Mapping the Risk and Distribution of Epidemics in the WHO African Region
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Linking Behavior, Co-Infection Patterns, and Viral Infection Risk with the Whole Gastrointestinal Helminth Community Structure in Mastomys Natalensis
ORIGINAL RESEARCH published: 17 August 2021 doi: 10.3389/fvets.2021.669058 Linking Behavior, Co-infection Patterns, and Viral Infection Risk With the Whole Gastrointestinal Helminth Community Structure in Mastomys natalensis Bram Vanden Broecke 1*, Lisse Bernaerts 1, Alexis Ribas 2, Vincent Sluydts 1, Ladslaus Mnyone 3, Erik Matthysen 1 and Herwig Leirs 1 1 Evolutionary Ecology Group, Department of Biology, University of Antwerp, Antwerp, Belgium, 2 Parasitology Section, Department of Biology, Healthcare and Environment, Faculty of Pharmacy and Food Science, IRBio (Research Institute of Biodiversity), University of Barcelona, Barcelona, Spain, 3 Pest Management Center, Sokoine University of Agriculture, Morogoro, Tanzania Edited by: Yadong Zheng, Infection probability, load, and community structure of helminths varies strongly between Lanzhou Institute of Veterinary and within animal populations. This can be ascribed to environmental stochasticity Research (CAAS), China or due to individual characteristics of the host such as their age or sex. Other, but Reviewed by: Mario Garrido, understudied, factors are the hosts’ behavior and co-infection patterns. In this study, we Ben-Gurion University of the used the multimammate mouse (Mastomys natalensis) as a model system to investigate Negev, Israel Si-Yang Huang, how the hosts’ sex, age, exploration behavior, and viral infection history affects their Yangzhou University, China infection risk, parasitic load, and community structure of gastrointestinal helminths. We Hannah Rose Vineer, hypothesized that the hosts’ exploration behavior would play a key role in the risk for University of Liverpool, United Kingdom infection by different gastrointestinal helminths, whereby highly explorative individuals *Correspondence: would have a higher infection risk leading to a wider diversity of helminths and a larger Bram Vanden Broecke load compared to less explorative individuals. -

Uveal Involvement in Marburg Virus Disease B
Br J Ophthalmol: first published as 10.1136/bjo.61.4.265 on 1 April 1977. Downloaded from British Journal of Ophthalmology, 1977, 61, 265-266 Uveal involvement in Marburg virus disease B. S. KUMING AND N. KOKORIS From the Department of Ophthalmology, Johannesburg General Hospital and University of the Witwatersrand SUMMARY The first reported case of uveal involvement in Marburg virus disease is described. 'Ex Africa semper aliquid novi'. Two outbreaks of Marburg virus disease have been Rhodesia and had also been constantly at his documented. The first occurred in Marburg and bedside till his death. Lassa fever was suspected and Frankfurt, West Germany, in 1967 (Martini, 1969) she was given a unit of Lassa fever convalescent and the second in Johannesburg in 1975 (Gear, serum when she became desperately ill on the fifth 1975). This case report describes the third patient day. She also developed acute pancreatitis. Within in the Johannesburg outbreak, who developed an 52 hours she made a dramatic and uneventful anterior uveitis. The cause of the uveitis was proved recovery. Her illness mainly affected the haema- to be the Marburg virus by identiying it in a tissue topoietic, hepatic, and pancreatic systems. culture of her aqueous fluid. The subject of this report was a nurse who had helped to nurse patients 1 and 2. Nine days after the Case report death ofthe first patient she presented with lower back pain and high fever. She developed hepatitis, a mild Before describing the case history of the patient the disseminated intravascular coagulation syndrome, events leading to her contracting the disease must successfully treated with heparin, and the classical be briefly described. -

Establishment of a Genetically Confirmed Breeding Colony of Mastomys Natalensis from Wild-Caught Founders from West Africa
viruses Article Establishment of a Genetically Confirmed Breeding Colony of Mastomys natalensis from Wild-Caught Founders from West Africa David Safronetz 1,*,†, Kyle Rosenke 1, Robert J. Fischer 2,‡, Rachel A. LaCasse 3, Dana P. Scott 3, Greg Saturday 3, Patrick W. Hanley 3, Ousmane Maiga 4, Nafomon Sogoba 4, Tom G. Schwan 2 and Heinz Feldmann 1,* 1 Laboratory of Virology, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA; [email protected] 2 Laboratory of Zoonotic Pathogens, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA; fi[email protected] (R.J.F.); [email protected] (T.G.S.) 3 Rocky Mountain Veterinary Branch, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA; [email protected] (R.A.L.); [email protected] (D.P.S.); [email protected] (G.S.); [email protected] (P.W.H.) 4 International Center for Excellence in Research (ICER-Mali), Faculty of Medicine and Odonto Stomatology, University of Sciences, Techniques and Technologies of Bamako (USTTB), Bamako, Mali; [email protected] (O.M.); [email protected] (N.S.) * Correspondence: [email protected] (D.S.); [email protected] (H.F.) † Current address: Zoonotic Diseases and Special Pathogens, Public Health Agency of Canada, Winnipeg, MB R3E 3R2, Canada. Citation: Safronetz, D.; Rosenke, K.; ‡ Current Address: Laboratory of Virology, Rocky Mountain Laboratories, National Institute of Allergy Fischer, R.J.; LaCasse, R.A.; Scott, D.P.; and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA. -

Chikungunya Fever: Epidemiology, Clinical Syndrome, Pathogenesis
Antiviral Research 99 (2013) 345–370 Contents lists available at SciVerse ScienceDirect Antiviral Research journal homepage: www.elsevier.com/locate/antiviral Review Chikungunya fever: Epidemiology, clinical syndrome, pathogenesis and therapy ⇑ Simon-Djamel Thiberville a,b, , Nanikaly Moyen a,b, Laurence Dupuis-Maguiraga c,d, Antoine Nougairede a,b, Ernest A. Gould a,b, Pierre Roques c,d, Xavier de Lamballerie a,b a UMR_D 190 ‘‘Emergence des Pathologies Virales’’ (Aix-Marseille Univ. IRD French Institute of Research for Development EHESP French School of Public Health), Marseille, France b University Hospital Institute for Infectious Disease and Tropical Medicine, Marseille, France c CEA, Division of Immuno-Virologie, Institute of Emerging Diseases and Innovative Therapies, Fontenay-aux-Roses, France d UMR E1, University Paris Sud 11, Orsay, France article info abstract Article history: Chikungunya virus (CHIKV) is the aetiological agent of the mosquito-borne disease chikungunya fever, a Received 7 April 2013 debilitating arthritic disease that, during the past 7 years, has caused immeasurable morbidity and some Revised 21 May 2013 mortality in humans, including newborn babies, following its emergence and dispersal out of Africa to the Accepted 18 June 2013 Indian Ocean islands and Asia. Since the first reports of its existence in Africa in the 1950s, more than Available online 28 June 2013 1500 scientific publications on the different aspects of the disease and its causative agent have been pro- duced. Analysis of these publications shows that, following a number of studies in the 1960s and 1970s, Keywords: and in the absence of autochthonous cases in developed countries, the interest of the scientific commu- Chikungunya virus nity remained low. -

Mastomys Spp. – Multimammate Mouse
Mastomys spp. – Multimammate Mouse Taxonomic status: Species Taxonomic notes: A good review of the systematics of Mastomys is provided by Granjon et al. (1997). Mastomys spp. are cryptic and difficult to distinguish morphologically but clearly separable by molecular and chromosomal markers (Britton-Davidian et al. 1995; Lecompte et al. 2005). For example, within the assessment region, M. coucha and M. natalensis can be distinguished only through chromosome number (in M. coucha 2n = 36; in M. natalensis 2n = 32) and molecular markers (Colangelo et al. 2013) but not on cranio-dental features, nor a multivariate analysis (Dippenaar et al. 1993). Mastomys coucha – Richard Yarnell Assessment Rationale Regional Red List status (2016) Both species are listed as Least Concern as they have a Mastomys coucha Least Concern wide distribution within the assessment region, where they likely occur in most protected areas, are abundant in Mastomys natalensis Least Concern human-transformed areas, including agricultural areas and areas affected by human disturbances, and because National Red List status (2004) there are no significant threats that could cause range- Mastomys coucha Least Concern wide decline. Additionally, these species are known as prolific breeders with population numbers likely to recover Mastomys natalensis Least Concern quickly after a decline. Because of their reproductive Reasons for change No change characteristics, population eruptions often occur under favourable conditions. Landowners and managers should Global Red List status (2016) pursue ecologically-based rodent management strategies Mastomys coucha Least Concern and biocontrol instead of rodenticides to regulate population explosions of this species. Mastomys natalensis Least Concern Regional population effects: For M. coucha, significant TOPS listing (NEMBA) (2007) None dispersal is unlikely because the bulk of the population CITES listing None occurs within the assessment region. -

As a Model of Human Ebola Virus Infection
Viruses 2012, 4, 2400-2416; doi:10.3390/v4102400 OPEN ACCESS viruses ISSN 1999-4915 www.mdpi.com/journal/viruses Review The Baboon (Papio spp.) as a Model of Human Ebola Virus Infection Donna L. Perry 1,*, Laura Bollinger 1 and Gary L.White 2 1 Integrated Research Facility, Division of Clinical Research, NIAID, NIH, Frederick, MD, USA; E-Mail: [email protected] 2 Department of Pathology, University of Oklahoma Baboon Research Resource, University of Oklahoma, Ft. Reno Science Park, OK, USA; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-301-631-7249; Fax: +1-301-619-5029. Received: 8 October 2012; in revised form: 17 October 2012 / Accepted: 17 October 2012 / Published: 23 October 2012 Abstract: Baboons are susceptible to natural Ebola virus (EBOV) infection and share 96% genetic homology with humans. Despite these characteristics, baboons have rarely been utilized as experimental models of human EBOV infection to evaluate the efficacy of prophylactics and therapeutics in the United States. This review will summarize what is known about the pathogenesis of EBOV infection in baboons compared to EBOV infection in humans and other Old World nonhuman primates. In addition, we will discuss how closely the baboon model recapitulates human EBOV infection. We will also review some of the housing requirements and behavioral attributes of baboons compared to other Old World nonhuman primates. Due to the lack of data available on the pathogenesis of Marburg virus (MARV) infection in baboons, discussion of the pathogenesis of MARV infection in baboons will be limited. -

Wnv-Case-Definition.Pdf
Draft Case Definition for West Nile Fever Animal and Plant Health Inspection Service West Nile Fever Veterinary Services October 2018 Case Definition (Notifiable) 1. Clinical Signs 1.1 Clinical Signs: West Nile Fever (WNF) is a zoonotic mosquito-borne viral disease caused by the West Nile virus (WNV), a Flavivirus of the family Flaviviridae. Many vertebrate species are susceptible to natural WNV infection; however, fatal neurological outbreaks have only been documented in equids, humans, geese, wild birds (particularly corvids), squirrels, farmed alligators, and dogs. Birds serve as the natural host reservoir of WNV. The incubation period is estimated to be three to 15 days in horses Ten to 39 percent of unvaccinated horses infected with WNV will develop clinical signs. Most clinically affected horses exhibit neurological signs such as ataxia (including stumbling, staggering, wobbly gait, or incoordination) or at least two of the following: circling, hind limb weakness, recumbency or inability to stand (or both), multiple limb paralysis, muscle fasciculation, proprioceptive deficits, altered mental status, blindness, lip droop/paralysis, teeth grinding. Behavioral changes including somnolence, listlessness, apprehension, or periods of hyperexcitability may occur. Other common clinical signs include colic, lameness, anorexia, and fever. 2. Laboratory criteria: 2.1 Agent isolation and identification: The virus can be identified by polymerase chain reaction (PCR) and virus isolation (VI). Preferred tissues from equids are brain or spinal cord. 2.2 Serology: Antibody titers can be identified in paired serum samples by IgM and IgG capture enzyme linked immunosorbent assay (ELISA), plaque reduction neutralization test (PRNT), and virus neutralization (VN). Only a single serum sample is required for IgM capture ELISA, and this is the preferred serologic test in live animals. -

The Hemorrhagic Fevers of Southern Africa South African Institute For
THE YALE JOURNAL OF BIOLOGY AND MEDICINE 55 (1982), 207-212 The Hemorrhagic Fevers of Southern Africa with Special Reference to Studies in the South African Institute for Medical Research J.H.S. GEAR, M.D. National Institute for Virology, Johannesburg, South Africa Received April 19, 1982 In this review of studies on the hemorrhagic fevers of Southern Africa carried out in the South African Institute for Medical Research, attention has been called to occurrence of meningococcal septicemia in recruits to the mining industry and South African Army, to cases of staphylococcal and streptococcal septicemia with hemorrhagic manifestations, and to the occurrence of plague which, in its septicemic form, may cause a hemorrhagic state. "Onyalai," a bleeding disease in tropical Africa, often fatal, was related to profound throm- bocytopenia possibly following administration of toxic witch doctor medicine. Spirochetal diseases, and rickettsial diseases in their severe forms, are often manifested with hemorrhagic complications. Of enterovirus infections, Coxsackie B viruses occasionally caused severe hepa- titis associated with bleeding, especially in newborn babies. Cases of hemorrhagic fever presenting in February-March, 1975 are described. The first out- break was due to Marburg virus disease and the second, which included seven fatal cases, was caused by Rift Valley fever virus. In recent cases of hemorrhagic fever a variety of infective organisms have been incriminated including bacterial infections, rickettsial diseases, and virus diseases, including Herpesvirus hominis; in one patient, the hemorrhagic state was related to rubella. A boy who died in a hemorrhagic state was found to have Congo fever; another pa- tient who died of severe bleeding from the lungs was infected with Leptospira canicola, and two patients who developed a hemorrhagic state after a safari trip in Northern Botswana were infected with Trypanosoma rhodesiense. -

Viral Hemorrhagic Fevers and Bioterrorism
What you need to know about . Viral Hemorrhagic Fevers and Bioterrorism What are viral hemorrhagic fevers? How are viral hemorrhagic fevers Viral hemorrhagic fevers (VHFs) are a spread? group of illnesses caused by several distinct In nature, viruses causing hemorrhagic fever families of viruses. In general the term typically are passed from mice, rats, fleas “viral hemorrhagic fever” describes severe and ticks to humans. People can be infected problems affecting several organ systems when they come in contact with urine, fecal in the body. Typically, the entire system of ma�er, saliva or other body fluids from blood vessels is damaged, and the body has infected rodents. Fleas and ticks transmit the problems regulating itself. Symptoms o�en viruses when they bite a person or when a include bleeding, but the bleeding itself is person crushes a tick. Hosts for some viruses rarely life-threatening. VHFs are caused by such as Ebola and Marburg are not known. viruses of four families: Some viruses such as Ebola, Marburg and Lassa can be spread from person to person • Arenavirus including Lassa fever and by direct contact with infected blood or Argentine, Bolivian, Brazilian and organs or indirectly through contact with Venezuelan hemorrhagic fevers; objects such as syringes or needles that are • Filovirus including Ebola and Marburg; contaminated with infected body fluids. • Bunyavirus including Hantavirus and Ri� Valley Fever; What are the symptoms? • Flavivirus including yellow fever and Symptoms vary with the different virus dengue fever. families, but first signs o�en include sudden fever, weakness, muscle pain, tiredness, Can viral hemorrhagic fevers be used headache and sore throat. -

Rift Valley Fever for Host Innate Immunity in Resistance to a New
A New Mouse Model Reveals a Critical Role for Host Innate Immunity in Resistance to Rift Valley Fever This information is current as Tânia Zaverucha do Valle, Agnès Billecocq, Laurent of September 25, 2021. Guillemot, Rudi Alberts, Céline Gommet, Robert Geffers, Kátia Calabrese, Klaus Schughart, Michèle Bouloy, Xavier Montagutelli and Jean-Jacques Panthier J Immunol 2010; 185:6146-6156; Prepublished online 11 October 2010; Downloaded from doi: 10.4049/jimmunol.1000949 http://www.jimmunol.org/content/185/10/6146 Supplementary http://www.jimmunol.org/content/suppl/2010/10/12/jimmunol.100094 http://www.jimmunol.org/ Material 9.DC1 References This article cites 46 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/185/10/6146.full#ref-list-1 Why The JI? Submit online. by guest on September 25, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American -
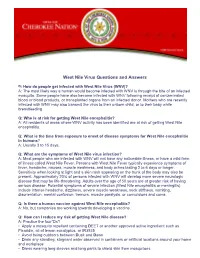
West Nile Virus Questions and Answers
West Nile Virus Questions and Answers Q: How do people get infected with West Nile Virus (WNV)? A: The most likely way a human would become infected with WNV is through the bite of an infected mosquito. Some people have also become infected with WNV following receipt of contaminated blood or blood products, or transplanted organs from an infected donor. Mothers who are recently infected with WNV may also transmit the virus to their unborn child, or to their baby while breastfeeding. Q: Who is at risk for getting West Nile encephalitis? A: All residents of areas where WNV activity has been identified are at risk of getting West Nile encephalitis. Q: What is the time from exposure to onset of disease symptoms for West Nile encephalitis in humans? A: Usually 3 to 15 days. Q: What are the symptoms of West Nile virus infection? A: Most people who are infected with WNV will not have any noticeable illness, or have a mild form of illness called West Nile Fever. Persons with West Nile Fever typically experience symptoms of fever, headache, nausea, muscle weakness, and body aches lasting 2 to 6 days or longer. Sensitivity when looking at light and a skin rash appearing on the trunk of the body may also be present. Approximately 20% of persons infected with WNV will develop more severe neurologic disease that may be life-threatening. Adults over the age of 50 years are at greater risk of having serious disease. Potential symptoms of severe infection (West Nile encephalitis or meningitis) include intense headache, dizziness, severe muscle weakness, neck stiffness, vomiting, disorientation, mental confusion, tremors, muscle paralysis, or convulsions and coma. -

Viral Hemorrhagic Fevers (Lassa, Marburg, Ebola, Crimean-Congo, and Other Emerging Viruses)
Viral Hemorrhagic Fevers (Lassa, Marburg, Ebola, Crimean-Congo, and other emerging viruses) What Are They? Viral hemorrhagic fevers are a group of illnesses causes by several viruses. These viruses affect multiple organs in the body by damaging the vascular (blood vessel) system. The bleeding or hemorrhaging caused by the virus is not usually life threatening but damage to organ systems in the body can range from mild to deadly. The viruses responsible for this type of illness include Lassa, Marburg, Ebola, and Crimean-Congo hemorrhagic fever. How can you get it? These emerging viral hemorrhagic fevers are presumed to be animal borne (zoonotic) and can be transmitted to humans through contact. Infected humans can spread the virus to each other through contact with contaminated objects or blood. The risk of acquiring these diseases is typically restricted to the geographic regions where the virus is found. Given global travel, rare cases have been reported outside of the host region. These rare cases are probably the greatest form of the occupational threat to fire fighters. Lassa Associated with specific rodents Found in West Africa Marburg Transmitted by African fruit bat Found in Africa Ebola Transmitted by unknown animal Found in Africa Crimean-Congo Tick-borne virus Found in Africa, Asia, Europe What are the symptoms? The time to develop symptoms varies by virus but is between 2 to 21 days after exposure to the Ebola virus. The signs and symptoms of viral hemorrhagic fever vary depending on the virus but include: Flu-like symptoms o Fever o Fatigue o Muscle aches Exhaustion Nausea and/or vomiting Abdominal pain Shock Seizures Delirium Bleeding Organ failure The most common complication of Lassa fever is deafness.