HOSPITALS UROLOGY DEPARTMENT Table of Contents Dear Parent(s), Your child has been referred to the Pediatric Urology Parent Program at UCSF Benioff Children’s Hospitals. We specialize in the treatment of children with bladder and bowel dysfunction. This booklet contains information that will help you understand more about your child’s problem(s) and tips you can use at home before your first visit to the urology clinic. Please review the sections below that match your child’s symptoms. 1. Stool Retention and Urologic Problems (p.3) (Bowel Dysfunction) 2. Bladder Dysfunction (p.7) Includes daytime incontinence (wetting), urinary frequency and infrequency, dysuria (painful urination) and overactive bladder 3. Urinary Tract Infection and Vesicoureteral Reflux (p. 10) 4. Nocturnal Enuresis (p.12) Introduction (Nighttime Bedwetting) It’s distressing to see your child continually having accidents. The good news is that the problem is very 5. Urologic Tests (p.15) common – even if it doesn’t feel that way – and that children generally outgrow it. However, the various interventions we offer can help resolve the issue sooner THIS BOOKLET ALSO CONTAINS: rather than later. » Resources for Parents (p.16) » References (p.17) Childhood bladder and bowel dysfunction takes several forms. -

Gotta Gotta Go Right Now: a Comprehensive Assessment of Frequent Urination and Nocturnal Enuresis
Gotta Go Right Now: A Comprehensive Assessment of Frequent Urination and Nocturnal Enuresis Kelly Haack, M.A., and William J. Warzak, Ph.D. Department of Psychology, Munroe-Meyer Institute at the University of Nebraska Medical Center INTRODUCTION METHOD RESULTS Participant Bartter’s Syndrome Baseline 2 Months Following BRT ¾ Bartter’s Syndrome is caused by a defect in the kidney’s ¾ The participant was a 14-year-old male with Bartter’s Syndrome. Fluid Intake and Output Fluid Intake and Output ability to reabsorb potassium. ¾ He presented with frequent daytime and nighttime voiding. 1000 1000 ¾ As a result, the kidneys remove too much potassium from ¾ Medical History: 900 900 the body. 4 years old: Renal Ultrasound showed normal kidneys and 800 800 ¾ Excessive loss of potassium leads to muscle cramping and hypokalemia (low potassium level) was ruled out. Intake weakness, constipation, increased frequency of urination, 700 700 Intake and growth failure. 11 years old: Ditropan XL 10 mg daily and Imipramine 35 mg 600 600 daily were prescribed to treat symptoms of overactive bladder, Nocturnal Enuresis 500 500 ML such as frequent urination. ML ¾ Nocturnal Enuresis is involuntary passing of urine while 12 years old: Neurological exam was normal and neurogenic 400 400 asleep. bladder was ruled out. 300 300 Output Bartter’s Syndrome Output • Continued taking Ditropan and Imipramine. 200 200 and • Prescribed DDAVP 0.6 mg each evening to increase urine 100 100 concentration and decrease urine production. Nocturnal Enuresis 0 0 ¾ Adolescents with Bartter’s Syndrome often have a problem • Started use of a urine alarm; however, it was a short trial and 3:00 6:00 7:45 9:45 1:00 2:30 4:00 5:00 6:20 8:00 9:30 1:00 2:45 5:00 7:00 9:00 2:00 4:00 5:00 7:00 9:00 1:45 4:00 7:00 4:00 7:05 9:45 2:00 4:00 5:45 7:00 9:30 2:30 5:00 7:45 2:30 4:30 7:00 9:30 1:45 5:00 12:00 11:00 11:00 10:45 12:00 10:00 12:00 concentrating urine and excrete an excessive volume of he slept through it and continued to wet 5 out of 7 nights. -
Urinary Tract Infections
Urinary Tract Infections www.kidney.org Did you know that... n Urinary tract infections (UTIs) are responsible for nearly 10 million doctor visits each year. n One in five women will have at least one UTI in her lifetime. Nearly 20 percent of women who have a UTI will have another, and 30 percent of those will have yet another. Of this last group, 80 percent will have recurrences. n About 80 to 90 percent of UTIs are caused by a single type of bacteria. 2 NATIONAL KIDNEY FOUNDATION n UTIs can be treated effectively with medications called antibiotics. n People who get repeated UTIs may need additional tests to check for other health problems. n UTIs also may be called cystitis or a bladder infection. This brochure answers the questions most often asked about UTIs. If you have more questions, speak to your doctor. What is a urinary tract infection? A urinary tract infection is what happens when bacteria (germs) get into the urinary tract (the bladder) and multiply. The result is redness, swelling and pain in the urinary tract (see diagram). WWW.KIDNEY.ORG 3 Most UTIs stay in the bladder, the pouch-shaped organ where urine is stored before it passes out of the body. If a UTI is not treated promptly, the bacteria can travel up to the kidneys and cause a more serious type of infection, called pyelonephritis (pronounced pie-low-nef-right- iss). Pyelonephritis is an actual infection of the kidney, where urine is produced. This may result in fever and back pain. What causes a UTI? About 80 to 90 percent of UTIs are caused by a type of bacteria, called E. -

Urinary Retention in Women Workshop Chair: David Castro-Diaz, Spain 07 October 2015 08:30 - 11:30
W16: Urinary Retention in Women Workshop Chair: David Castro-Diaz, Spain 07 October 2015 08:30 - 11:30 Start End Topic Speakers 08:30 08:45 Urinary retention in women: concepts and pathophysiology David Castro-Diaz 08:45 08:50 Discussion All 08:50 09:05 Evaluation Tufan Tarcan 09:05 09:10 Discussion All 09:10 09:30 Conservative management Cristina Naranjo-Ortiz 09:30 09:35 Discussion All 09:35 09:55 Medical and surgical management Christopher Chapple 09:55 10:00 Discussion All 10:00 10:30 Break None 10:30 11:20 Typical clinical cases discussion All 11:20 11:30 Take home messages David Castro-Diaz Aims of course/workshop Urinary retention in women is rare and diverse. Diagnostic criteria are not agreed and epidemiology is not well known. Forms of urinary retention in women include: complete retention, incomplete or insufficient emptying and elevated post-void residual. It may be acute or chronic, symptomatic or asymptomatic. Etiology is multifactorial including anatomic or functional bladder outlet obstruction and bladder dysfunction related to neurological diseases, diabetes mellitus, aging, pharmacotherapy, pain and infective/inflammatory disease and idiopathic or unknown aetiology. This workshop will analyse and discuss physiopathology, evaluation and management of urinary retention in women from an integral, practical and evidence based approach. Learning Objectives 1. Identify urinary retention in women, its etiology and risk factors. 2. Carry out proper diagnosis of urinary retention in women as well as its relationship with risk and influent factors. 3. Properly manage female acute and chronic acute and chronic urinary retention with the different approaches including conservative, medical and surgical therapies.