The Bicipital Aponeurosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Section 1 Upper Limb Anatomy 1) with Regard to the Pectoral Girdle
Section 1 Upper Limb Anatomy 1) With regard to the pectoral girdle: a) contains three joints, the sternoclavicular, the acromioclavicular and the glenohumeral b) serratus anterior, the rhomboids and subclavius attach the scapula to the axial skeleton c) pectoralis major and deltoid are the only muscular attachments between the clavicle and the upper limb d) teres major provides attachment between the axial skeleton and the girdle 2) Choose the odd muscle out as regards insertion/origin: a) supraspinatus b) subscapularis c) biceps d) teres minor e) deltoid 3) Which muscle does not insert in or next to the intertubecular groove of the upper humerus? a) pectoralis major b) pectoralis minor c) latissimus dorsi d) teres major 4) Identify the incorrect pairing for testing muscles: a) latissimus dorsi – abduct to 60° and adduct against resistance b) trapezius – shrug shoulders against resistance c) rhomboids – place hands on hips and draw elbows back and scapulae together d) serratus anterior – push with arms outstretched against a wall 5) Identify the incorrect innervation: a) subclavius – own nerve from the brachial plexus b) serratus anterior – long thoracic nerve c) clavicular head of pectoralis major – medial pectoral nerve d) latissimus dorsi – dorsal scapular nerve e) trapezius – accessory nerve 6) Which muscle does not extend from the posterior surface of the scapula to the greater tubercle of the humerus? a) teres major b) infraspinatus c) supraspinatus d) teres minor 7) With regard to action, which muscle is the odd one out? a) teres -
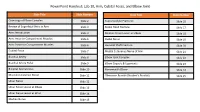
Powerpoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint
PowerPoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint Slide Title Slide Number Slide Title Slide Number Osteology of Elbow Complex Slide 2 Supracondylar Fractures Slide 16 Review of Superficial Veins in Arm Slide 3 Radial Head Fracture Slide 17 Arm: Introduction Slide 4 Median Nerve Lesion at Elbow Slide 18 Arm: Anterior Compartment Muscles Slide 5 Radial Nerve Slide 19 Arm: Posterior Compartment Muscles Slide 6 Humeral Shaft Fracture Slide 20 Cubital Fossa Slide 7 Medial Cutaneous Nerve of Arm Slide 21 Brachial Artery Slide 8 Elbow Joint Complex Slide 22 Brachial Artery Pulse Slide 9 Elbow Capsule & Ligaments Slide 23 Bicipital Aponeurosis Slide 10 Nursemaid’s Elbow Slide 24 Musculocutaneous Nerve Slide 11 Olecranon Bursitis (Student’s Bursitis) Slide 25 Ulnar Nerve Slide 12 Ulnar Nerve Lesion at Elbow Slide 13 Ulnar Nerve Lesion at Wrist Slide 14 Median Nerve Slide 15 Osteology of Elbow Complex To adequately review the learning objectives covering osteology of the distal humerus, radius, and ulna, view the Lower Limb Osteology and Medical Imaging Guide. Review of Superficial Veins in Arm The cephalic and basilic veins are the main superficial veins of the upper limb. They originate from the dorsal venous network on the dorsum of the hand. • The cephalic vein ascends along the anterolateral aspect of the forearm and arm. It then follows the superior border of the pectoralis major muscle to enter the deltopectoral triangle. It ultimately joins the axillary vein after passing through the clavipectoral fascia. • The basilic vein ascends along the medial forearm and the arm. In the arm, it passes deep to the brachial fascia where it courses in close proximity to the brachial artery and medial cutaneous nerve of the forearm along its path into the axilla. -

Morphology of the Bicipital Aponeurosis: a Cadaveric Study S.D
Folia Morphol. Vol. 73, No. 1, pp. 79–83 DOI: 10.5603/FM.2014.0011 O R I G I N A L A R T I C L E Copyright © 2014 Via Medica ISSN 0015–5659 www.fm.viamedica.pl Morphology of the bicipital aponeurosis: a cadaveric study S.D. Joshi, A.S. Yogesh, P.S. Mittal, S.S. Joshi Department of Anatomy, Sri Aurobindo Medical College and Postgraduate Institute, Indore, India [Received 17 May 2013; Accepted 2 July 2013] The bicipital aponeurosis (BA) is a fascial expansion which arises from the ten- don of biceps brachii and dissipates some of the force away from its enthesis. It helps in dual action of biceps brachii as supinator and flexor of forearm. The aim of the present work was to study the morphology of BA. Thirty cadaveric upper limbs (16 right and 14 left side limbs) were dissected and dimensions of the BA were noted. The average width of aponeurosis at its commencement on the right was 15.74 mm while on the left it was 17.57 mm. The average angle between tendon and aponeurosis on the right was 21.16° and on the left it was 21.78°. The fibres from the short head of the biceps brachii contributed to the formation of proximal part of aponeurosis. Fascial sheath over the tendon of long head of biceps brachii was seen to form the distal part of the aponeurosis. In 5 cases, large fat globules were present between the sheath and the tendon. Histologically: The aponeurosis showed presence of thick collagen bundles. -

Bilateral Reversed Palmaris Longus Muscle: a Rare Anatomical Variation
Folia Morphol. Vol. 71, No. 1, pp. 52–55 Copyright © 2012 Via Medica C A S E R E P O R T ISSN 0015–5659 www.fm.viamedica.pl Bilateral reversed palmaris longus muscle: a rare anatomical variation G. Salgado1, M. Cantín2, O. Inzunza1, A. Muñoz1, J. Saez1, M. Macuer1 1Department of Normal Anatomy, Pontificia Universidad Católica de Chile, Faculty of Medicine, Santiago, Chile 2Department of Integral Odontology, Doctoral Program in Morphological Sciences, Faculty of Odontology, Faculty of Medicine, Universidad de La Frontera, Temuco, Chile [Received 8 September 2011; Accepted 23 October 2011] We report a case of bilateral reversed palmaris longus muscle (PLM). The mus- cle was tendinous in its upper portion and muscular in its lower portion in both arms. This rare variation has been mentioned only once in the literature as a surgical finding. According to the literature, a reversed PLM may cause a com- partment syndrome in the wrist area, carpal tunnel, and Guyon’s syndrome. The described variation is also useful to the hand surgeon as a tendon graft, a tendon for transfer, or as an anatomical landmark for operations at this area. (Folia Morphol 2012; 71, 1: 52–55) Key words: palmaris longus muscle, reversed muscle, anatomical variation, forearm INTRODUCTION The PLM is extremely variable. Its most frequent The palmaris longus muscle (PLM) is a fusiform variation is agenesis, reported in 12.8% of the po- and thin muscle that lies medial to the flexor carpi pulation [10, 15]. Other variations include differenc- radialis (FCR) muscle. It shares a common origin with es in shape and position described as central, in- the flexor superficialis digitorum (FSD) muscle, the verted, bifid, duplicated [11], and even triplicated flexor carpi ulnaris (FCU) muscle, and the FCR, in the [7, 15]. -

Additional Muscle Slips from the Bicipital Aponeurosis and a Long Communicating Branch Between the Musculocutaneous and the Median Nerves
eISSN 1308-4038 International Journal of Anatomical Variations (2012) 5: 41–43 Case Report Additional muscle slips from the bicipital aponeurosis and a long communicating branch between the musculocutaneous and the median nerves Published online October 12th, 2012 © http://www.ijav.org Kumar MR BHAT Abstract Vinay KULAKARNI Additional muscle slips from the bicipital aponeurosis both to pronator teres and flexor carpi radialis muscles are uncommon and not been reported. Here, we report a case of presence of Chandni GUPTA tendentious slip arising from the under surface of the bicipital aponeurosis in the cubital fossa in the left upper limb of a 72-year-old male cadaver. This tendineous slip was then divided into two separate muscular heads for the pronator teres and flexor carpi radialis muscles. Department of Anatomy, Kasturba Medical College, Additionally, in the same cadaver we also found an unusual long communicating branch from the Manipal University, Manipal, INDIA. musculocutaneous nerve in the upper arm, which had long course through the arm before joining the median nerve in the cubital fossa. This report discusses the details of these variations, their clinical implication and embryological explanations. Dr. Kumar MR Bhat © Int J Anat Var (IJAV). 2012; 5: 41–43. Associate Professor Department of Anatomy Kasturba Medical College Manipal University Manipal, 576104, INDIA. +91 (820) 2922327 [email protected] Received April 15th, 2011; accepted January 17th, 2012 Key words [pronator teres] [flexor carpi radialis] [musculocutaneous nerve] [communicating branch] [additional head] Introduction of pronator teres and flexor carpi radialis (2.08%). This Pronator teres usually originates as two heads, the superficial additional muscle was originated as tendineous slip from humeral head from medial epicondyle and the deep ulnar head the undersurface of the aponeurotic extension of the biceps from the coronoid process. -

Anatomical Study of Myofascial Continuity in the Anterior Region of the Upper Limb
ARTICLE IN PRESS Journal of Bodywork and Movement Therapies (2009) 13,53–62 Journal of Bodywork and Movement Therapies www.intl.elsevierhealth.com/journals/jbmt HUMAN ANATOMY Anatomical study of myofascial continuity in the anterior region of the upper limb Antonio Steccoa, Veronica Macchib, Carla Steccoc, Andrea Porzionatob, Julie Ann Dayd, Vincent Delmase, Raffaele De Carob,Ã aPhysical Medicine and Rehabilitation Clinic, University of Padova, Italy bSection of Anatomy, Department of Human Anatomy and Physiology, University of Padova, Italy cSection of Orthopedics, Department of Medical Surgical Specialisations, University of Padova, Italy dPhysical Medicine and Rehabilitation Clinic, Ospedale dei Colli, Padova, Italy eInstitut d’Anatomie, Universite´ Paris Descartes, France Received 18 March 2007; received in revised form 27 April 2007; accepted 27 April 2007 KEYWORDS Summary Fifteen unembalmed cadavers were dissected in order to study the Myofascial ‘‘anatomical continuity’’ between the various muscles involved in the movement of continuity; flexion of the upper limb. This study demonstrated the existence of specific Fascia; myofascial expansions, with a nearly constant pattern, which originate from the Proprioception; flexor muscles and extend to the overlying fascia. The clavicular part of the Chaıˆnes musculaires; pectoralis major sends a myofascial expansion, with a mean length of 3.6 cm, to Meridians; the anterior region of the brachial fascia, and the costal part sends one to the Anatomy trains; medial region of the brachial fascia (mean length: 6.8 cm). The biceps brachii Sequences presents two expansions: the lacertus fibrosus, oriented medially, with a mean height of 4.7 cm and a base of 1.9 cm, and a second, less evident, longitudinal expansion (mean length: 4.5 cm, mean width: 0.7 cm). -

Elbow Tendinopathies • Defined As Non-Inflammatory Intratendinous Collagen Degeneration Bernard F
Tendinosis Elbow Tendinopathies • Defined as non-inflammatory intratendinous collagen degeneration Bernard F. Hearon, M.D. Clinical Assistant Professor, Department of Surgery • Angiofibroblastic hyperplasia - University of Kansas School of Medicine - Wichita hypertrophic fibroblasts, vascular April 23, 2019 hyperplasia, disorganized collagen • Areas of focal necrosis, calcification • No acute inflammatory cells Elbow Tendinopathies Distal Biceps Potential Mechanisms of Rupture: Arterial Supply, Mechanical Impingement. Seiler Tendinosis vs Tendinitis et al., JSES 1995; 4: 149-56. • “Tendinosis” implies an intrinsic degenerative • Proximal one-third supplied by brachial artery condition, determines therapeutic goals, sets • Distal one-third from posterior interosseous reasonable outcome expectations recurrent artery • “Tendinitis” implies an inflammatory condition, • 2-cm middle-third is a hypovascular zone where is misleading, allows misguided treatment & blood supply is from paratenon unreasonable expectations • Radioulnar space for tendon is 48% less in pronation than in supination • Basic Science study (Emory University) Elbow Tendinopathies Elbow Tendinopathies Read File Distal Biceps Ruptures Bilateral ruptures of the distal biceps brachii tendon Epidemiology Schneider et al., JSES 2009; 18: 804-07. • 25 pts, non-simultaneous bilateral biceps ruptures • Male mesomorphs (rare in females) • All pts male, average age 50 (range 28 to 76) Age range 30-60 years (mean age 47) • • Mean time between ruptures 2.7 yrs (0.5 to 6.3) • Dominant extremity (86%) • Pts found to have higher rate of nicotine (50%) • Incidence 1.2 ruptures / 100K / year (rare) and anabolic steroid use (20%) • Smokers 7.5 times greater risk • Therapeutic Level IV study (Fondren, Houston) Elbow Tendinopathies Elbow Tendinopathies Read File Distal biceps tendon insertion: An anatomic study Distal Biceps Anatomy Hutchinson et al., JSES 2008; 17: 342-46. -

Entrapment of the Median Nerves and Brachial Arteries in the Lower Arms Bilaterally and Additional Origin of Biceps Brachii Muscle
Int. J. Morphol., 28(4):1241-1244, 2010. Entrapment of the Median Nerves and Brachial Arteries in the Lower Arms Bilaterally and Additional Origin of Biceps brachii Muscle. Case Report Compresión Bilateral del Nervio Mediano y de la Arteria Braquial en la Parte Distal del Brazo y Origen Adicional del Músculo Bíceps Braquial. Reporte de Caso Niladri Kumar Mahato MAHATO, N. K. Entrapment of the median nerves and brachial arteries in the lower arm bilaterally and additional origin of biceps brachii muscle. Case report. Int. J. Morphol., 28(4):1241-1244, 2010. SUMMARY: Neuro-vascular entrapments associated with variations observed in the origins of muscles in the arm are not uncommon. Though additional heads of biceps brachii muscle and extra fibres of brachialis muscles have been demonstrated earlier, bilateral additional heads of the biceps are rarely seen, especially with entrapment of the median nerve and the brachial arteries in both the arms. The present study reports conspicuous heads of the biceps brachii originating extensively from the medial inter-muscular septum, sharing its origin with the brachialis muscle. The extra origins of the muscle formed long musculo-aponeurotic tunnels. The tunnels measured eight centimeters in length extending from the lower arm to the cubital-fossa. Both the median nerve and the brachial arteries passed through the tunnel. The lower aspect of the left tunnel exhibited origins of fibres belonging to the superficial flexors of the forearm. The neuro-vascular structures did not give any branches in the tunnel. Awareness of such variations can aid clinicians in diagnosing and treating such neuropathies and vascular compromise. -

Showing a Thickened Bicipital Aponeurosis Tence of a Trigeminal Artery Provides Some Flexor Digitorum Profundus, Abductor Compressing the Nervous Trunk
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.45.2.181 on 1 February 1982. Downloaded from Letters 181 at the elbow gives rise to a compression aponeurosis can be causative factors of neuropathy commonly called the pronator this syndrome.5 7 8 Radiographs excluded syndrome.1-5 We studied a patient the presence of a bony supracondylar presenting this symptom-complex caused prozess. Clinically it is not always possible by a thickened bicipital aponeurosis to assess if an entrapment is caused by the compressing the median nerve. Struthers ligament or by the bicipital A 55-year-old brick-layer noted weak- aponeurosis. Our patient's symptoms ness of his left hand and numbness of the represented the common features of the thumb, second and third finger, associated entrapment of the median nerve above the with pain at the left wrist, forearm and elbow, but did not give any suggestion arm. These symptoms had an acute onset about the structure restraining it. after a day in which the patient had Some manoeuvres are described which carried heavy building material supported are supposed to be suggestive of the exact on his left forearm. When admitted, two site of the compression :27 the entrapment months later, examination revealed a by the Struthers ligament is described as slight wasting of the thenar eminence and usually associated with forearm pain of the volar aspect of the forearm. Tinel's elicited or increased during forceful sign over the median nerve at the elbow extension of the wrist, while reproduction was positive. There was weakness of the of pain by resistence to forearm supination pronator teres, flexor digitorum sublimis, and elbow flexion is considered a positive flexor digitorum profundus to the second sign for entrapment at the bicipital and third finger, flexor pollicis longus, aponeurosis. -

Anatomy of the Hand Bones of the Hand
Topics Anatomy of the Hand • Surface Anatomy • Bony Anatomy Diane Coker, PT, DPT, CHT • Joints & Ligaments • Muscular Anatomy • Tendon Anatomy University of California, Irvine •Flexors Irvine, CA •Extensors February 9-11, 2018 • Neuroanatomy • Thumb Surface Topography P3 • Joint flexion creases P2 • DPC • Thenar crease DIP • Hypothenar crease P1 • Digital creases PIP • Distal wrist creases DPC = MP joint volar crease (prox • Muscle groups & distal palmar • Thenar crease) • Hypothenar IP • Rays • 1 - 5 Bones of the Hand Bony Anatomy Metacarpal Cascade • 19 bones distal to the carpus • Metacarpals (5) . Numbered • Phalanges (12) • Proximal (P1) • Middle (P2) • Distal (P3) • Thumb phalanges (2) Structural Units • Fixed Unit • Distal carpal row • Metacarpals 2 & 3 • 3 mobile units • Thumb ray • Index finger ray • Metacarpals 4 & 5, with long, ring, & little fingers Green: Mobile Units Red: Fixed Units Types of Joints Joints and Articulations (condyloid) Joints in the Hand Fixed and Mobile Units • Saddle: Carpometacarpal (CMC) • Ellipsoidal: • “Ulnar” opposition Metacarpophalangeal (MP or MCP) • 20-30° at SF • 10-15° at RF • Hinge: Interphalangeal (IP) • Plane: Hamate and • Less mobility at MCs Triquetrum II & III thought to be a • Not represented: ball and functional adaptation socket to enhance ECRL/B & FCR activity MCP Joints • Condyloid (Ellipsoid)Joints • flexion/extension P1 • abduction/adduction • IF sl rotation • Motion increases radial to ulnar in digits • 0/90‐110⁰ MC • Hyperextension varies Green: Mobile Units among individual Red: -

Arm & Cubital Fossa
Arm & Cubital Fossa Dr Brijendra Singh MBBS,MS,DNB,MNAMS Professor & HoD Anatomy AIIMS Rishikesh Learning Objectives • At end of this session, students should be able to: • DESCRIBE • Attachments, actions & innervations of - biceps brachii, coracobrachialis, brachialis, triceps brachii • Contents of ant & post compartment of arm , their anatomical Relations and clinical importance • Boundaries of cubital fossa and its contents. Medial Intermuscular Septum •From subcutaneous sheath to humerus. •Separates muscles of anterior arm from medial side of triceps complex. •Lateral Intermuscular Septum •From subcutaneous sheath to humerus. •Separates muscles of anterior arm from lateral side of triceps complex. Anterior Brachial Compartment BBC – Musculocutaneous nerve Muscles •Components: Biceps brachii Coracobrachialis Brachialis • Function: Forearm flexors Biceps also supinates forearm Innervation •Musculocutaneous nerve C5-6 •Nerves passing through compartment - But not innervating anterior compartment structures are : Median & Ulnar nerve Through proximal part of anterior compartment. •Blood supply – •Brachial artery •Basilic vein and venae comitantes Posterior compartment Triceps & anconeus – Radial Nerve Muscles •Components: •Triceps brachii. •Anconeus. •Function: •Forearm extensors. •Long head of triceps can extend shoulder (arm). •Synergists in forearm supination. •Innervation/Vascularization •Radial nerve C7 •Deep brachial artery Nerves and Vessels in Arm Median Nerve •Supplies flexor muscles on radial side of forearm. •Travels with brachial artery: •upper half - Lateral to brachial artery. •lower half - Medial to brachial artery . •Crosses cubital fossa superficially: •With brachial artery & •Deep to bicipital aponeurosis Ulnar Nerve •Supplies flexor muscles on ulnar side of forearm. •Starts in anterior brachial compartment - MC •Medial to brachial artery •Runs with superior ulnar collateral artery. •Pierces medial intermuscular septum: •Enters posterior compartment of arm. -

An Unusual Variation of Abductor Digiti Minimi Manus and Its Clinical Significance
IJAE Vol. 123, n. 3: 189-193, 2018 ITALIAN JOURNAL OF ANATOMY AND EMBRYOLOGY Research Article - Human Anatomy Case Report An unusual variation of abductor digiti minimi manus and its clinical significance Álvaro R. Teixeira*, Albino J. Fonseca, Márcio A. Babinski, Lucas A.S. Pires, Carlos A.A. Chagas Anatomy Laboratory, Morphology Department, Biomedical Institute, Fluminense Federal University, Rio de Janeiro, Brazil Abstract The abductor digiti minimi manus muscle usually has two heads and two insertions, often close to each other. Accessory bellies of this muscle have been vastly described in anatomy text- books. During routine dissection of an adult male cadaver left forearm and hand we observed a rare variation of this muscle, in which there was an accessory muscle band which originated from the palmaris longus muscle tendon and traversed through the Guyon’s canal, an ana- tomical tunnel that is occupied by the ulnar nerve and artery. This type of anatomic variation is often associated with ulnar tunnel syndrome, in which the accessory belly is the source of a neurovascular compression causing pain, weakness of the muscles in the hand, and loss of motor and sensitive functions. Key words Anatomic variation, autopsy, cadaver, Guyon syndrome, ulnar nerve compression. Introduction The abductor digiti minimi muscle (ADMM) is one of the most variables muscles that form the hypothenar eminence and its usual origins are: the pisiform bone, the flexor carpi ulnaris tendon, and the pisohamate ligament. Its tendon usually divides into two (sometimes three) slips that insert onto the ulnar side of the fifth finger proximal phalanx, additionally, the muscle emits thin aponeurotic fibers to the meta- carpophalangeal joint of the fifth finger.