2018 DSHS Arbovirus Activity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Arboviral Infection Surveillance Protocol
April 2013 Arboviral Infection Surveillance Protocol Arboviruses endemic to the U.S. include Eastern equine encephalitis virus (EEE), La Crosse encephalitis virus (LAC), Saint Louis encephalitis virus (SLE), West Nile virus (WNV), Western equine encephalitis virus (WEE), and the tickborne Powassan encephalitis virus (POW). See other materials for information on non-endemic arboviruses (e.g., dengue fever and yellow fever) Provider Responsibilities 1. Report suspect and confirmed cases of arbovirus infection (including copies of lab results) to the local health department within one week of diagnosis. Supply requested clinical information to the local health department to assist with case ascertainment. 2. Assure appropriate testing is completed for patients with suspected arboviral infection. The preferred diagnostic test is testing of virus-specific IgM antibodies in serum or cerebrospinal fluid (CSF). In West Virginia, appropriate arbovirus testing should include EEE, LAC, SLE, and WNV. Testing for a complete arboviral panel is available free of charge through the West Virginia Office of Laboratory Services (OLS). Laboratory Responsibilities 1. Report positive laboratory results for arbovirus infection to the local health department within 1 week. 2. Submit positive arboviral samples to the Office of Laboratory Services within 1 week. 3. Appropriate testing for patients with suspected arboviral infection includes testing of virus-specific IgM antibodies in serum or CSF. In West Virginia, testing should routinely be conducted for WNV, EEE, SLE, and LAC. A complete arboviral panel is available free of charge through OLS. For more information go to: http://www.wvdhhr.org/labservices/labs/virology/arbovirus.cfm Local Health Responsibilities 1. Conduct an appropriate case investigation. -

MDHHS BOL Mosquito-Borne and Tick-Borne Disease Testing
MDHHS BUREAU OF LABORATORIES MOSQUITO-BORNE AND TICK-BORNE DISEASE TESTING MOSQUITO-BORNE DISEASES The Michigan Department of Health and Human Services Bureau of Laboratories (MDHHS BOL) offers comprehensive testing on clinical specimens for the following viral mosquito-borne diseases (also known as arboviruses) of concern in Michigan: California Group encephalitis viruses including La Crosse encephalitis virus (LAC) and Jamestown Canyon virus (JCV), Eastern Equine encephalitis virus (EEE), St. Louis encephalitis virus (SLE), and West Nile virus (WNV). Testing is available free of charge through Michigan healthcare providers for their patients. Testing for mosquito-borne viruses should be considered in patients presenting with meningitis, encephalitis, or other acute neurologic illness in which an infectious etiology is suspected during the summer months in Michigan. Methodologies include: • IgM detection for five arboviruses (LAC, JCV, EEE, SLE, WNV) • Molecular detection (PCR) for WNV only • Plaque Reduction Neutralization Test (PRNT) is also available and may be performed on select samples when indicated The preferred sample for arbovirus serology at MDHHS BOL is cerebral spinal fluid (CSF), followed by paired serum samples (acute and convalescent). In cases where CSF volume may be small, it is recommended to also include an acute serum sample. Please see the following document for detailed instructions on specimen requirements, shipping and handling instructions: http://www.michigan.gov/documents/LSGArbovirus_IgM_Antibody_Panel_8347_7.doc Michigan residents may also be exposed to mosquito-borne viruses when traveling domestically or internationally. In recent years, the most common arboviruses impacting travelers include dengue, Zika and chikungunya virus. MDHHS has the capacity to perform PCR for dengue, chikungunya and Zika virus and IgM for dengue and Zika virus to confirm commercial laboratory arbovirus findings or for complicated medical investigations. -

What Is Veterinary Public Health? Zoonosis
Your Zoonosis Connection Veterinary Public Health Division Volume 4, Issue 1 March 2012 612 Canino Rd., Houston, Texas 77076 Phone: 281-999-3191 Fax: 281-847-1911 Harris County Rabies Update Inside this issue: Rabies continues to be a serious health threat to people and domestic What is Veterinary 2 animals. In the United States prior to 1960, the majority of all animal cases re- Public Health ported to the Centers for Disease Control and Prevention were seen in do- Rabies Submissions 3 mestic animals. Now more than 90% of the cases occur in wild animals. Since the 1950s, human rabies deaths have declined from more than a 100 annually Continuing Education 3 to a couple each year. This reduction in the number of human deaths associat- ed with rabies can be attributed to the implementation of rabies vaccination Zoonosis Trivia 4 laws, oral rabies vaccination programs, improved public health practices and the increased administration of post-exposure prophylaxis. Did you know? Veterinarians are In Harris County, rabies was last documented in a dog in 1979 and in a cat in uniquely qualified to 1986. However, rabies continues to be enzootic in our bat population. In address issues and 2011, 4.3% of bats submitted for testing were positive for rabies, which has de- concerns related to clined from 7.9% in 2010 (see table below). Last year, one horse and two the interactions of skunks tested positive for rabies in Harris County. The horse was infected people, animals, and with the South Central Skunk strain of rabies, which often spills over into oth- the environment. -

Arbovirus Discovery in Central African Republic (1973-1993): Zika, Bozo
Research Article Annals of Infectious Disease and Epidemiology Published: 13 Nov, 2017 Arbovirus Discovery in Central African Republic (1973- 1993): Zika, Bozo, Bouboui, and More Jean François Saluzzo1, Tom Vincent2, Jay Miller3, Francisco Veas4 and Jean-Paul Gonzalez5* 1Fab’entech, Lyon, France 2O’Neill Institute for National and Global Health Law, Georgetown University Law Center, Washington, DC, USA 3Department of Infectious Disease, Health Security Partners, Washington, DC, USA 4Laboratoire d’Immunophysiopathologie Moléculaire Comparée-UMR- Ministère de la Défense3, Institute de Recherche pour le Développement, Montpellier, France 5Center of Excellence for Emerging and Zoonotic Animal Disease, Kansas State University, Manhattan, KS, USA Abstract The progressive research on yellow fever and the subsequent emergence of the field of arbovirology in the 1950s gave rise to the continued development of a global arbovirus surveillance network with a specific focus on human pathogenic arboviruses of the tropical zone. Though unknown at the time, some of the arboviruses studies would emerge within the temperate zone decades later (e.g.: West Nile, Zika, Chikungunya). However, initial research by the surveillance network was heavily focused on the discovery, isolation, and characterization of numerous arbovirus species. Global arboviral surveillance has revealed a cryptic circulation of several arboviruses, mainly in wild cycles of the tropical forest. Although there are more than 500 registered arbovirus species, a mere one third has proved to be pathogenic to humans (CDC, 2015). Indeed, most known arboviruses did not initially demonstrate a pathogenicity to humans or other vertebrates, and were considered “orphans” (i.e. without known of vertebrate hosts). As a part of this global surveillance network, the Institut Pasteur International Network has endeavored to understand the role played by arboviruses in the etiology of febrile syndromes of unknown origin as one of its research missions. -

Potential Arbovirus Emergence and Implications for the United Kingdom Ernest Andrew Gould,* Stephen Higgs,† Alan Buckley,* and Tamara Sergeevna Gritsun*
Potential Arbovirus Emergence and Implications for the United Kingdom Ernest Andrew Gould,* Stephen Higgs,† Alan Buckley,* and Tamara Sergeevna Gritsun* Arboviruses have evolved a number of strategies to Chikungunya virus and in the family Bunyaviridae, sand- survive environmental challenges. This review examines fly fever Naples virus (often referred to as Toscana virus), the factors that may determine arbovirus emergence, pro- sandfly fever Sicilian virus, Crimean-Congo hemorrhagic vides examples of arboviruses that have emerged into new fever virus (CCHFV), Inkoo virus, and Tahyna virus, habitats, reviews the arbovirus situation in western Europe which is widespread throughout Europe. Rift Valley fever in detail, discusses potential arthropod vectors, and attempts to predict the risk for arbovirus emergence in the virus (RVFV) and Nairobi sheep disease virus (NSDV) United Kingdom. We conclude that climate change is prob- could be introduced to Europe from Africa through animal ably the most important requirement for the emergence of transportation. Finally, the family Reoviridae contains a arthropodborne diseases such as dengue fever, yellow variety of animal arbovirus pathogens, including blue- fever, Rift Valley fever, Japanese encephalitis, Crimean- tongue virus and African horse sickness virus, both known Congo hemorrhagic fever, bluetongue, and African horse to be circulating in Europe. This review considers whether sickness in the United Kingdom. While other arboviruses, any of these pathogenic arboviruses are likely to emerge such as West Nile virus, Sindbis virus, Tahyna virus, and and cause disease in the United Kingdom in the foresee- Louping ill virus, apparently circulate in the United able future. Kingdom, they do not appear to present an imminent threat to humans or animals. -

Florida Arbovirus Surveillance Week 13: March 28-April 3, 2021
Florida Arbovirus Surveillance Week 13: March 28-April 3, 2021 Arbovirus surveillance in Florida includes endemic mosquito-borne viruses such as West Nile virus (WNV), Eastern equine encephalitis virus (EEEV), and St. Louis encephalitis virus (SLEV), as well as exotic viruses such as dengue virus (DENV), chikungunya virus (CHIKV), Zika virus (ZIKV), and California encephalitis group viruses (CEV). Malaria, a parasitic mosquito-borne disease is also included. During the period of March 28- April 3, 2021, the following arboviral activity was recorded in Florida. WNV activity: No human cases of WNV infection were reported this week. No horses with WNV infection were reported this week. No sentinel chickens tested positive for antibodies to WNV this week. In 2021, positive samples from two sentinel chickens has been reported from two counties. SLEV activity: No human cases of SLEV infection were reported this week. No sentinel chickens tested positive for antibodies to SLEV this week. In 2021, no positive samples have been reported. EEEV activity: No human cases of EEEV infection were reported this week. No horses with EEEV infection were reported this week. No sentinel chickens tested positive for antibodies to EEEV this week. In 2021, positive samples from one horse and 14 sentinel chickens have been reported from four counties. International Travel-Associated Dengue Fever Cases: No cases of dengue fever were reported this week in persons that had international travel. In 2021, one travel-associated dengue fever case has been reported. Dengue Fever Cases Acquired in Florida: No cases of locally acquired dengue fever were reported this week. In 2021, no cases of locally acquired dengue fever have been reported. -

Taxonomy of the Order Bunyavirales: Update 2019
Archives of Virology (2019) 164:1949–1965 https://doi.org/10.1007/s00705-019-04253-6 VIROLOGY DIVISION NEWS Taxonomy of the order Bunyavirales: update 2019 Abulikemu Abudurexiti1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Tatjana Avšič‑Županc5 · Matthew J. Ballinger6 · Dennis A. Bente7 · Martin Beer8 · Éric Bergeron9 · Carol D. Blair10 · Thomas Briese11 · Michael J. Buchmeier12 · Felicity J. Burt13 · Charles H. Calisher10 · Chénchén Cháng14 · Rémi N. Charrel15 · Il Ryong Choi16 · J. Christopher S. Clegg17 · Juan Carlos de la Torre18 · Xavier de Lamballerie15 · Fēi Dèng19 · Francesco Di Serio20 · Michele Digiaro21 · Michael A. Drebot22 · Xiaˇoméi Duàn14 · Hideki Ebihara23 · Toufc Elbeaino21 · Koray Ergünay24 · Charles F. Fulhorst7 · Aura R. Garrison25 · George Fú Gāo26 · Jean‑Paul J. Gonzalez27 · Martin H. Groschup28 · Stephan Günther29 · Anne‑Lise Haenni30 · Roy A. Hall31 · Jussi Hepojoki32,33 · Roger Hewson34 · Zhìhóng Hú19 · Holly R. Hughes35 · Miranda Gilda Jonson36 · Sandra Junglen37,38 · Boris Klempa39 · Jonas Klingström40 · Chūn Kòu14 · Lies Laenen41,42 · Amy J. Lambert35 · Stanley A. Langevin43 · Dan Liu44 · Igor S. Lukashevich45 · Tāo Luò1 · Chuánwèi Lüˇ 19 · Piet Maes41 · William Marciel de Souza46 · Marco Marklewitz37,38 · Giovanni P. Martelli47 · Keita Matsuno48,49 · Nicole Mielke‑Ehret50 · Maria Minutolo3 · Ali Mirazimi51 · Abulimiti Moming14 · Hans‑Peter Mühlbach50 · Rayapati Naidu52 · Beatriz Navarro20 · Márcio Roberto Teixeira Nunes53 · Gustavo Palacios25 · Anna Papa54 · Alex Pauvolid‑Corrêa55 · Janusz T. Pawęska56,57 · Jié Qiáo19 · Sheli R. Radoshitzky25 · Renato O. Resende58 · Víctor Romanowski59 · Amadou Alpha Sall60 · Maria S. Salvato61 · Takahide Sasaya62 · Shū Shěn19 · Xiǎohóng Shí63 · Yukio Shirako64 · Peter Simmonds65 · Manuela Sironi66 · Jin‑Won Song67 · Jessica R. Spengler9 · Mark D. Stenglein68 · Zhèngyuán Sū19 · Sùróng Sūn14 · Shuāng Táng19 · Massimo Turina69 · Bó Wáng19 · Chéng Wáng1 · Huálín Wáng19 · Jūn Wáng19 · Tàiyún Wèi70 · Anna E. -

Notification Requirements
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2021 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of within the next reporting cycle. a case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 Approved by CSTE: June 2019 within 24 hours of a case meeting the notification criteria, followed by Interim Update Approved by CSTE: April 5, 2020 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2020 electronic transmission. Updated: May 28, 2020 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Page 1 of 5 Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis -

Fragile Transmission Cycles of Tick-Borne Encephalitis Virus May Be Disrupted by Predicted Climate Change
doi 10.1098/rspb.2000.1204 Fragiletransmissionc yclesof tick-borne encephalitisvirusmaybedisruptedbypredicted climatechange Sarah E.Randolph * and David J.Rogers Department of Zoology,University of Oxford, SouthP arks Road, Oxford OX13PS, U K Repeatedpredictions that vector-bornedisease prevalencewill increase withglobal warming are usually basedon univariatemodels. T oaccommodatethe fullrange of constraints, the present-daydistribution of tick-borneencephalitis virus (TBEv) was matched statistically tocurrent climatic variables,to provide a multivariatedescription of present-day areas of disease risk.This was then appliedto outputs ofageneral circulationmodel that predicts howclimatic variablesmay change in the future, andfuture distributions ofTBEv were predicted forthem. Theexpected summer rise intemperature anddecrease inmoisture appearsto drive the distributionof TBEv into higher-latitude and higher-altitude regions progressively throughthe 2020s,2050s and 208 0s.The ¢ naltoe-hold in the 2080smay be con¢ ned to a small partof Scandinavia,including new foci in southern Finland. The reason for this apparentcontraction of the rangeof TBEv is that its transmission cycles dependon a particularpattern oftick seasonal dynamics, whichmay be disrupted byclimate change.The observed marked increase inincidence of tick-borne encephalitisin most parts ofEuropesince 1993may be dueto non-biological causes, such aspoliticaland sociologicalchanges. Keywords: ticks; tick-borneencephalitis; global warming ;climate matching;risk maps the winter withminimum temperatures below 712 8C. 1.INTRODUCTION Further south,in areas with medium tohigh tick densi- Tick-borneencephalitis (TBE) ,causedby two subtypes of ties, further increases intick abundance were related to a £avivirus(TBEv) transmitted bythe ticks Ixodes ricinus combinationof milder winters (fewer dayswith minimum and I.persulcatus ,is the most signi¢cant vector-borne temperatures below 7 7 8C)and extended spring and disease inEurope and Eurasia. -

MI Weekly Arbovirus Summary, 2020
Arbovirus* Activity, Including West Nile Virus and Eastern Equine Encephalitis: Weekly Summary, Michigan 2020 *Arboviruses are viruses transmitted by mosquitoes or other insects Updated: August 20, 2020 12Mosquito pools testing 2 Human1 cases of West Birds testing positive for positive for West Nile West Nile virus infection Nile virus or other virus infection arboviruses reported 2020 Michigan Arbovirus Surveillance (click links below to see map** of cases by county) Highlights West Nile virus Positive Mosquito Pools 12 • EEE has been reported in 2 horses, from Clare and Montcalm County. Total Number of Mosquito Pools Tested 272 • For 2020, West Nile Virus (WNV) has been reported in 2 birds from Lapeer County and Total Number of Mosquitoes Tested 5323 Oakland County, and mosquito pools in Kent, Human WNV cases 0 Oakland, and Saginaw Counties. • One human case of Jamestown Canyon Human California Group virus cases 1 virus(a California Group virus) has been reported in a resident of Ottawa County. WNV asymptomatic, viremic blood donor 0 • In 2019, Michigan experienced its largest ever Equine/Other Animal WNV cases reported 0 outbreak of Eastern Equine encephalitis (EEE). Ten Michigan residents (1 Barry, 2 Berrien, 1 Avian WNV cases reported 2 Calhoun, 2 Cass, 3 Kalamazoo, and 1 Van Buren) were infected, with 6 fatalities; 50 EEE Human Eastern Equine Encephalitis cases reported 0 positive animals were also reported. Animal Eastern Equine Encephalitis cases reported 2 **data in linked maps may lag behind this report by 1-2 business days. -

Cleveland Clinic Zika Virus
Zika Virus What is the Zika virus? The Zika virus is an arbovirus transmitted by mosquitoes. The Zika virus is thought to be linked to a rise in the cases of a birth defect called microcephaly. This defect leaves a baby with an abnormally small head and a shorter life expectancy. The baby’s brain is also small and is not completely developed. The Centers for Disease Control and Prevention (CDC) performed lab tests that suggest a link between the Zika virus and some of the more than 3,500 babies born in Brazil with microcephaly in 2015. The CDC is advising women who are pregnant or thinking of becoming pregnant to avoid going to countries in South America, Central America, Mexico, and the Caribbean, where the virus is rapidly spreading. What causes the Zika virus? The Zika virus is spread by mosquito bites from infected mosquitoes. In most cases, these mosquitoes are found in tropical regions. What are the symptoms of the Zika virus? Symptoms usually are mild, and include: Fever Skin rashes Conjunctivitis (pinkeye) Headaches Pain in the muscles and joints How is the Zika virus treated? Currently, there is no vaccine for the virus. The CDC recommends supportive care. If a person is sick with the Zika virus, he or she should drink lots of fluids, rest, and take medicine (Tylenol) for pain and fever. A person with the virus should see a doctor if symptoms get worse. How can the Zika virus be prevented? It is important to avoid mosquito bites. Insect repellents and public mosquito control measures can help cut down on the number of mosquitoes present. -
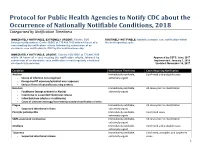
Protocol for Public Health Agencies to Notify CDC About the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification within Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of a the next reporting cycle. case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 within 24 hours of a case meeting the notification criteria, followed by Approved by CSTE: June 2017 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2018 electronic transmission. Updated: November 16, 2017 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis Immediately notifiable, Confirmed cases extremely