DSHS Arbovirus Activity 061817
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wnv-Case-Definition.Pdf
Draft Case Definition for West Nile Fever Animal and Plant Health Inspection Service West Nile Fever Veterinary Services October 2018 Case Definition (Notifiable) 1. Clinical Signs 1.1 Clinical Signs: West Nile Fever (WNF) is a zoonotic mosquito-borne viral disease caused by the West Nile virus (WNV), a Flavivirus of the family Flaviviridae. Many vertebrate species are susceptible to natural WNV infection; however, fatal neurological outbreaks have only been documented in equids, humans, geese, wild birds (particularly corvids), squirrels, farmed alligators, and dogs. Birds serve as the natural host reservoir of WNV. The incubation period is estimated to be three to 15 days in horses Ten to 39 percent of unvaccinated horses infected with WNV will develop clinical signs. Most clinically affected horses exhibit neurological signs such as ataxia (including stumbling, staggering, wobbly gait, or incoordination) or at least two of the following: circling, hind limb weakness, recumbency or inability to stand (or both), multiple limb paralysis, muscle fasciculation, proprioceptive deficits, altered mental status, blindness, lip droop/paralysis, teeth grinding. Behavioral changes including somnolence, listlessness, apprehension, or periods of hyperexcitability may occur. Other common clinical signs include colic, lameness, anorexia, and fever. 2. Laboratory criteria: 2.1 Agent isolation and identification: The virus can be identified by polymerase chain reaction (PCR) and virus isolation (VI). Preferred tissues from equids are brain or spinal cord. 2.2 Serology: Antibody titers can be identified in paired serum samples by IgM and IgG capture enzyme linked immunosorbent assay (ELISA), plaque reduction neutralization test (PRNT), and virus neutralization (VN). Only a single serum sample is required for IgM capture ELISA, and this is the preferred serologic test in live animals. -

Rift Valley Fever for Host Innate Immunity in Resistance to a New
A New Mouse Model Reveals a Critical Role for Host Innate Immunity in Resistance to Rift Valley Fever This information is current as Tânia Zaverucha do Valle, Agnès Billecocq, Laurent of September 25, 2021. Guillemot, Rudi Alberts, Céline Gommet, Robert Geffers, Kátia Calabrese, Klaus Schughart, Michèle Bouloy, Xavier Montagutelli and Jean-Jacques Panthier J Immunol 2010; 185:6146-6156; Prepublished online 11 October 2010; Downloaded from doi: 10.4049/jimmunol.1000949 http://www.jimmunol.org/content/185/10/6146 Supplementary http://www.jimmunol.org/content/suppl/2010/10/12/jimmunol.100094 http://www.jimmunol.org/ Material 9.DC1 References This article cites 46 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/185/10/6146.full#ref-list-1 Why The JI? Submit online. by guest on September 25, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American -

Taxonomy of the Order Bunyavirales: Update 2019
Archives of Virology (2019) 164:1949–1965 https://doi.org/10.1007/s00705-019-04253-6 VIROLOGY DIVISION NEWS Taxonomy of the order Bunyavirales: update 2019 Abulikemu Abudurexiti1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Tatjana Avšič‑Županc5 · Matthew J. Ballinger6 · Dennis A. Bente7 · Martin Beer8 · Éric Bergeron9 · Carol D. Blair10 · Thomas Briese11 · Michael J. Buchmeier12 · Felicity J. Burt13 · Charles H. Calisher10 · Chénchén Cháng14 · Rémi N. Charrel15 · Il Ryong Choi16 · J. Christopher S. Clegg17 · Juan Carlos de la Torre18 · Xavier de Lamballerie15 · Fēi Dèng19 · Francesco Di Serio20 · Michele Digiaro21 · Michael A. Drebot22 · Xiaˇoméi Duàn14 · Hideki Ebihara23 · Toufc Elbeaino21 · Koray Ergünay24 · Charles F. Fulhorst7 · Aura R. Garrison25 · George Fú Gāo26 · Jean‑Paul J. Gonzalez27 · Martin H. Groschup28 · Stephan Günther29 · Anne‑Lise Haenni30 · Roy A. Hall31 · Jussi Hepojoki32,33 · Roger Hewson34 · Zhìhóng Hú19 · Holly R. Hughes35 · Miranda Gilda Jonson36 · Sandra Junglen37,38 · Boris Klempa39 · Jonas Klingström40 · Chūn Kòu14 · Lies Laenen41,42 · Amy J. Lambert35 · Stanley A. Langevin43 · Dan Liu44 · Igor S. Lukashevich45 · Tāo Luò1 · Chuánwèi Lüˇ 19 · Piet Maes41 · William Marciel de Souza46 · Marco Marklewitz37,38 · Giovanni P. Martelli47 · Keita Matsuno48,49 · Nicole Mielke‑Ehret50 · Maria Minutolo3 · Ali Mirazimi51 · Abulimiti Moming14 · Hans‑Peter Mühlbach50 · Rayapati Naidu52 · Beatriz Navarro20 · Márcio Roberto Teixeira Nunes53 · Gustavo Palacios25 · Anna Papa54 · Alex Pauvolid‑Corrêa55 · Janusz T. Pawęska56,57 · Jié Qiáo19 · Sheli R. Radoshitzky25 · Renato O. Resende58 · Víctor Romanowski59 · Amadou Alpha Sall60 · Maria S. Salvato61 · Takahide Sasaya62 · Shū Shěn19 · Xiǎohóng Shí63 · Yukio Shirako64 · Peter Simmonds65 · Manuela Sironi66 · Jin‑Won Song67 · Jessica R. Spengler9 · Mark D. Stenglein68 · Zhèngyuán Sū19 · Sùróng Sūn14 · Shuāng Táng19 · Massimo Turina69 · Bó Wáng19 · Chéng Wáng1 · Huálín Wáng19 · Jūn Wáng19 · Tàiyún Wèi70 · Anna E. -

Notification Requirements
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2021 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of within the next reporting cycle. a case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 Approved by CSTE: June 2019 within 24 hours of a case meeting the notification criteria, followed by Interim Update Approved by CSTE: April 5, 2020 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2020 electronic transmission. Updated: May 28, 2020 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Page 1 of 5 Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis -
West Nile Virus Questions and Answers
West Nile Virus Questions and Answers Q: How do people get infected with West Nile Virus (WNV)? A: The most likely way a human would become infected with WNV is through the bite of an infected mosquito. Some people have also become infected with WNV following receipt of contaminated blood or blood products, or transplanted organs from an infected donor. Mothers who are recently infected with WNV may also transmit the virus to their unborn child, or to their baby while breastfeeding. Q: Who is at risk for getting West Nile encephalitis? A: All residents of areas where WNV activity has been identified are at risk of getting West Nile encephalitis. Q: What is the time from exposure to onset of disease symptoms for West Nile encephalitis in humans? A: Usually 3 to 15 days. Q: What are the symptoms of West Nile virus infection? A: Most people who are infected with WNV will not have any noticeable illness, or have a mild form of illness called West Nile Fever. Persons with West Nile Fever typically experience symptoms of fever, headache, nausea, muscle weakness, and body aches lasting 2 to 6 days or longer. Sensitivity when looking at light and a skin rash appearing on the trunk of the body may also be present. Approximately 20% of persons infected with WNV will develop more severe neurologic disease that may be life-threatening. Adults over the age of 50 years are at greater risk of having serious disease. Potential symptoms of severe infection (West Nile encephalitis or meningitis) include intense headache, dizziness, severe muscle weakness, neck stiffness, vomiting, disorientation, mental confusion, tremors, muscle paralysis, or convulsions and coma. -

2018 DSHS Arbovirus Activity
Health and Human Texas Department of State Services Health Services Arbovirus Activity in Texas 2018 Surveillance Report August 2019 Texas Department of State Health Services Zoonosis Control Branch Overview Viruses transmitted by mosquitoes are referred to as arthropod-borne viruses or arboviruses. Arboviruses reported in Texas may include California (CAL) serogroup viruses, chikungunya virus (CHIKV), dengue virus (DENV), eastern equine encephalitis virus (EEEV), Saint Louis encephalitis virus (SLEV), western equine encephalitis virus (WEEV), West Nile virus (WNV), and Zika virus (ZIKV), many of which are endemic or enzootic in the state. In 2018, reported human arboviral disease cases were attributed to WNV (82%), DENV (11%), CHIKV (4%), ZIKV (2%), and CAL (1%) (Table 1). In addition, there were two cases reported as arbovirus disease cases which could not be diagnostically or epidemiologically differentiated between DENV and ZIKV. Animal infections or disease caused by WNV and SLEV were also reported during 2018. Local transmission of DENV, SLEV, and WNV was documented during 2018 (Figure 1). No reports of EEEV or WEEV were received during 2018. Table 1. Year-End Arbovirus Activity Summary, Texas, 2018 Positive Human* Arbovirus Mosquito Avian Equine TOTAL TOTAL Fever Neuroinvasive Severe Deaths PVD‡ Pools (Human) CAL 1 1 1 CHIK 7 7 7 DEN 20 20 20 SLE 2 0 2 WN 1,021 6 19 38 108 146 11 24 1,192 Zika** 4 4 TOTAL 1,023 6 19 65 109 0 178 11 24 1,226 CAL - California serogroup includes California encephalitis, Jamestown Canyon, Keystone, La Crosse, Snowshoe hare and Trivittatus viruses CHIK - Chikungunya DEN - Dengue SLE - Saint Louis encephalitis WN - West Nile ‡PVD - Presumptive viremic blood donors are people who had no symptoms at the time of donating blood through a blood collection agency, but whose blood tested positive when screened for the presence of West Nile virus or Zika virus. -

West Nile Virus
Oklahoma State Department of Health Acute Disease Service Public Health Fact Sheet West Nile Virus What is West Nile virus? West Nile virus is one of a group of viruses called arboviruses that are spread by mosquitoes and may cause illness in birds, animals, and humans. West Nile virus was not known to be present in the United States until the summer of 1999. Previously, West Nile virus was only found in Africa, western Asia, the Middle East, and Eastern Europe. Where is West Nile virus in the United States? West Nile virus was first identified as a disease threat in the United States during the summer of 1999 and was limited to the northeastern states through 2000. However, the virus rapidly expanded its geographic range. By the end of 2004, West Nile virus had spread from the Atlantic to the Pacific coast with viral activity confirmed in all 48 contiguous states. How is it spread? West Nile virus is primarily spread through the bite of an infected mosquito. Mosquitoes pick up the virus when they feed on infected birds. The virus must then circulate in the mosquito for a few days before they are capable of passing the infection to animals or humans while biting. West Nile virus is not spread person to person through casual contact such as touching or kissing. Rarely, West Nile virus has also been spread through blood transfusions, although blood banks do screen blood supply for the infection. How long does it take to get sick after a bite from an infected mosquito? It takes about three to 15 days for both human and equine (horse, mule, or donkey) illness to occur after a bite from infected mosquito. -
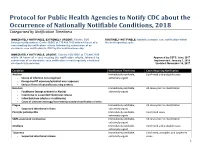
Protocol for Public Health Agencies to Notify CDC About the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness
Protocol for Public Health Agencies to Notify CDC about the Occurrence of Nationally Notifiable Conditions, 2018 Categorized by Notification Timeliness IMMEDIATELY NOTIFIABLE, EXTREMELY URGENT: Call the CDC ROUTINELY NOTIFIABLE: Submit electronic case notification within Emergency Operations Center (EOC) at 770.488.7100 within 4 hours of a the next reporting cycle. case meeting the notification criteria, followed by submission of an electronic case notification to CDC by the next business day. IMMEDIATELY NOTIFIABLE, URGENT: Call the CDC EOC at 770.488.7100 within 24 hours of a case meeting the notification criteria, followed by Approved by CSTE: June 2017 submission of an electronic case notification in next regularly scheduled Implemented: January 1, 2018 electronic transmission. Updated: November 16, 2017 Condition Notification Timeliness Cases Requiring Notification Anthrax Immediately notifiable, Confirmed and probable cases - Source of infection not recognized extremely urgent - Recognized BT exposure/potential mass exposure - Serious illness of naturally-occurring anthrax Botulism Immediately notifiable, All cases prior to classification - Foodborne (except endemic to Alaska) extremely urgent - Intentional or suspected intentional release - Infant botulism (clusters or outbreaks) - Cases of unknown etiology/not meeting standard notification criteria Plague Immediately notifiable, All cases prior to classification - Suspected intentional release extremely urgent Paralytic poliomyelitis Immediately notifiable, Confirmed cases extremely -

Taxonomy of the Family Arenaviridae and the Order Bunyavirales: Update 2018
Archives of Virology https://doi.org/10.1007/s00705-018-3843-5 VIROLOGY DIVISION NEWS Taxonomy of the family Arenaviridae and the order Bunyavirales: update 2018 Piet Maes1 · Sergey V. Alkhovsky2 · Yīmíng Bào3 · Martin Beer4 · Monica Birkhead5 · Thomas Briese6 · Michael J. Buchmeier7 · Charles H. Calisher8 · Rémi N. Charrel9 · Il Ryong Choi10 · Christopher S. Clegg11 · Juan Carlos de la Torre12 · Eric Delwart13,14 · Joseph L. DeRisi15 · Patrick L. Di Bello16 · Francesco Di Serio17 · Michele Digiaro18 · Valerian V. Dolja19 · Christian Drosten20,21,22 · Tobiasz Z. Druciarek16 · Jiang Du23 · Hideki Ebihara24 · Toufc Elbeaino18 · Rose C. Gergerich16 · Amethyst N. Gillis25 · Jean‑Paul J. Gonzalez26 · Anne‑Lise Haenni27 · Jussi Hepojoki28,29 · Udo Hetzel29,30 · Thiện Hồ16 · Ní Hóng31 · Rakesh K. Jain32 · Petrus Jansen van Vuren5,33 · Qi Jin34,35 · Miranda Gilda Jonson36 · Sandra Junglen20,22 · Karen E. Keller37 · Alan Kemp5 · Anja Kipar29,30 · Nikola O. Kondov13 · Eugene V. Koonin38 · Richard Kormelink39 · Yegor Korzyukov28 · Mart Krupovic40 · Amy J. Lambert41 · Alma G. Laney42 · Matthew LeBreton43 · Igor S. Lukashevich44 · Marco Marklewitz20,22 · Wanda Markotter5,33 · Giovanni P. Martelli45 · Robert R. Martin37 · Nicole Mielke‑Ehret46 · Hans‑Peter Mühlbach46 · Beatriz Navarro17 · Terry Fei Fan Ng14 · Márcio Roberto Teixeira Nunes47,48 · Gustavo Palacios49 · Janusz T. Pawęska5,33 · Clarence J. Peters50 · Alexander Plyusnin28 · Sheli R. Radoshitzky49 · Víctor Romanowski51 · Pertteli Salmenperä28,52 · Maria S. Salvato53 · Hélène Sanfaçon54 · Takahide Sasaya55 · Connie Schmaljohn49 · Bradley S. Schneider25 · Yukio Shirako56 · Stuart Siddell57 · Tarja A. Sironen28 · Mark D. Stenglein58 · Nadia Storm5 · Harikishan Sudini59 · Robert B. Tesh48 · Ioannis E. Tzanetakis16 · Mangala Uppala59 · Olli Vapalahti28,30,60 · Nikos Vasilakis48 · Peter J. Walker61 · Guópíng Wáng31 · Lìpíng Wáng31 · Yànxiăng Wáng31 · Tàiyún Wèi62 · Michael R. -
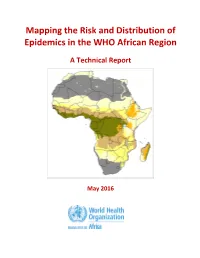
Mapping the Risk and Distribution of Epidemics in the WHO African Region
Mapping the Risk and Distribution of Epidemics in the WHO African Region A Technical Report May 2016 WHO/AFRO Library Cataloguing – in – Publication Data Mapping the Risk and Distribution of Epidemics in the WHO African Region: a technical report 1. Disease Outbreaks – statistics and numerical data 2. Epidemics – statistics and numerical data 3. Communicable Diseases – statistics and numerical data 4. Risk Assessment – supply and distribution – statistics and numerical data 5. Data collection – utilization 6. Africa I. Work Health Organization. Regional Office for Africa II. Title ISBN: 978-9290233084-4 (NLM Classification : WA 105) © WHO Regional Office for Africa, 2016 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. Copies of this publication may be obtained from the Library, WHO Regional Office for Africa, P.O. Box 6, Brazzaville, Republic of Congo (Tel: +47 241 39100; Fax: +47 241 39507; E-mail: [email protected]). Requests for permission to reproduce or translate this publication – whether for sale or for non-commercial distribution – should be sent to the same address. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

West Nile Virus
West Nile Virus Frequently Asked Questions What is West Nile virus? West Nile virus is a viral infection that is spread by the bite of an infected mosquito. Mosquitoes get infected with the West Nile virus by feeding on infected birds. The infected mosquitoes then spread the virus by biting humans and other animals, such as horses. Identified in the United States in 1999, West Nile virus is seen most often during the summer and early fall months. Who gets West Nile virus? Anyone can get infected with the West Nile virus. The virus can affect anyone bitten by an infected mosquito. People over the age of 50 and people with weak immune systems are at greater risk of developing severe illness. How do people get West Nile virus? The virus is spread by the bite of a mosquito infected with the West Nile virus. What are the symptoms of West Nile virus? Many people infected with West Nile virus do not become ill and may not develop symptoms. About 20% of infected people will develop West Nile fever. When symptoms do occur, they may be mild or severe and show up 3 to 15 days after being bitten by an infected mosquito. • Mild symptoms inlcude flu-like illness with fever, headache, body aches, nausea and sometimes swollen lymph glands or a skin rash on the chest, stomach and back. • Severe symptoms include high fever, neck stiffness and swelling of the brain (encephalitis) which can lead to coma, convulsions and death. Less than 1% of infected people will develop severe symptoms. -

Zoonotic Potential of International Trade in CITES-Listed Species Annexes B, C and D JNCC Report No
Zoonotic potential of international trade in CITES-listed species Annexes B, C and D JNCC Report No. 678 Zoonotic potential of international trade in CITES-listed species Annex B: Taxonomic orders and associated zoonotic diseases Annex C: CITES-listed species and directly associated zoonotic diseases Annex D: Full trade summaries by taxonomic family UNEP-WCMC & JNCC May 2021 © JNCC, Peterborough 2021 Zoonotic potential of international trade in CITES-listed species Prepared for JNCC Published May 2021 Copyright JNCC, Peterborough 2021 Citation UNEP-WCMC and JNCC, 2021. Zoonotic potential of international trade in CITES- listed species. JNCC Report No. 678, JNCC, Peterborough, ISSN 0963-8091. Contributing authors Stafford, C., Pavitt, A., Vitale, J., Blömer, N., McLardy, C., Phillips, K., Scholz, L., Littlewood, A.H.L, Fleming, L.V. & Malsch, K. Acknowledgements We are grateful for the constructive comments and input from Jules McAlpine (JNCC), Becky Austin (JNCC), Neville Ash (UNEP-WCMC) and Doreen Robinson (UNEP). We also thank colleagues from OIE for their expert input and review in relation to the zoonotic disease dataset. Cover Photographs Adobe Stock images ISSN 0963-8091 JNCC Report No. 678: Zoonotic potential of international trade in CITES-listed species Annex B: Taxonomic orders and associated zoonotic diseases Annex B: Taxonomic orders and associated zoonotic diseases Table B1: Taxonomic orders1 associated with at least one zoonotic disease according to the source papers, ranked by number of associated zoonotic diseases identified.