An Unusual Variation of Abductor Digiti Minimi Manus and Its Clinical Significance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intrinsic Hand Muscles of the Japanese Monkey, Macaca Fuscata
Anthropol.Sci. 102(Suppl.), 85-95,1994 Intrinsic Hand Muscles of the Japanese Monkey, Macaca fuscata TOSHIHIKO HOMMA AND TATSUO SAKAI Department of Anatomy, School of Medicine, Juntendo University, Hongo 2-1-1, Bunkyo-ku, Tokyo 113, Japan Received December 24, 1993 •ôGH•ô Abstract•ôGS•ô Anatomy of the intrinsic hand muscles in the Japanese monkeys was studied with an improved method to dissect the muscles and nerves in water after removal of the skeletal framework. The thenar eminence contained four muscles, namely m. abductor pollicis brevis, m. opponens pollicis, m, flexor pollicis brevis, and m. adductor pollicis. The hypothenar eminence contained four muscles, namely m. palmaris brevis, m. abductor digiti minimi, m. flexor digiti minimi brevis, and m. opponens digiti minimi. Majority of the thenar muscles are fused more or less with each other, so that clear separation of these muscles was difficult. The lumbrical muscles arose from the palmar parts of four main tendons of the deep flexor muscle to the second, third, fourth, and fifth digits. The mm, contrahentes arose mainly from a medial tendinous septum attached on the palmar surface to the third metacarpus, and included three muscles destined to the second, fourth and fifth digits. The interossei were found on the radial side of the second, third, fourth and fifth finger as well as on the ulnar side of the second, third and fourth finger. The intrinsic hand muscles in the Japanese monkey received innervation either from the median or the ulnar nerve. Branching pattern of these nerves to the individual muscles was fundamentally similar to those in man except for the fact that the median and the ulnar nerve in the Japanese monkey do not communi cateto make a loop in the thenar muscles. -

Coonrad/Morrey Total Elbow Surgical Technique
Zimmer Coonrad/Morrey Total Elbow Surgical Technique Table of Contents Indications/Contraindications ................................................................................ 2 Preoperative Considerations ................................................................................... 3 Surgical Technique ................................................................................................... 4 Incision ............................................................................................................... 4 Humeral Resection ............................................................................................. 5 Preparation of the Ulna ....................................................................................... 7 Trial Reduction .................................................................................................... 9 Cement Technique .............................................................................................. 9 Humeral Bone Graft ......................................................................................... 10 Assembly and Impaction .................................................................................. 10 Closure ............................................................................................................. 11 Postoperative Management .................................................................................. 11 2 | Coonrad/Morrey Total Elbow Surgical Technique INDICATIONS & CONTRAINDICATIONS Indications include: post—traumatic -

The Muscles That Act on the Upper Limb Fall Into Four Groups
MUSCLES OF THE APPENDICULAR SKELETON UPPER LIMB The muscles that act on the upper limb fall into four groups: those that stabilize the pectoral girdle, those that move the arm, those that move the forearm, and those that move the wrist, hand, and fingers. Muscles Stabilizing Pectoral Girdle (Marieb / Hoehn – Chapter 10; Pgs. 346 – 349; Figure 1) MUSCLE: ORIGIN: INSERTION: INNERVATION: ACTION: ANTERIOR THORAX: anterior surface coracoid process protracts & depresses Pectoralis minor* pectoral nerves of ribs 3 – 5 of scapula scapula medial border rotates scapula Serratus anterior* ribs 1 – 8 long thoracic nerve of scapula laterally inferior surface stabilizes / depresses Subclavius* rib 1 --------------- of clavicle pectoral girdle POSTERIOR THORAX: occipital bone / acromion / spine of stabilizes / elevates / accessory nerve Trapezius* spinous processes scapula; lateral third retracts / rotates (cranial nerve XI) of C7 – T12 of clavicle scapula transverse processes upper medial border elevates / adducts Levator scapulae* dorsal scapular nerve of C1 – C4 of scapula scapula Rhomboids* spinous processes medial border adducts / rotates dorsal scapular nerve (major / minor) of C7 – T5 of scapula scapula * Need to be familiar with on both ADAM and the human cadaver Figure 1: Muscles stabilizing pectoral girdle, posterior and anterior views 2 BI 334 – Advanced Human Anatomy and Physiology Western Oregon University Muscles Moving Arm (Marieb / Hoehn – Chapter 10; Pgs. 350 – 352; Figure 2) MUSCLE: ORIGIN: INSERTION: INNERVATION: ACTION: intertubercular -

Forearm and Carpal Tunnel
FOREARM AND CARPAL TUNNEL Prof. AO Ihunwo, PhD School of Anatomical Sciences Constituents of the Forearm • Bones • Radius and Ulna • Muscles • Flexors (anterior compartment) • Extensors (posterior compartment) • Blood vessels • Ulnar and Radial • Nerves Anterior (Flexor) Compartment Muscles - Superficial Group: • Cross elbow joint. • Possess a common origin (anterior surface of medial epicondyle of humerus). • Lateral to medial • Pronator teres (1) • Flexor Carpi Radialis (FCR) 2 • Flexor Digitorum Superficialis (FDS) 3 • Palmaris longus 4 • Flexor Carpi Ulnaris (FCU) 5 • Nerve supply – Median nerve except FCU (ulnar nerve) Flexor Compartment.. Deep Group: • Do not have a common origin. • Do not cross elbow joint. • Flexor Digitorum Profundus FDP (FDP) FPL • most powerful & bulkiest muscles. • Median nerve to lateral half & ulnar nerve to medial half • Flexor Pollicis Longus (FPL) PQ median nerve • Pronator quadratus • median nerve Actions of muscles in flexor compartment • Pronators of forearm • Pronator teres and Pronator Quadratus • Supinator of forearm • Supinator • Flexors of wrist • FCR (+ abduction), FCU ( + adduction) at wrist • Flexors of fingers • FDS (middle phalages) and FDP (distal phalanges) • Flexors of thumb • FPL Posterior (Extensor) Compartment Muscles – Divided into 3 groups based on origin Group A: Lateral supracondylar ridge of humerus. • Brachioradialis & ECRL. • Nerve Supply – Radial nerve Group B: Lateral epicondyle • ECRB. ED, ECU, Anconeus, Supinator & EDM. • Nerve Supply – Posterior interosseous nerve (radial nerve) Group C: Radius, ulna & interrosseous membrane • AbPL, EPL, EPB. • Nerve Supply – Posterior interosseous nerve (radial nerve). Extensor Compartment… • Extensors of wrist • ECRL, ECRB, ECU • Extensors of fingers • ED, EId, EDM • Extensors of thumb • EPL • EPB • Abductor of thumb • AbPL Nerves of Forearm • Median • Ulnar & • Radial Nerves • Review their origin and distribution from the cords of the brachial plexus Arteries of the forearm • Ulnar artery is main artery of forearm • Radial artery is for the hand. -

This Sumarry Is Only for the Muscles of the Hand (Slides: 14-33) Please Refer to the First 13 Slide When Studying
This sumarry is only for the muscles of the hand (slides: 14-33) please refer to the first 13 slide when studying. For The innervation of these muscles its easier to memorize them from the last paragraph in the last page Muscle Origin Insertion Nerve Action Image 1st and 2nd, Flexmetacarpoph (lateral two) alangeal (MP) Extensor Tendons of flexor median nerve; joints & extend Lumbricals expansion of Digitorum 3rd and 4th interphalangeal (4 muscles) medial four profundus medial deep (IP) joints of fingers branch of ulnar fingers except nerve thumb -First arises from Proximal base of 1st phalanges of metacarpal thumb and index, Palmar adduct fingers - remaining three ring, and little Deep branch of Interossei toward center of from anterior fingers and ulnar nerve (4 muscles) third finger surface of shafts dorsal extensor of 2nd, 4th, and expansion of 5th metacarpals each finger . Proximal phalanges of index, middle, and ring fingers Contiguous sides abduct fingers Dorsal Interossei and dorsal Deep branch of of shafts of from center of (4 muscles) extensor ulnar nerve metacarpal bones third finger expansion (1st:index\ 2nd,3rd:middle \ 4th:ring) Both palmar and dorsal: -Flex metacarpophalangeal joints -Extend interphalangeal joints Simultaneous flexion at the metacarpophalangeal joints and extension at the interphalangeal joints of a digit are essential for the fine movements of writing, drawing, threading a needle, etc. The Lumbricals and interossei have long been accepted as not only primary agents in flexing the metacarpophalangeal joints -

ISPUB.COM Volume 9 Number 2
The Internet Journal of Surgery ISPUB.COM Volume 9 Number 2 An Anomalous Palmaris Brevis Muscle and its Clinical Implications S Das, S Paul Citation S Das, S Paul. An Anomalous Palmaris Brevis Muscle and its Clinical Implications. The Internet Journal of Surgery. 2006 Volume 9 Number 2. Abstract The palmaris brevis (PB) muscle is a small, thin, subcutaneous muscle of the palm. The palmaris brevis muscle is important muscle contributing to the grip of the hand. In the present case, during routine cadaveric dissection, we detected a PB muscle which was not subcutaneous but existed as a muscle deep to the dermis of the skin of the palm. The PB muscle stretched as a horizontal band over the hypothenar muscles of the palm. The anomalous location of the PB may result in compression of neurovascular structures on the ulnar side of the palm. The awareness of such anomalous muscle which is not subcutaneous, may be clinical important for surgeons operating on the hand and clinicians diagnosing compressive symptoms. INTRODUCTION Figure 1 The PB muscle is a thin subcutaneous muscle. The PB arises Figure 1: Photograph of dissected right palm showing from the flexor retinaculum and the medial border of the central part of the palmar aponeurosis and attached to the dermis of the skin on the ulnar side of the palm. 1 The PB is innervated by the ulnar nerve and the main action of the muscle makes the palmar grip more secure. 1 The clinical importance of the muscle lies in the fact, that it lies above the ulnar artery and the ulnar nerve in the palm. -

Neuroanatomy for Nerve Conduction Studies
Neuroanatomy for Nerve Conduction Studies Kimberley Butler, R.NCS.T, CNIM, R. EP T. Jerry Morris, BS, MS, R.NCS.T. Kevin R. Scott, MD, MA Zach Simmons, MD AANEM 57th Annual Meeting Québec City, Québec, Canada Copyright © October 2010 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 Printed by Johnson Printing Company, Inc. AANEM Course Neuroanatomy for Nerve Conduction Studies iii Neuroanatomy for Nerve Conduction Studies Contents CME Information iv Faculty v The Spinal Accessory Nerve and the Less Commonly Studied Nerves of the Limbs 1 Zachary Simmons, MD Ulnar and Radial Nerves 13 Kevin R. Scott, MD The Tibial and the Common Peroneal Nerves 21 Kimberley B. Butler, R.NCS.T., R. EP T., CNIM Median Nerves and Nerves of the Face 27 Jerry Morris, MS, R.NCS.T. iv Course Description This course is designed to provide an introduction to anatomy of the major nerves used for nerve conduction studies, with emphasis on the surface land- marks used for the performance of such studies. Location and pathophysiology of common lesions of these nerves are reviewed, and electrodiagnostic methods for localization are discussed. This course is designed to be useful for technologists, but also useful and informative for physicians who perform their own nerve conduction studies, or who supervise technologists in the performance of such studies and who perform needle EMG examinations.. Intended Audience This course is intended for Neurologists, Physiatrists, and others who practice neuromuscular, musculoskeletal, and electrodiagnostic medicine with the intent to improve the quality of medical care to patients with muscle and nerve disorders. -

Section 1 Upper Limb Anatomy 1) with Regard to the Pectoral Girdle
Section 1 Upper Limb Anatomy 1) With regard to the pectoral girdle: a) contains three joints, the sternoclavicular, the acromioclavicular and the glenohumeral b) serratus anterior, the rhomboids and subclavius attach the scapula to the axial skeleton c) pectoralis major and deltoid are the only muscular attachments between the clavicle and the upper limb d) teres major provides attachment between the axial skeleton and the girdle 2) Choose the odd muscle out as regards insertion/origin: a) supraspinatus b) subscapularis c) biceps d) teres minor e) deltoid 3) Which muscle does not insert in or next to the intertubecular groove of the upper humerus? a) pectoralis major b) pectoralis minor c) latissimus dorsi d) teres major 4) Identify the incorrect pairing for testing muscles: a) latissimus dorsi – abduct to 60° and adduct against resistance b) trapezius – shrug shoulders against resistance c) rhomboids – place hands on hips and draw elbows back and scapulae together d) serratus anterior – push with arms outstretched against a wall 5) Identify the incorrect innervation: a) subclavius – own nerve from the brachial plexus b) serratus anterior – long thoracic nerve c) clavicular head of pectoralis major – medial pectoral nerve d) latissimus dorsi – dorsal scapular nerve e) trapezius – accessory nerve 6) Which muscle does not extend from the posterior surface of the scapula to the greater tubercle of the humerus? a) teres major b) infraspinatus c) supraspinatus d) teres minor 7) With regard to action, which muscle is the odd one out? a) teres -
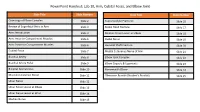
Powerpoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint
PowerPoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint Slide Title Slide Number Slide Title Slide Number Osteology of Elbow Complex Slide 2 Supracondylar Fractures Slide 16 Review of Superficial Veins in Arm Slide 3 Radial Head Fracture Slide 17 Arm: Introduction Slide 4 Median Nerve Lesion at Elbow Slide 18 Arm: Anterior Compartment Muscles Slide 5 Radial Nerve Slide 19 Arm: Posterior Compartment Muscles Slide 6 Humeral Shaft Fracture Slide 20 Cubital Fossa Slide 7 Medial Cutaneous Nerve of Arm Slide 21 Brachial Artery Slide 8 Elbow Joint Complex Slide 22 Brachial Artery Pulse Slide 9 Elbow Capsule & Ligaments Slide 23 Bicipital Aponeurosis Slide 10 Nursemaid’s Elbow Slide 24 Musculocutaneous Nerve Slide 11 Olecranon Bursitis (Student’s Bursitis) Slide 25 Ulnar Nerve Slide 12 Ulnar Nerve Lesion at Elbow Slide 13 Ulnar Nerve Lesion at Wrist Slide 14 Median Nerve Slide 15 Osteology of Elbow Complex To adequately review the learning objectives covering osteology of the distal humerus, radius, and ulna, view the Lower Limb Osteology and Medical Imaging Guide. Review of Superficial Veins in Arm The cephalic and basilic veins are the main superficial veins of the upper limb. They originate from the dorsal venous network on the dorsum of the hand. • The cephalic vein ascends along the anterolateral aspect of the forearm and arm. It then follows the superior border of the pectoralis major muscle to enter the deltopectoral triangle. It ultimately joins the axillary vein after passing through the clavipectoral fascia. • The basilic vein ascends along the medial forearm and the arm. In the arm, it passes deep to the brachial fascia where it courses in close proximity to the brachial artery and medial cutaneous nerve of the forearm along its path into the axilla. -

The Bicipital Aponeurosis
Surg Radiol Anat DOI 10.1007/s00276-017-1885-0 ORIGINAL ARTICLE Ultrasound visualization of an underestimated structure: the bicipital aponeurosis 1 1 1 M. Konschake • H. Stofferin • B. Moriggl Received: 15 February 2017 / Accepted: 31 May 2017 Ó The Author(s) 2017. This article is an open access publication Abstract the BA. Therefore, we suggest additional BA scanning during Purpose We established a detailed sonographic approach to clinical examinations of several pathologies, not only for BA the bicipital aponeurosis (BA), because different pathologies augmentation procedures in distal biceps tendon tears. of this, sometimes underestimated, structure are associated with vascular, neural and muscular lesions; emphasizing its Keywords Bicipital aponeurosis Á Lacertus fibrosus Á further implementation in routine clinical examinations. Biceps brachii muscle Á Ultrasonography Methods The BA of 100 volunteers, in sitting position with the elbow lying on a suitable table, was investigated. Patients were aged between 18 and 28 with no history of Introduction distal biceps injury. Examination was performed using an 18–6 MHz linear transducer (LA435; system MyLab25 by The biceps brachii muscle (BM) is attached distally to the Esaote, Genoa, Italy) utilizing the highest frequency, radial tuberosity via the strong biceps tendon (BT) and to scanned in two planes (longitudinal and transverse view). the antebrachial fascia via the bicipital aponeurosis (BA), In each proband, scanning was done with and without also known as lacertus fibrosus. As previously described, isometric contraction of the biceps brachii muscle. the BT consists of two distinct portions separated by an Results The BA was characterized by two clearly distin- endotenon septum and surrounded by a common paratenon, guishable white lines enveloping a hypoechoic band. -

Compressive Mononeuropathies of the Upper Extremity in Chronic Paraplegia
ParapkgW 29 (1991) 17-24 © 1991 International Medical Society of Paraplegia Paraplegia Compressive Mononeuropathies of the Upper Extremity in Chronic Paraplegia G. Davidoff, MD, R. Werner, MD, W. Waring, MD Department of Physical Medicine and Rehabilitation, University of Michigan Medical Center, and Rehabilitation Medicine Service, Veterans Affairs Medical Center, Ann Arbor, Michigan, USA. Summary Controversy exists with regard to the actual prevalence of compressive mononeuropathies at the wrist which may occur following chronic paraplegia. Thirty one chronic paraplegics, with a mean age of 37'9 years (range 20-68 years), and mean time since injury of 9'7 years (range 1-28 years), were studied with a comprehensive neurologic and electrodiagnostic (EDX) assessment. No patient had any clinical or EDX evidence of a peripheral polyneuropathy. The diagnosis of a median mononeuropathy at the wrist was determined by the following criteria: (a) prolonged median sensory distal latency > ipsilateral ulnar sensory distal latency 2 0·5 msec; (b) a median mid-palmar sensory latency> ipsilateral ulnar mid-palmar sensory latency of 2 0'3 msec; or (c) a median motor distal latency 2 l' 7 milliseconds as compared to the ipsilateral ulnar motor distal latency. Ulnar mononeuropathy at the wrist or across the elbow was also characterised. The EDX criteria for a median mononeuropathy at the wrist was met in 55% of subjects (24% of these with bilateral presentations). The location of ulnar mononeuropathies included: two at the superficial sensory branch at the wrist, one at the deep motor branch at the wrist, and three patients with a conduction block across the elbow. -

Neuroanatomy of NCS
Neuroanatomy of NCS Jerry Morris, CNCT, MS, R.NCS.T. William S. David, MD, PhD presenting for Kevin Scott, MD, MA Kimberley B. Butler, CNCT, R.NCS.T, R.EPT, CNIM Zachary Simmons, MD AANEM 59th Annual Meeting Orlando, Florida Copyright © September 2012 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 Printed by Johnson’s Printing Company, Inc. 1 Please be aware that some of the medical devices or pharmaceuticals discussed in this handout may not be cleared by the FDA or cleared by the FDA for the specific use described by the authors and are “off-label” (i.e., a use not described on the product’s label). “Off-label” devices or pharmaceuticals may be used if, in the judgment of the treating physician, such use is medically indicated to treat a patient’s condition. Information regarding the FDA clearance status of a particular device or pharmaceutical may be obtained by reading the product’s package labeling, by contacting a sales representative or legal counsel of the manufacturer of the device or pharmaceutical, or by contacting the FDA at 1-800-638-2041. 2 Neuroanatomy of NCS Table of Contents Course Committees & Course Objectives 4 Faculty 5 Median and Facial Nerves—Anatomy, Techniques, and Applications 7 Jerry Morris, CNCT, MS, R.NCS.T. Ulnar and Radial Nerves 17 William S. David, MD, PhD presenting for Kevin Scott, MD, MA The Tibial & the Common Peroneal Nerves 25 Kimberley B. Butler, CNCT, R.NCS.T, R.EPT, CNIM The Spinal Accessory Nerve and the Less Commonly Studied Nerves of the Limbs 29 Zachary Simmons, MD CME Questions 41 No one involved in the planning of this CME activity had nay relevant financial relationships to disclose.