Biceps Tendon and Triceps Tendon Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Extended Insertion of Teres Minor Muscle: a Rare Case Report
Eur J Anat, 16 (3): 224-225 (2012) CASE REPORT Extended insertion of teres minor muscle: a rare case report Monica Jain, Lovesh Shukla, Dalbir Kaur Maharaja Agrasen Medical College, Agroha-125047, Hisar, Haryana, India SUMMARY upwards and laterally, and gets inserted on the lowest of the three impressions on the greater Teres minor is one of the muscles of the shoul- tubercle of the humerus and fuses with the der joint along with subscapularis, supraspina- capsule of the shoulder joint along with other tus and infraspinatus forming rotator cuff. muscles forming the rotator cuff. It is inner- Variations of teres minor are relatively uncom- vated by the posterior branch of the axillary mon. A unique and extended insertion of this nerve. It stabilizes the humerus by holding muscle is being reported in the present case. the humeral head in the glenoid cavity of the Knowledge of the anatomy of this muscle is scapula, a and causes lateral rotation of the important to avoid injury to the axillary nerve arm (Johnson, 2008). Variations of teres and posterior circumflex humeral vessels while minor are relatively uncommon and have been surgically approaching the shoulder joint and occasionally reported by various authors inserting portals of the arthroscope in a poste- (Bergman et al., 2006). rior approach to the shoulder joint. Key words: Teres minor – Rotator cuff – CASE REPORT Shoulder joint – Capsule of shoulder joint – Humerus – Surgical neck of humerus During routine dissection of the shoulder region of upper limb of an approximately 50 year-old male cadaver for undergraduate teach- INTRODUCTION ing and training, a unique and extended inser- tion of the teres minor muscle was found on the Teres minor is a one of the short scapular right side. -

Tricepsterrific
ACE-SPONSORED RESEARCH TricepsTerrific omen from all walks of life struggle to avoid the dreaded flabby, jiggly arms—and they often turn to personal trainers and fitness pros for help. “Guys always want to get rid of their bellies, while women always By Brittany Boehler,W B.S., seem to want to tone their triceps,” says John P. Porcari, Ph.D., John Porcari, Ph.D., an exercise physiologist Dennis Kline, M.S., with the University of Wisconsin and former C. Russell Hendrix, Ph.D., and personal trainer. Carl Foster, Ph.D., with Mark Anders But as with most clients, their time is constantly being gobbled up by work and family obligations, leaving little extra time for regular exercise. They want results—and fast! With that in mind, the This study was funded solely by the American Council on Exercise, the nation’s Work- American Council on Exercise (ACE). out Watchdog, sponsored comprehensive research to determine which exercises are most effec- tive—and efficient—for targeting the triceps. Armed with this new research, you’ll be able to better guide your clients in their efforts to tone and strengthen their triceps. TheTo determine Study the efficacy of the eight most common triceps exercises, ACE enlisted a team of exercise scientists from the University of Wiscon- sin/La Crosse Exercise and Health Program. Led www.acefitness.org pg. 1 ACE-SPONSORED RESEARCH by John Porcari, Ph.D., and Brittany Boehler, B.S., the exercise to ensure proper muscle recovery. Subjects lifted research team recruited 15 healthy female subjects, ages 70 percent of their previously determined 1 RM for the 20 to 24, from the local La Crosse community. -

Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies
Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies a, b Leo H. Wang, MD, PhD *, Michael D. Weiss, MD KEYWORDS Radial Posterior interosseous Neuropathy Electrodiagnostic study KEY POINTS The radial nerve subserves the extensor compartment of the arm. Radial nerve lesions are common because of the length and winding course of the nerve. The radial nerve is in direct contact with bone at the midpoint and distal third of the humerus, and therefore most vulnerable to compression or contusion from fractures. Electrodiagnostic studies are useful to localize and characterize the injury as axonal or demyelinating. Radial neuropathies at the midhumeral shaft tend to have good prognosis. INTRODUCTION The radial nerve is the principal nerve in the upper extremity that subserves the extensor compartments of the arm. It has a long and winding course rendering it vulnerable to injury. Radial neuropathies are commonly a consequence of acute trau- matic injury and only rarely caused by entrapment in the absence of such an injury. This article reviews the anatomy of the radial nerve, common sites of injury and their presentation, and the electrodiagnostic approach to localizing the lesion. ANATOMY OF THE RADIAL NERVE Course of the Radial Nerve The radial nerve subserves the extensors of the arms and fingers and the sensory nerves of the extensor surface of the arm.1–3 Because it serves the sensory and motor Disclosures: Dr Wang has no relevant disclosures. Dr Weiss is a consultant for CSL-Behring and a speaker for Grifols Inc. and Walgreens. He has research support from the Northeast ALS Consortium and ALS Therapy Alliance. -
Monday: Back, Biceps, Forearms, Traps & Abs Wednesday
THE TOOLS YOU NEED TO BUILD THE BODY YOU WANT® Store Workouts Diet Plans Expert Guides Videos Tools BULLDOZER TRAINING 3 DAY WORKOUT SPLIT 3 day Bulldozer Training muscle building split. Combines rest-pause sets with progressive Main Goal: Build Muscle Time Per Workout: 30-45 Mins resistance. Workouts are shorter but more Training Level: Intermediate Equipment: Barbell, Bodyweight, intense. Program Duration: 8 Weeks Dumbbells, EZ Bar, Machines Link to Workout: https://www.muscleandstrength.com/ Days Per Week: 3 Days Author: Steve Shaw workouts/bulldozer-training-3-day-workout-split Monday: Back, Biceps, Forearms, Traps & Abs Exercise Mini Sets Rep Goal Rest Deadlift: Perform as many rest-paused singles as you (safely) can within 10 Mins. Use a weight you could easily perform a 10 rep set with. Rest as needed. When you can perform 15 reps, add weight the next time you deadlift. Barbell Row 5 25 30 / 30 / 45 / 45 Wide Grip Pull Up 5 35 30 / 30 / 30 / 30 Standing Dumbbell Curl 4 25 30 / 30 / 30 EZ Bar Preacher Curl 4 25 30 / 30 / 30 Seated Barbell Wrist Curl 4 35 30 / 30 / 30 Barbell Shrug 5 35 30 / 30 / 30 / 30 Preferred Abs Exercise(s): I recommend using at least one weighted exercise (e.g. Weighted Sit Ups or Cable Crunches). Rest Periods: 30 / 30 / 45 / 45 notates rest periods between each set. Take 30 Secs after the 1st set, 30 Secs after the 2nd set, 45 Secs after the 3rd set, etc. After the final set, rest, and move on to the next exercise. -

M1 – Muscled Arm
M1 – Muscled Arm See diagram on next page 1. tendinous junction 38. brachial artery 2. dorsal interosseous muscles of hand 39. humerus 3. radial nerve 40. lateral epicondyle of humerus 4. radial artery 41. tendon of flexor carpi radialis muscle 5. extensor retinaculum 42. median nerve 6. abductor pollicis brevis muscle 43. flexor retinaculum 7. extensor carpi radialis brevis muscle 44. tendon of palmaris longus muscle 8. extensor carpi radialis longus muscle 45. common palmar digital nerves of 9. brachioradialis muscle median nerve 10. brachialis muscle 46. flexor pollicis brevis muscle 11. deltoid muscle 47. adductor pollicis muscle 12. supraspinatus muscle 48. lumbrical muscles of hand 13. scapular spine 49. tendon of flexor digitorium 14. trapezius muscle superficialis muscle 15. infraspinatus muscle 50. superficial transverse metacarpal 16. latissimus dorsi muscle ligament 17. teres major muscle 51. common palmar digital arteries 18. teres minor muscle 52. digital synovial sheath 19. triangular space 53. tendon of flexor digitorum profundus 20. long head of triceps brachii muscle muscle 21. lateral head of triceps brachii muscle 54. annular part of fibrous tendon 22. tendon of triceps brachii muscle sheaths 23. ulnar nerve 55. proper palmar digital nerves of ulnar 24. anconeus muscle nerve 25. medial epicondyle of humerus 56. cruciform part of fibrous tendon 26. olecranon process of ulna sheaths 27. flexor carpi ulnaris muscle 57. superficial palmar arch 28. extensor digitorum muscle of hand 58. abductor digiti minimi muscle of hand 29. extensor carpi ulnaris muscle 59. opponens digiti minimi muscle of 30. tendon of extensor digitorium muscle hand of hand 60. superficial branch of ulnar nerve 31. -

Triceps Exercises.Pdf
Ultimate Personal Training Triceps Exercise Guide Major Muscles That Act On the Elbow and Forearm MUSCLE ORIGIN INSERTION PRIMARY FUNCTIONS Brachialis Anterior humerous Ulnar tuberosity and Flexion at elbow coronoid process of ulna Triceps Long head from lower edge of glenoid cavity of Olecranon process of Extension at elbow brachii scapula; lateral head from posterior humerus; ulna short head from distal two-thirds of posterior humerus Pronator Distal end of medial humerus and medial aspect Middle third of lateral Flexion at elbow; teres of ulna radius pronation at forearm Triceps exercises.doc Page 1 of 21 Bench Tricep Dips Exercise Data Main Muscle Worked: Triceps Other Muscles Worked: Chest Equipment: BodyOnly Mechanics Type: Compound Tips: Place two flat benches parallel to each other, about three to four feet apart. Sit on one bench facing the other, with your hands grasping the side of the bench. Using your hands to support your weight, lift your feet to the top of the other bench so that the rest of your body is suspended between the two benches. Cross one foot over the other. Slowly lower your body toward the floor by bending your elbows until your upper arms and forearms form a right angle. Do not go below a 90-degree angle, as this can stress your shoulders. Slowly raise back up to the start position by straightening your arms. You can also place a weight plate on your upper legs for added resistance! Lying Cable Triceps Extension Exercise Data Main Muscle Worked: Triceps Other Muscles Worked: None Equipment: Cable Mechanics Type: Isolation Tips: Lie on a bench and grasp a short bar with a narrow overhand grip. -

Rotator Cuff 101 Every Year, More Than Two Million American Adults Seek Medical Care for Rotator Cuff Disease
BONE & JOINT BRIEFINGS Rotator Cuff 101 Every year, more than two million American adults seek medical care for rotator cuff disease. he rotator cuff is a series of 4 muscles It’s important to recognize that most people who surrounding the ball and socket joint of have shoulder pain don’t have a rotator cuff tear; the shoulder and plays a crucial role in there are many other causes. Pain from a rotator cuff optimizing shoulder function. The shoulder tear is usually experienced on the lateral aspect of the joint is inherently unstable, as the major arm, almost midway between the shoulder and the Tmuscles that move the shoulder around—the deltoid, elbow. It’s usually worse with overhead activity and the pectoralis, the back muscles—have a tendency worse at night. If this sort of pain is accompanied by to move the ball out of the center of the socket. The weakness, it probably should be checked right away. rotator cuff, almost as a counterforce against the If there’s no weakness involved, just aches and major muscles, helps to provide a stable fulcrum and pain, then ice, anti-inflammatory medication and a to optimize shoulder mechanics. couple of weeks of lighter activity could be all one As you might imagine, the muscles of the rotator needs. However, if the pain continues for more than a Christopher Gorczynski, MD cuff are subjected to quite a bit of stress. Friction couple of weeks, it deserves to be evaluated. Because and heavy usage (through sports or other repetitive the rotator cuff is under tension, tears generally get activity) can cause the tendons of the rotator cuff bigger over time and partial tears can become full- Those of us who are 30, to thicken or become inflamed and get “pinched” thickness tears. -

Section 1 Upper Limb Anatomy 1) with Regard to the Pectoral Girdle
Section 1 Upper Limb Anatomy 1) With regard to the pectoral girdle: a) contains three joints, the sternoclavicular, the acromioclavicular and the glenohumeral b) serratus anterior, the rhomboids and subclavius attach the scapula to the axial skeleton c) pectoralis major and deltoid are the only muscular attachments between the clavicle and the upper limb d) teres major provides attachment between the axial skeleton and the girdle 2) Choose the odd muscle out as regards insertion/origin: a) supraspinatus b) subscapularis c) biceps d) teres minor e) deltoid 3) Which muscle does not insert in or next to the intertubecular groove of the upper humerus? a) pectoralis major b) pectoralis minor c) latissimus dorsi d) teres major 4) Identify the incorrect pairing for testing muscles: a) latissimus dorsi – abduct to 60° and adduct against resistance b) trapezius – shrug shoulders against resistance c) rhomboids – place hands on hips and draw elbows back and scapulae together d) serratus anterior – push with arms outstretched against a wall 5) Identify the incorrect innervation: a) subclavius – own nerve from the brachial plexus b) serratus anterior – long thoracic nerve c) clavicular head of pectoralis major – medial pectoral nerve d) latissimus dorsi – dorsal scapular nerve e) trapezius – accessory nerve 6) Which muscle does not extend from the posterior surface of the scapula to the greater tubercle of the humerus? a) teres major b) infraspinatus c) supraspinatus d) teres minor 7) With regard to action, which muscle is the odd one out? a) teres -

Guidelines for Returning to Weightlifting Following Shoulder Surgery
Guidelines for Returning to Weightlifting Following Shoulder Surgery Before initiating any type of weight training, you must have full range of motion of the shoulder and normal strength of the rotator cuff and scapular muscle groups. Your motion and strength should be tested by COLUMBIA UNIVERSITY your surgeon before beginning any weightlifting regimen. CENTER FOR SHOULDER, ELBOW AND SPORTS The following illustrates the approximate time table for beginning MEDICINE weight training following your particular surgery: Rotator Cuff Repair: 6 months Christopher S. Ahmad, MD Bankart Repair: 3 months Office (212) 305-5561 Labrum Repair: 4-6 months Fax (212) 305-4040 Arthroscopic Subacromial Decompression: 4-6 months Louis U. Bigliani, MD When beginning a weight training program, you should start with low Office (212) 305-5564 weights and with 3 sets of 15-20 repetitions. The high repetition sets Fax (212) 305-0999 will ensure that the weights you are using are not too heavy. NEVER perform any weightlifting exercise to the point of muscle failure. Edwin Cadet, MD Muscle failure occurs when the muscle is no longer able to provide the Office (212) 305-4626 energy necessary to contract and move the joints involved in the Fax (212) 305-4040 particular exercise. When muscle failure occurs, the risk for joint, muscle and tendon injuries is greatly increased. William N. Levine, MD Office (212) 305-0762 Exercises to AVOID: Fax (212) 305-4040 1. Triceps Dips 2. Chest Flies Appointment Scheduling 3. Pull-downs behind the neck (212) 305-4565 4. Wide grip bench press 5. Triceps press overhead Mailing Address: th 6. -
Powerpoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint
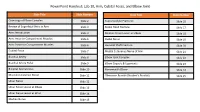
PowerPoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint Slide Title Slide Number Slide Title Slide Number Osteology of Elbow Complex Slide 2 Supracondylar Fractures Slide 16 Review of Superficial Veins in Arm Slide 3 Radial Head Fracture Slide 17 Arm: Introduction Slide 4 Median Nerve Lesion at Elbow Slide 18 Arm: Anterior Compartment Muscles Slide 5 Radial Nerve Slide 19 Arm: Posterior Compartment Muscles Slide 6 Humeral Shaft Fracture Slide 20 Cubital Fossa Slide 7 Medial Cutaneous Nerve of Arm Slide 21 Brachial Artery Slide 8 Elbow Joint Complex Slide 22 Brachial Artery Pulse Slide 9 Elbow Capsule & Ligaments Slide 23 Bicipital Aponeurosis Slide 10 Nursemaid’s Elbow Slide 24 Musculocutaneous Nerve Slide 11 Olecranon Bursitis (Student’s Bursitis) Slide 25 Ulnar Nerve Slide 12 Ulnar Nerve Lesion at Elbow Slide 13 Ulnar Nerve Lesion at Wrist Slide 14 Median Nerve Slide 15 Osteology of Elbow Complex To adequately review the learning objectives covering osteology of the distal humerus, radius, and ulna, view the Lower Limb Osteology and Medical Imaging Guide. Review of Superficial Veins in Arm The cephalic and basilic veins are the main superficial veins of the upper limb. They originate from the dorsal venous network on the dorsum of the hand. • The cephalic vein ascends along the anterolateral aspect of the forearm and arm. It then follows the superior border of the pectoralis major muscle to enter the deltopectoral triangle. It ultimately joins the axillary vein after passing through the clavipectoral fascia. • The basilic vein ascends along the medial forearm and the arm. In the arm, it passes deep to the brachial fascia where it courses in close proximity to the brachial artery and medial cutaneous nerve of the forearm along its path into the axilla. -

The Bicipital Aponeurosis
Surg Radiol Anat DOI 10.1007/s00276-017-1885-0 ORIGINAL ARTICLE Ultrasound visualization of an underestimated structure: the bicipital aponeurosis 1 1 1 M. Konschake • H. Stofferin • B. Moriggl Received: 15 February 2017 / Accepted: 31 May 2017 Ó The Author(s) 2017. This article is an open access publication Abstract the BA. Therefore, we suggest additional BA scanning during Purpose We established a detailed sonographic approach to clinical examinations of several pathologies, not only for BA the bicipital aponeurosis (BA), because different pathologies augmentation procedures in distal biceps tendon tears. of this, sometimes underestimated, structure are associated with vascular, neural and muscular lesions; emphasizing its Keywords Bicipital aponeurosis Á Lacertus fibrosus Á further implementation in routine clinical examinations. Biceps brachii muscle Á Ultrasonography Methods The BA of 100 volunteers, in sitting position with the elbow lying on a suitable table, was investigated. Patients were aged between 18 and 28 with no history of Introduction distal biceps injury. Examination was performed using an 18–6 MHz linear transducer (LA435; system MyLab25 by The biceps brachii muscle (BM) is attached distally to the Esaote, Genoa, Italy) utilizing the highest frequency, radial tuberosity via the strong biceps tendon (BT) and to scanned in two planes (longitudinal and transverse view). the antebrachial fascia via the bicipital aponeurosis (BA), In each proband, scanning was done with and without also known as lacertus fibrosus. As previously described, isometric contraction of the biceps brachii muscle. the BT consists of two distinct portions separated by an Results The BA was characterized by two clearly distin- endotenon septum and surrounded by a common paratenon, guishable white lines enveloping a hypoechoic band. -

Morphology of the Bicipital Aponeurosis: a Cadaveric Study S.D
Folia Morphol. Vol. 73, No. 1, pp. 79–83 DOI: 10.5603/FM.2014.0011 O R I G I N A L A R T I C L E Copyright © 2014 Via Medica ISSN 0015–5659 www.fm.viamedica.pl Morphology of the bicipital aponeurosis: a cadaveric study S.D. Joshi, A.S. Yogesh, P.S. Mittal, S.S. Joshi Department of Anatomy, Sri Aurobindo Medical College and Postgraduate Institute, Indore, India [Received 17 May 2013; Accepted 2 July 2013] The bicipital aponeurosis (BA) is a fascial expansion which arises from the ten- don of biceps brachii and dissipates some of the force away from its enthesis. It helps in dual action of biceps brachii as supinator and flexor of forearm. The aim of the present work was to study the morphology of BA. Thirty cadaveric upper limbs (16 right and 14 left side limbs) were dissected and dimensions of the BA were noted. The average width of aponeurosis at its commencement on the right was 15.74 mm while on the left it was 17.57 mm. The average angle between tendon and aponeurosis on the right was 21.16° and on the left it was 21.78°. The fibres from the short head of the biceps brachii contributed to the formation of proximal part of aponeurosis. Fascial sheath over the tendon of long head of biceps brachii was seen to form the distal part of the aponeurosis. In 5 cases, large fat globules were present between the sheath and the tendon. Histologically: The aponeurosis showed presence of thick collagen bundles.