And Report of a New Strain, Keystone Virus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mosquito Species Identification Using Convolutional Neural Networks With
www.nature.com/scientificreports OPEN Mosquito species identifcation using convolutional neural networks with a multitiered ensemble model for novel species detection Adam Goodwin1,2*, Sanket Padmanabhan1,2, Sanchit Hira2,3, Margaret Glancey1,2, Monet Slinowsky2, Rakhil Immidisetti2,3, Laura Scavo2, Jewell Brey2, Bala Murali Manoghar Sai Sudhakar1, Tristan Ford1,2, Collyn Heier2, Yvonne‑Marie Linton4,5,6, David B. Pecor4,5,6, Laura Caicedo‑Quiroga4,5,6 & Soumyadipta Acharya2* With over 3500 mosquito species described, accurate species identifcation of the few implicated in disease transmission is critical to mosquito borne disease mitigation. Yet this task is hindered by limited global taxonomic expertise and specimen damage consistent across common capture methods. Convolutional neural networks (CNNs) are promising with limited sets of species, but image database requirements restrict practical implementation. Using an image database of 2696 specimens from 67 mosquito species, we address the practical open‑set problem with a detection algorithm for novel species. Closed‑set classifcation of 16 known species achieved 97.04 ± 0.87% accuracy independently, and 89.07 ± 5.58% when cascaded with novelty detection. Closed‑set classifcation of 39 species produces a macro F1‑score of 86.07 ± 1.81%. This demonstrates an accurate, scalable, and practical computer vision solution to identify wild‑caught mosquitoes for implementation in biosurveillance and targeted vector control programs, without the need for extensive image database development for each new target region. Mosquitoes are one of the deadliest animals in the world, infecting between 250–500 million people every year with a wide range of fatal or debilitating diseases, including malaria, dengue, chikungunya, Zika and West Nile Virus1. -

Pesticide Discharge Management Plan
Pesticide Discharge Management Plan 1. PDMP Team a. Person(s) responsible for managing pests in relation to pest management area: All operational and biological support staff along with the Director of Mosquito Management Services (Wade Brennan, 5531 Pinkney Ave. Sarasota, FL. 34233) b. Person(s) responsible for developing and revising PDMP John Eaton, Operations Supervisor, and Wade Brennan Environmental Scientist III, are the individuals responsible for monitoring changes in Federal and State regulatory agencies that govern mosquito control operations. c. John Eaton, and Wade Brennan, are the individuals responsible for developing, revising and implementing corrective actions and other effluent requirements d. Person(s) responsible for pesticide applications Persons (supervisors and above) who direct applicators these include: All Operational staff employed by Sarasota County Mosquito Management Services that hold a Public Health Pest Control License administered by Florida Department of Agriculture and Consumer Services are directly responsible for pesticide applications (because they can oversee uncertified applicators) additionally, Sarasota County’s awarded Contractors must have required state certification (s). 2. Pest Management Area Description Overview Sarasota County Mosquito Management Services (SCMMS) has been mitigating pestiferous nuisance host seeking mosquitoes of public health importance for over 60 years. A total of forty- four mosquito species are found in Sarasota County of which a dozen are in need of management through a typical peak mosquito season, April through November. When intervention action plans are developed and implemented more than one species is usually involved. Past and current mitigation strategies for both larval and adult mosquitoes have always been in full compliance with FIFRA conditions which have met water quality standards. -

MOSQUITOES of the SOUTHEASTERN UNITED STATES
L f ^-l R A R > ^l^ ■'■mx^ • DEC2 2 59SO , A Handbook of tnV MOSQUITOES of the SOUTHEASTERN UNITED STATES W. V. King G. H. Bradley Carroll N. Smith and W. C. MeDuffle Agriculture Handbook No. 173 Agricultural Research Service UNITED STATES DEPARTMENT OF AGRICULTURE \ I PRECAUTIONS WITH INSECTICIDES All insecticides are potentially hazardous to fish or other aqpiatic organisms, wildlife, domestic ani- mals, and man. The dosages needed for mosquito control are generally lower than for most other insect control, but caution should be exercised in their application. Do not apply amounts in excess of the dosage recommended for each specific use. In applying even small amounts of oil-insecticide sprays to water, consider that wind and wave action may shift the film with consequent damage to aquatic life at another location. Heavy applications of insec- ticides to ground areas such as in pretreatment situa- tions, may cause harm to fish and wildlife in streams, ponds, and lakes during runoff due to heavy rains. Avoid contamination of pastures and livestock with insecticides in order to prevent residues in meat and milk. Operators should avoid repeated or prolonged contact of insecticides with the skin. Insecticide con- centrates may be particularly hazardous. Wash off any insecticide spilled on the skin using soap and water. If any is spilled on clothing, change imme- diately. Store insecticides in a safe place out of reach of children or animals. Dispose of empty insecticide containers. Always read and observe instructions and precautions given on the label of the product. UNITED STATES DEPARTMENT OF AGRICULTURE Agriculture Handbook No. -

Taxonomy of the Order Bunyavirales: Update 2019
Archives of Virology (2019) 164:1949–1965 https://doi.org/10.1007/s00705-019-04253-6 VIROLOGY DIVISION NEWS Taxonomy of the order Bunyavirales: update 2019 Abulikemu Abudurexiti1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Tatjana Avšič‑Županc5 · Matthew J. Ballinger6 · Dennis A. Bente7 · Martin Beer8 · Éric Bergeron9 · Carol D. Blair10 · Thomas Briese11 · Michael J. Buchmeier12 · Felicity J. Burt13 · Charles H. Calisher10 · Chénchén Cháng14 · Rémi N. Charrel15 · Il Ryong Choi16 · J. Christopher S. Clegg17 · Juan Carlos de la Torre18 · Xavier de Lamballerie15 · Fēi Dèng19 · Francesco Di Serio20 · Michele Digiaro21 · Michael A. Drebot22 · Xiaˇoméi Duàn14 · Hideki Ebihara23 · Toufc Elbeaino21 · Koray Ergünay24 · Charles F. Fulhorst7 · Aura R. Garrison25 · George Fú Gāo26 · Jean‑Paul J. Gonzalez27 · Martin H. Groschup28 · Stephan Günther29 · Anne‑Lise Haenni30 · Roy A. Hall31 · Jussi Hepojoki32,33 · Roger Hewson34 · Zhìhóng Hú19 · Holly R. Hughes35 · Miranda Gilda Jonson36 · Sandra Junglen37,38 · Boris Klempa39 · Jonas Klingström40 · Chūn Kòu14 · Lies Laenen41,42 · Amy J. Lambert35 · Stanley A. Langevin43 · Dan Liu44 · Igor S. Lukashevich45 · Tāo Luò1 · Chuánwèi Lüˇ 19 · Piet Maes41 · William Marciel de Souza46 · Marco Marklewitz37,38 · Giovanni P. Martelli47 · Keita Matsuno48,49 · Nicole Mielke‑Ehret50 · Maria Minutolo3 · Ali Mirazimi51 · Abulimiti Moming14 · Hans‑Peter Mühlbach50 · Rayapati Naidu52 · Beatriz Navarro20 · Márcio Roberto Teixeira Nunes53 · Gustavo Palacios25 · Anna Papa54 · Alex Pauvolid‑Corrêa55 · Janusz T. Pawęska56,57 · Jié Qiáo19 · Sheli R. Radoshitzky25 · Renato O. Resende58 · Víctor Romanowski59 · Amadou Alpha Sall60 · Maria S. Salvato61 · Takahide Sasaya62 · Shū Shěn19 · Xiǎohóng Shí63 · Yukio Shirako64 · Peter Simmonds65 · Manuela Sironi66 · Jin‑Won Song67 · Jessica R. Spengler9 · Mark D. Stenglein68 · Zhèngyuán Sū19 · Sùróng Sūn14 · Shuāng Táng19 · Massimo Turina69 · Bó Wáng19 · Chéng Wáng1 · Huálín Wáng19 · Jūn Wáng19 · Tàiyún Wèi70 · Anna E. -

Notification Requirements
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2021 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of within the next reporting cycle. a case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 Approved by CSTE: June 2019 within 24 hours of a case meeting the notification criteria, followed by Interim Update Approved by CSTE: April 5, 2020 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2020 electronic transmission. Updated: May 28, 2020 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Page 1 of 5 Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis -

Testing Effects of Aerial Spray Technologies on Biting Flies
TESTING EFFECTS OF AERIAL SPRAY TECHNOLOGIES ON BITING FLIES AND NONTARGET INSECTS AT THE PARRIS ISLAND MARINE CORPS RECRUIT DEPOT, SOUTH CAROLINA, USA. A dissertation submitted to Kent State University in partial fulfillment of the requirements for the degree of Doctor of Philosophy by Mark S. Breidenbaugh December 2008 Dissertation written by Mark S. Breidenbaugh B.S., California State Polytechnic University, Pomona 1994 M.S., University of California, Riverside, 1997 Ph.D., Kent State University, 2008 Approved by _____________________________, Chair, Doctoral Dissertation Committee Ferenc A. de Szalay _____________________________, Members, Doctoral Dissertation Committee Benjamin A. Foote _____________________________ Mark W. Kershner _____________________________ Scott C. Sheridan Accepted by ______________________________, Chair, Department of Biological Sciences James L. Blank ______________________________, Dean, College of Arts and Sciences John R.D. Stalvey ii TABLE OF CONTENTS Page LIST OF FIGURES……………………………………………………………………viii LIST OF TABLES………………………………………………………………………xii ACKNOWLEDGEMENTS………………….…………………………………………xiv CHAPTER I. An introduction to the biting flies of Parris Island and the use of aerial spray technologies in their control……………………………………………..1 Biology of biting midges .....……..……………………………………………..1 Culicoides as nuisance pests and vectors……………………………3 Biology of mosquitoes…………………………………………………………..5 Mosquitoes as nuisance pests and vectors…………………………..6 Integrated pest management…………………………………………………..7 Physical barriers…………………………………………………………8 -

2018 DSHS Arbovirus Activity
Health and Human Texas Department of State Services Health Services Arbovirus Activity in Texas 2018 Surveillance Report August 2019 Texas Department of State Health Services Zoonosis Control Branch Overview Viruses transmitted by mosquitoes are referred to as arthropod-borne viruses or arboviruses. Arboviruses reported in Texas may include California (CAL) serogroup viruses, chikungunya virus (CHIKV), dengue virus (DENV), eastern equine encephalitis virus (EEEV), Saint Louis encephalitis virus (SLEV), western equine encephalitis virus (WEEV), West Nile virus (WNV), and Zika virus (ZIKV), many of which are endemic or enzootic in the state. In 2018, reported human arboviral disease cases were attributed to WNV (82%), DENV (11%), CHIKV (4%), ZIKV (2%), and CAL (1%) (Table 1). In addition, there were two cases reported as arbovirus disease cases which could not be diagnostically or epidemiologically differentiated between DENV and ZIKV. Animal infections or disease caused by WNV and SLEV were also reported during 2018. Local transmission of DENV, SLEV, and WNV was documented during 2018 (Figure 1). No reports of EEEV or WEEV were received during 2018. Table 1. Year-End Arbovirus Activity Summary, Texas, 2018 Positive Human* Arbovirus Mosquito Avian Equine TOTAL TOTAL Fever Neuroinvasive Severe Deaths PVD‡ Pools (Human) CAL 1 1 1 CHIK 7 7 7 DEN 20 20 20 SLE 2 0 2 WN 1,021 6 19 38 108 146 11 24 1,192 Zika** 4 4 TOTAL 1,023 6 19 65 109 0 178 11 24 1,226 CAL - California serogroup includes California encephalitis, Jamestown Canyon, Keystone, La Crosse, Snowshoe hare and Trivittatus viruses CHIK - Chikungunya DEN - Dengue SLE - Saint Louis encephalitis WN - West Nile ‡PVD - Presumptive viremic blood donors are people who had no symptoms at the time of donating blood through a blood collection agency, but whose blood tested positive when screened for the presence of West Nile virus or Zika virus. -
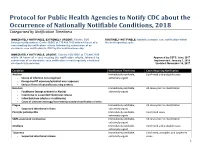
Protocol for Public Health Agencies to Notify CDC About the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification within Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of a the next reporting cycle. case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 within 24 hours of a case meeting the notification criteria, followed by Approved by CSTE: June 2017 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2018 electronic transmission. Updated: November 16, 2017 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis Immediately notifiable, Confirmed cases extremely -

Taxonomy of the Family Arenaviridae and the Order Bunyavirales: Update 2018
Archives of Virology https://doi.org/10.1007/s00705-018-3843-5 VIROLOGY DIVISION NEWS Taxonomy of the family Arenaviridae and the order Bunyavirales: update 2018 Piet Maes1 · Sergey V. Alkhovsky2 · Yīmíng Bào3 · Martin Beer4 · Monica Birkhead5 · Thomas Briese6 · Michael J. Buchmeier7 · Charles H. Calisher8 · Rémi N. Charrel9 · Il Ryong Choi10 · Christopher S. Clegg11 · Juan Carlos de la Torre12 · Eric Delwart13,14 · Joseph L. DeRisi15 · Patrick L. Di Bello16 · Francesco Di Serio17 · Michele Digiaro18 · Valerian V. Dolja19 · Christian Drosten20,21,22 · Tobiasz Z. Druciarek16 · Jiang Du23 · Hideki Ebihara24 · Toufc Elbeaino18 · Rose C. Gergerich16 · Amethyst N. Gillis25 · Jean‑Paul J. Gonzalez26 · Anne‑Lise Haenni27 · Jussi Hepojoki28,29 · Udo Hetzel29,30 · Thiện Hồ16 · Ní Hóng31 · Rakesh K. Jain32 · Petrus Jansen van Vuren5,33 · Qi Jin34,35 · Miranda Gilda Jonson36 · Sandra Junglen20,22 · Karen E. Keller37 · Alan Kemp5 · Anja Kipar29,30 · Nikola O. Kondov13 · Eugene V. Koonin38 · Richard Kormelink39 · Yegor Korzyukov28 · Mart Krupovic40 · Amy J. Lambert41 · Alma G. Laney42 · Matthew LeBreton43 · Igor S. Lukashevich44 · Marco Marklewitz20,22 · Wanda Markotter5,33 · Giovanni P. Martelli45 · Robert R. Martin37 · Nicole Mielke‑Ehret46 · Hans‑Peter Mühlbach46 · Beatriz Navarro17 · Terry Fei Fan Ng14 · Márcio Roberto Teixeira Nunes47,48 · Gustavo Palacios49 · Janusz T. Pawęska5,33 · Clarence J. Peters50 · Alexander Plyusnin28 · Sheli R. Radoshitzky49 · Víctor Romanowski51 · Pertteli Salmenperä28,52 · Maria S. Salvato53 · Hélène Sanfaçon54 · Takahide Sasaya55 · Connie Schmaljohn49 · Bradley S. Schneider25 · Yukio Shirako56 · Stuart Siddell57 · Tarja A. Sironen28 · Mark D. Stenglein58 · Nadia Storm5 · Harikishan Sudini59 · Robert B. Tesh48 · Ioannis E. Tzanetakis16 · Mangala Uppala59 · Olli Vapalahti28,30,60 · Nikos Vasilakis48 · Peter J. Walker61 · Guópíng Wáng31 · Lìpíng Wáng31 · Yànxiăng Wáng31 · Tàiyún Wèi62 · Michael R. -

Mosquitoes and the Diseases They Transmit J
B-6119 6-02 Mosquitoes and the Diseases they Transmit J. A. Jackman and J. K. Olson* osquitoes are among the most important The length of time that a mosquito takes to complete insect pests affecting the health of people its life cycle varies according to food availability, weath- er conditions and the species of mosquito. Under favor- and animals. Biting female mosquitoes not M able conditions, some mosquitoes can complete their only irritate people and animals, but they can also entire life cycle in only 8 to 10 days. transmit many disease-causing organisms. Egg Annoying populations of mosquitoes can occur any- where in Texas because there are habitats favorable for One way to identify mosquito species almost everywhere in the state. the breeding sites of mosquitoes is to find the To control mosquitoes effectively, it helps to under- eggs. Mosquito eggs may stand their life cycle, to be able to identify the various be laid in clusters called kinds of mosquitoes, and to know what steps work best rafts on the water sur- for the different species and specific locations. face. They may also be laid singly on the water Life history surface or in dry areas Adult mosquito laying eggs. Mosquitoes have four distinct stages during their life that are flooded periodi- cycle: egg, larva, pupa and adult. The adult stage is free- cally. flying; the other stages are aquatic. When first laid, mosquito eggs are white, but within a few hours they become dark brown to black. The shape and size of mosquito eggs vary, with most being football- shaped or boat-shaped and 0.02 to 0.04 inch long. -

DSHS Arbovirus Activity 061817
Arbovirus Activity in Texas 2017 Surveillance Report June 2018 Texas Department of State Health Services Infectious Disease Control Unit Zoonosis Control Branch Overview Viruses transmitted by mosquitoes are referred to as arthropod-borne viruses or arboviruses. Arboviruses reported in Texas may include California serogroup viruses (CAL), chikungunya virus (CHIKV), dengue virus (DENV), eastern equine encephalitis virus (EEEV), Saint Louis encephalitis virus (SLEV), western equine encephalitis virus (WEEV), West Nile virus (WNV), and Zika virus (ZIKV), many of which are endemic or enzootic in the state. In 2017, reported human arboviral disease cases were attributed to WNV (54%), ZIKV (22%), DENV (17%), and CHIKV (6%) (Table 1). Animal infections or disease caused by CAL, EEEV, SLEV, and WNV were also reported during 2017. Table 1. Year-End Arbovirus Activity Summary, Texas, 2017 California Serogroup Viruses California serogroup viruses (CAL) are bunyaviruses and include California encephalitis virus (CEV), Jamestown Canyon virus, Keystone virus, La Crosse virus (LACV), snowshoe hare virus, and Trivittatus virus. These viruses are maintained in a cycle between mosquito vectors and vertebrate hosts in forest habitats. In the United States (U.S.), approximately 80-100 reported cases of human neuroinvasive disease are caused by LACV each year (CDC), mostly in mid-Atlantic and southeastern states. From 2002-2016, Texas reported a total of 5 cases of human CAL disease (range: 0-3 cases/year): 1 case of CEV neuroinvasive disease and 4 cases of LACV neuroinvasive disease. In 2017, one CEV-positive mosquito pool was identified in Orange County (Figure 1); no human cases of CAL disease were reported. -

The History of Public Entomology at the Connecticut Agricultural
The Connecticut Agricultural Experiment Station The History of Public Health Entomology at The Connecticut Agricultural Experiment Station 1904 –2009 JOHN F. ANDERSON, Ph.D. Distinguished Scientist Emeritus, Department of Entomology The Connecticut Agricultural Experiment Station The History of Public Health Entomology at The Connecticut Agricultural Experiment Station 1904 –2009 JOHN F. ANDERSON, Ph.D. Distinguished Scientist Emeritus, Department of Entomology Funded, in part, by The Experiment Station Associates Bulletin 1030 2010 Acknowledgments This publication is in response to citizen requests that I write an Experiment Station publication of my talk entitled, “104 Years of Public Health Entomology at The Connecticut Agricultural Experiment Station.” I gave this presentation in New Haven at an open house event in the spring of 2008. I express my sincere appreciation to Bonnie Hamid, who formatted the complex figures and the entire text and provided assistance with library searches and the writing. Vickie Bomba-Lewandoski assisted with acquiring some of the historical publications and scanning some of the photographs. Dr. Toby Anita Appel, John R. Bumstead Librarian for Medical History, and Florence Gillich, Historical Medical Library Assistant at the Harvey Cushing/John Hay Whitney Medical Library, Yale University, assisted me with locating critical publications, as did Suzy Taraba, University Archivist and Head of Special Collections at Olin Library, Wesleyan University, and Professor Durland Fish, Yale University. James W. Campbell, Librarian and Curator of Manuscripts at the New Haven Museum sent me a copy of the New Haven Chronicle masthead (Figure 7). The extraordinary efforts of Mr. David Miles, photographer, Mr. Andrew Rogalski, Technical Services Librarian, and Terrie Wheeler, Chief Librarian, Gorgas Memorial Library, Walter Reed Army Institute of Research, in providing the superb image of Dean Cornwell’s painting entitled “Conquerors of Yellow Fever” (Figure 12) are greatly appreciated.