Anatomy of the Hand Bones of the Hand
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identification and Surgical Management of Upper Arm and Forearm Compartment Syndrome
Open Access Case Report DOI: 10.7759/cureus.5862 Identification and Surgical Management of Upper Arm and Forearm Compartment Syndrome Adel Hanandeh 1 , Vishnu R. Mani 2 , Paul Bauer 1 , Alexius Ramcharan 3 , Brian Donaldson 1 1. General Surgery, Columbia University College of Physicians and Surgeons at Harlem Hospital Center, New York, USA 2. Surgery, Columbia University College of Physicians and Surgeons at Harlem Hospital Center, New York, USA 3. Surgery, Harlem Hospital Center, New York, USA Corresponding author: Adel Hanandeh, [email protected] Abstract Extremity muscles are grouped and divided by strong fascial membranes into compartments. Multiple pathological processes can result in an increase in the pressure within a muscle compartment. An increase in the compartment pressure beyond the adequate perfusion pressure has the potential to cause extremity compartment syndrome. There are multiple sites where compartment syndrome can occur. In this article, an arm and forearm compartment syndrome ensued secondary to a minor crushing injury that lead to supracondylar and medial epicondylar non-displaced fractures. A pure motor radial and ulnar nerve deficits noted on presentation, worsened with progression of the compartment syndrome. Ultimately, a surgical fasciotomy was carried out to release all compartments of the right upper arm and forearm. Categories: General Surgery, Orthopedics, Anatomy Keywords: upper arm compartment syndrome, fasciotomy, forearm compartment syndrome, condylar fracture, pediatric supracondylar humerus fracture Introduction In 1872, the first description of compartment syndrome was published by Richard von Volkmann. His publication described an irreversible contracture of muscles due to ischemic process resulting in the first documented nerve injury and contracture from compartment syndrome. -

Exposure of the Forearm and Distal Radius
Exposure of the Forearm and Distal Radius Melissa A. Klausmeyer, MDa, Chaitanya Mudgal, MDb,* KEYWORDS Henry approach Thompson approach Flexor carpi radialis approach Dorsal distal radius approach Distal radius approach KEY POINTS The use of internervous planes allow access to the underlying bone without risk of denervating the overlying muscles. The choice of approach is based on the injury pattern and need for exposure. The Henry and Thompson approaches are useful for radial shaft fractures. The distal radius can be approached volarly through the flexor carpi radialis (FCR) approach or dorsally through the extended Thompson approach. The extended FCR approach is useful for intraarticular fractures of the distal radius as well as mal- unions and subacute fractures. INTRODUCTION ANATOMY OF THE FOREARM Muscles Safe operative approaches to the bones of the forearm and wrist include the use of internervous The muscles of the forearm are split into 4 compart- planes. These planes lie between muscles that ments: The superficial volar, the deep volar, the are innervated by different nerves. By utilizing extensor, and the mobile wad (Table 1). The median these planes for dissection, extensive mobilization nerve supplies all of the volar muscles of the forearm of muscles and therefore large areas of exposure except the ulnar half of the flexor digitorum profun- may be obtained without the risk of muscle dus and the flexor carpi ulnaris that are supplied denervation. by the ulnar nerve. The radial nerve proper supplies A successful operative plan also must include the brachioradialis and extensor carpi radialis lon- consideration of the soft tissues, particularly gus. -

The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications
diagnostics Article The Branching and Innervation Pattern of the Radial Nerve in the Forearm: Clarifying the Literature and Understanding Variations and Their Clinical Implications F. Kip Sawyer 1,2,* , Joshua J. Stefanik 3 and Rebecca S. Lufler 1 1 Department of Medical Education, Tufts University School of Medicine, Boston, MA 02111, USA; rebecca.lufl[email protected] 2 Department of Anesthesiology, Stanford University School of Medicine, Stanford, CA 94305, USA 3 Department of Physical Therapy, Movement and Rehabilitation Science, Bouve College of Health Sciences, Northeastern University, Boston, MA 02115, USA; [email protected] * Correspondence: [email protected] Received: 20 May 2020; Accepted: 29 May 2020; Published: 2 June 2020 Abstract: Background: This study attempted to clarify the innervation pattern of the muscles of the distal arm and posterior forearm through cadaveric dissection. Methods: Thirty-five cadavers were dissected to expose the radial nerve in the forearm. Each muscular branch of the nerve was identified and their length and distance along the nerve were recorded. These values were used to determine the typical branching and motor entry orders. Results: The typical branching order was brachialis, brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis, supinator, extensor digitorum, extensor carpi ulnaris, abductor pollicis longus, extensor digiti minimi, extensor pollicis brevis, extensor pollicis longus and extensor indicis. Notably, the radial nerve often innervated brachialis (60%), and its superficial branch often innervated extensor carpi radialis brevis (25.7%). Conclusions: The radial nerve exhibits significant variability in the posterior forearm. However, there is enough consistency to identify an archetypal pattern and order of innervation. These findings may also need to be considered when planning surgical approaches to the distal arm, elbow and proximal forearm to prevent an undue loss of motor function. -
Neurology of the Upper Limb
Neurology of the Upper limb Donald Sammut Hand Surgeon Kings Upper Limb Anatomy plus lecture notes The$Neck$ The$Nerve$roots$which$supply$the$Upper$Limb$are$C5$to$T1$ Pre<fixed$(C4$to$C8)$and$Post<fixed$(C6$to$T2)$plexus$not$uncommon.$ Also$common$contributions$from$C4$and$from$T2$in$a$normally$rooted$plexus.$ $ The$anterior$nerve$roots$emerge$between$the$vertebrae$and$immediately$pass$ $through$the$first$area$of$possible$compression:$ The$root$nerve$canal$is$bounded$$ Anteriorly$by$the$posterior$margin$of$the$intervertebral$disc$and$$ Posteriorly,$by$the$facet$joint$between$vertebrae.$ $ Pathology$of$the$disc,$or$joint,$or$both,$can$narrow$this$channel$and$compress$ $the$nerve$root$ The$roots$emerge$from$the$cervical$spine$into$the$plane$between$$ Scalenius$Anterior$and$Scalenius$Medius.$$ $ Scalenius*Anterior:** Origin:$Anterior$tubercles$of$Cervical$vertebae$C3$to$6$(C6$tubercle$is$the$Carotid$tubercle)$ Insertion:$The$scalene$tubercle$on$inner$border/upper$surface$1st$rib$ $ Scalenius*Medius:* Origin:$Posterior$tubercles$of$all$cervical$vertebrae$ Insertion:$Quadrangular$area$between$the$neck$and$subclavian$groove$1st$rib$ $ Exiting$from$the$Scalenes,$the$trunks$lie$in$the$posterior$triangle$of$the$neck.$ The$posterior$triangle$is$bounded$anteriorly$by$SternoCleidoMastoid$and$$ posteriorly$by$the$Trapezius.$ The$inferior$border$is$the$clavicle$.$ The$apex$of$the$triangle$superiorly$is$at$the$back$of$the$skull$on$the$superior$nuchal$line$ $ $ The$Posterior$Triangle$ SternoCleidoMastoid$ Trapezius$ Scalenius$Medius$ Scalenius$Anterior$ -

Avulsion Fracture of Brachioradialis Muscle Origin: an Exceedingly Rare Entity: a Case Report
10-039_OA1 8/13/16 5:34 PM Page 50 Malaysian Orthopaedic Journal 2016 Vol 10 No 2 Behera G, et al http://dx.doi.org/10.5704/MOJ.1607.010 Avulsion Fracture of Brachioradialis Muscle Origin: An Exceedingly Rare Entity: A Case Report Behera G, DNB, Balaji G, MS Ortho, Menon J, MRCS (Edin.), Sharma D, MCH, Komuravalli VK, DNB Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India Date of submission: March 2016 Date of acceptance: June 2016 ABSTRACT lateral supracondylar ridge just proximal to the lateral epicondyle. He had restriction of active terminal elbow Avulsion fracture of the brachioradialis origin at its proximal extension by 10 degrees with near normal active elbow attachment on the lateral supracondylar ridge of the distal flexion, pronation and supination. Active flexion and humerus is exceedingly rare, and only two cases have been extension at wrist were painful along with the painful reported in the literature so far. In this article, we present a terminal elbow extension. There was significant pain at the 38 years old patient who sustained a closed avulsion fracture lateral distal humerus when active elbow flexion against of the lateral supracondylar ridge of left humerus at the resistance was performed in the mid-pronated position of the proximal attachment of brachioradialis following a fall forearm. There was no distal neurovascular deficit. backwards on outstretched hand after being struck by a lorry from behind while riding on a two-wheeler (motorcycle). He Antero-posterior (AP) plain radiograph of the left elbow was managed with above elbow plaster for four weeks showed a fracture of the lateral distal humerus at the followed by elbow and wrist mobilization. -

Section 1 Upper Limb Anatomy 1) with Regard to the Pectoral Girdle
Section 1 Upper Limb Anatomy 1) With regard to the pectoral girdle: a) contains three joints, the sternoclavicular, the acromioclavicular and the glenohumeral b) serratus anterior, the rhomboids and subclavius attach the scapula to the axial skeleton c) pectoralis major and deltoid are the only muscular attachments between the clavicle and the upper limb d) teres major provides attachment between the axial skeleton and the girdle 2) Choose the odd muscle out as regards insertion/origin: a) supraspinatus b) subscapularis c) biceps d) teres minor e) deltoid 3) Which muscle does not insert in or next to the intertubecular groove of the upper humerus? a) pectoralis major b) pectoralis minor c) latissimus dorsi d) teres major 4) Identify the incorrect pairing for testing muscles: a) latissimus dorsi – abduct to 60° and adduct against resistance b) trapezius – shrug shoulders against resistance c) rhomboids – place hands on hips and draw elbows back and scapulae together d) serratus anterior – push with arms outstretched against a wall 5) Identify the incorrect innervation: a) subclavius – own nerve from the brachial plexus b) serratus anterior – long thoracic nerve c) clavicular head of pectoralis major – medial pectoral nerve d) latissimus dorsi – dorsal scapular nerve e) trapezius – accessory nerve 6) Which muscle does not extend from the posterior surface of the scapula to the greater tubercle of the humerus? a) teres major b) infraspinatus c) supraspinatus d) teres minor 7) With regard to action, which muscle is the odd one out? a) teres -
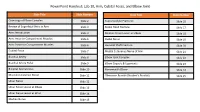
Powerpoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint
PowerPoint Handout: Lab 10, Arm, Cubital Fossa, and Elbow Joint Slide Title Slide Number Slide Title Slide Number Osteology of Elbow Complex Slide 2 Supracondylar Fractures Slide 16 Review of Superficial Veins in Arm Slide 3 Radial Head Fracture Slide 17 Arm: Introduction Slide 4 Median Nerve Lesion at Elbow Slide 18 Arm: Anterior Compartment Muscles Slide 5 Radial Nerve Slide 19 Arm: Posterior Compartment Muscles Slide 6 Humeral Shaft Fracture Slide 20 Cubital Fossa Slide 7 Medial Cutaneous Nerve of Arm Slide 21 Brachial Artery Slide 8 Elbow Joint Complex Slide 22 Brachial Artery Pulse Slide 9 Elbow Capsule & Ligaments Slide 23 Bicipital Aponeurosis Slide 10 Nursemaid’s Elbow Slide 24 Musculocutaneous Nerve Slide 11 Olecranon Bursitis (Student’s Bursitis) Slide 25 Ulnar Nerve Slide 12 Ulnar Nerve Lesion at Elbow Slide 13 Ulnar Nerve Lesion at Wrist Slide 14 Median Nerve Slide 15 Osteology of Elbow Complex To adequately review the learning objectives covering osteology of the distal humerus, radius, and ulna, view the Lower Limb Osteology and Medical Imaging Guide. Review of Superficial Veins in Arm The cephalic and basilic veins are the main superficial veins of the upper limb. They originate from the dorsal venous network on the dorsum of the hand. • The cephalic vein ascends along the anterolateral aspect of the forearm and arm. It then follows the superior border of the pectoralis major muscle to enter the deltopectoral triangle. It ultimately joins the axillary vein after passing through the clavipectoral fascia. • The basilic vein ascends along the medial forearm and the arm. In the arm, it passes deep to the brachial fascia where it courses in close proximity to the brachial artery and medial cutaneous nerve of the forearm along its path into the axilla. -

The Bicipital Aponeurosis
Surg Radiol Anat DOI 10.1007/s00276-017-1885-0 ORIGINAL ARTICLE Ultrasound visualization of an underestimated structure: the bicipital aponeurosis 1 1 1 M. Konschake • H. Stofferin • B. Moriggl Received: 15 February 2017 / Accepted: 31 May 2017 Ó The Author(s) 2017. This article is an open access publication Abstract the BA. Therefore, we suggest additional BA scanning during Purpose We established a detailed sonographic approach to clinical examinations of several pathologies, not only for BA the bicipital aponeurosis (BA), because different pathologies augmentation procedures in distal biceps tendon tears. of this, sometimes underestimated, structure are associated with vascular, neural and muscular lesions; emphasizing its Keywords Bicipital aponeurosis Á Lacertus fibrosus Á further implementation in routine clinical examinations. Biceps brachii muscle Á Ultrasonography Methods The BA of 100 volunteers, in sitting position with the elbow lying on a suitable table, was investigated. Patients were aged between 18 and 28 with no history of Introduction distal biceps injury. Examination was performed using an 18–6 MHz linear transducer (LA435; system MyLab25 by The biceps brachii muscle (BM) is attached distally to the Esaote, Genoa, Italy) utilizing the highest frequency, radial tuberosity via the strong biceps tendon (BT) and to scanned in two planes (longitudinal and transverse view). the antebrachial fascia via the bicipital aponeurosis (BA), In each proband, scanning was done with and without also known as lacertus fibrosus. As previously described, isometric contraction of the biceps brachii muscle. the BT consists of two distinct portions separated by an Results The BA was characterized by two clearly distin- endotenon septum and surrounded by a common paratenon, guishable white lines enveloping a hypoechoic band. -
Upper Extremity Compression Neuropathies
Peripheral Nerve Injury in the Athlete: Upper and Lower Limb Entrapment Neuropathies Greg Moore, MD Sports and Spine Rehabilitation NeuroSpine Institute Outline Review common nerve entrapment and injury syndromes, particularly related to sports Review pertinent anatomy to each nerve Review typical symptoms Discuss pathophysiology Discuss pertinent diagnostic tests and treatment options Neuropathy Mononeuropathies Median Femoral Pronator Teres Intrapelvic Anterior Interosseous Nerve Inguinal Ligament Carpal Tunnel Sciatic Ulnar Piriformis Cubital Tunnel Peroneal Guyon’s Canal Fibular Head Radial Axilla Tibial Spiral Groove Tarsal Tunnel Posterior Interosseous Nerve Sports Medicine Pearls Utilize your athletic trainers Individualize your diagnostic and treatment approach based on multiple factors Age Sport Level of Sport (HS, college, professional) Position Sports Medicine Pearls Time in the season Degree of pain/disability Desire of the patient/parents Coach’s desires/level of concern Cost (rarely discuss with the coach) Danger of a delay in diagnosis Impact to the team Obtaining the History Pain questions- location, duration, type, etc. Presence and location of numbness and paresthesias Exertional fatigue and/or weakness Subjective muscle atrophy Symptom onset- insidious or post-traumatic Exacerbating activities History (continued) Changes in exercise duration, intensity or frequency New techniques or equipment Past medical history and review of systems Diabetes Hypercoaguable state Depression/anxiety -

Morphology of the Bicipital Aponeurosis: a Cadaveric Study S.D
Folia Morphol. Vol. 73, No. 1, pp. 79–83 DOI: 10.5603/FM.2014.0011 O R I G I N A L A R T I C L E Copyright © 2014 Via Medica ISSN 0015–5659 www.fm.viamedica.pl Morphology of the bicipital aponeurosis: a cadaveric study S.D. Joshi, A.S. Yogesh, P.S. Mittal, S.S. Joshi Department of Anatomy, Sri Aurobindo Medical College and Postgraduate Institute, Indore, India [Received 17 May 2013; Accepted 2 July 2013] The bicipital aponeurosis (BA) is a fascial expansion which arises from the ten- don of biceps brachii and dissipates some of the force away from its enthesis. It helps in dual action of biceps brachii as supinator and flexor of forearm. The aim of the present work was to study the morphology of BA. Thirty cadaveric upper limbs (16 right and 14 left side limbs) were dissected and dimensions of the BA were noted. The average width of aponeurosis at its commencement on the right was 15.74 mm while on the left it was 17.57 mm. The average angle between tendon and aponeurosis on the right was 21.16° and on the left it was 21.78°. The fibres from the short head of the biceps brachii contributed to the formation of proximal part of aponeurosis. Fascial sheath over the tendon of long head of biceps brachii was seen to form the distal part of the aponeurosis. In 5 cases, large fat globules were present between the sheath and the tendon. Histologically: The aponeurosis showed presence of thick collagen bundles. -

Bilateral Reversed Palmaris Longus Muscle: a Rare Anatomical Variation
Folia Morphol. Vol. 71, No. 1, pp. 52–55 Copyright © 2012 Via Medica C A S E R E P O R T ISSN 0015–5659 www.fm.viamedica.pl Bilateral reversed palmaris longus muscle: a rare anatomical variation G. Salgado1, M. Cantín2, O. Inzunza1, A. Muñoz1, J. Saez1, M. Macuer1 1Department of Normal Anatomy, Pontificia Universidad Católica de Chile, Faculty of Medicine, Santiago, Chile 2Department of Integral Odontology, Doctoral Program in Morphological Sciences, Faculty of Odontology, Faculty of Medicine, Universidad de La Frontera, Temuco, Chile [Received 8 September 2011; Accepted 23 October 2011] We report a case of bilateral reversed palmaris longus muscle (PLM). The mus- cle was tendinous in its upper portion and muscular in its lower portion in both arms. This rare variation has been mentioned only once in the literature as a surgical finding. According to the literature, a reversed PLM may cause a com- partment syndrome in the wrist area, carpal tunnel, and Guyon’s syndrome. The described variation is also useful to the hand surgeon as a tendon graft, a tendon for transfer, or as an anatomical landmark for operations at this area. (Folia Morphol 2012; 71, 1: 52–55) Key words: palmaris longus muscle, reversed muscle, anatomical variation, forearm INTRODUCTION The PLM is extremely variable. Its most frequent The palmaris longus muscle (PLM) is a fusiform variation is agenesis, reported in 12.8% of the po- and thin muscle that lies medial to the flexor carpi pulation [10, 15]. Other variations include differenc- radialis (FCR) muscle. It shares a common origin with es in shape and position described as central, in- the flexor superficialis digitorum (FSD) muscle, the verted, bifid, duplicated [11], and even triplicated flexor carpi ulnaris (FCU) muscle, and the FCR, in the [7, 15]. -

Additional Muscle Slips from the Bicipital Aponeurosis and a Long Communicating Branch Between the Musculocutaneous and the Median Nerves
eISSN 1308-4038 International Journal of Anatomical Variations (2012) 5: 41–43 Case Report Additional muscle slips from the bicipital aponeurosis and a long communicating branch between the musculocutaneous and the median nerves Published online October 12th, 2012 © http://www.ijav.org Kumar MR BHAT Abstract Vinay KULAKARNI Additional muscle slips from the bicipital aponeurosis both to pronator teres and flexor carpi radialis muscles are uncommon and not been reported. Here, we report a case of presence of Chandni GUPTA tendentious slip arising from the under surface of the bicipital aponeurosis in the cubital fossa in the left upper limb of a 72-year-old male cadaver. This tendineous slip was then divided into two separate muscular heads for the pronator teres and flexor carpi radialis muscles. Department of Anatomy, Kasturba Medical College, Additionally, in the same cadaver we also found an unusual long communicating branch from the Manipal University, Manipal, INDIA. musculocutaneous nerve in the upper arm, which had long course through the arm before joining the median nerve in the cubital fossa. This report discusses the details of these variations, their clinical implication and embryological explanations. Dr. Kumar MR Bhat © Int J Anat Var (IJAV). 2012; 5: 41–43. Associate Professor Department of Anatomy Kasturba Medical College Manipal University Manipal, 576104, INDIA. +91 (820) 2922327 [email protected] Received April 15th, 2011; accepted January 17th, 2012 Key words [pronator teres] [flexor carpi radialis] [musculocutaneous nerve] [communicating branch] [additional head] Introduction of pronator teres and flexor carpi radialis (2.08%). This Pronator teres usually originates as two heads, the superficial additional muscle was originated as tendineous slip from humeral head from medial epicondyle and the deep ulnar head the undersurface of the aponeurotic extension of the biceps from the coronoid process.