381.Full.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prestinłs Anion Transport and Voltage-Sensing Capabilities Are
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Biophysical Journal Volume 96 April 2009 3179–3186 3179 Prestin’s Anion Transport and Voltage-Sensing Capabilities Are Independent Jun-Ping Bai,† Alexei Surguchev,†‡ Simone Montoya,†‡ Peter S. Aronson,§{ Joseph Santos-Sacchi,‡{k and Dhasakumar Navaratnam†k* †Department of Neurology, ‡Division of Otolaryngology, Department of Surgery, §Department of Internal Medicine, {Department of Cellular and Molecular Physiology, and kDepartment of Neurobiology, Yale University School of Medicine, New Haven, Connecticut ABSTRACT The integral membrane protein prestin, a member of the SLC26 anion transporter family, is responsible for the voltage-driven electromotility of mammalian outer hair cells. It was argued that the evolution of prestin’s motor function required a loss of the protein’s transport capabilities. Instead, it was proposed that prestin manages only an abortive hemicycle that results in the trapped anion acting as a voltage sensor, to generate the motor’s signature gating charge movement or nonlinear capaci- tance. We demonstrate, using classical radioactive anion ([14C]formate and [14C]oxalate) uptake studies, that in contrast to previous observations, prestin is able to transport anions. The prestin-dependent uptake of both these anions was twofold that of cells transfected with vector alone, and comparable to SLC26a6, prestin’s closest phylogenetic relative. Furthermore, we identify a potential chloride-binding site in which the mutations of two residues (P328A and L326A) preserve nonlinear capacitance, yet negate anion transport. Finally, we distinguish 12 charged residues out of 22, residing within prestin’s transmembrane regions, that contribute to unitary charge movement, i.e., voltage sensing. -

Supporting Information
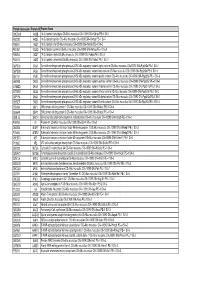
Supporting Information Table S1. List of confirmed SLC transporters represented in Canine GeneChip. SLC family Members detected Members not detected SLC1: The high affinity glutamate and neutral amino acid SLC1A1 SLC1A2, SLC1A3, SLC1A6 transporter family SLC2: The facilitative GLUT transporter family SLC2A1, SLC2A8 SLC2A3, SLC2A9 SLC3: The heavy subunits of the heteromeric amino acid SLC3A1 transporters SLC4: The bicarbonate transporter family SLC4A11 SLC4A4, SLC4A8 SLC5: The sodium glucose cotransporter family SLC5A6 SLC5A3, SLC5A10, SLC5A12 SLC6: The sodium- and chloride- dependent SLC6A6, SLC6A12 SLCA18 neurotransmitter transporter family SLC7: The cationic amino acid transporter/glycoprotein- NR associated family SLC8: The Na+/Ca2+ exchanger family SLC8A1 SLC9: The Na+/H+ exchanger family SLC9A1, SLC9A6, SLC9A9 SLC10: The sodium bile salt cotransport family SLC10A2 SLC11: The proton coupled metal ion transporter family NR SLC12: The electroneutral cation-Cl cotransporter family SLC12A3, SLC12A6, SLC12A8 SLC13: The human Na+-sulfate/carboxylate cotransporter SLC13A2 family SLC14: The urea transporter family NR SLC15: The proton oligopeptide cotransporter family SLC15A2, SLC15A4 SLC15A1 SLC16: The monocarboxylate transporter family SLC16A13 SLC16A4 SLC17: The vesicular glutamate transporter family SLC17A3, SLC17A7 SLC18: The vesicular amine transporter family NR SLC19: The folate/thiamine transporter family NR SLC20: The type III Na+-phosphate cotransporter family NR SLC21/SLCO: The organic anion transporting family SLC21A3, SLC21A8, -

RNA-Seq Reveals Conservation of Function Among the Yolk Sacs Of
RNA-seq reveals conservation of function among the PNAS PLUS yolk sacs of human, mouse, and chicken Tereza Cindrova-Daviesa, Eric Jauniauxb, Michael G. Elliota,c, Sungsam Gongd,e, Graham J. Burtona,1, and D. Stephen Charnock-Jonesa,d,e,1,2 aCentre for Trophoblast Research, Department of Physiology, Development and Neuroscience, University of Cambridge, Cambridge, CB2 3EG, United Kingdom; bElizabeth Garret Anderson Institute for Women’s Health, Faculty of Population Health Sciences, University College London, London, WC1E 6BT, United Kingdom; cSt. John’s College, University of Cambridge, Cambridge, CB2 1TP, United Kingdom; dDepartment of Obstetrics and Gynaecology, University of Cambridge, Cambridge, CB2 0SW, United Kingdom; and eNational Institute for Health Research, Cambridge Comprehensive Biomedical Research Centre, Cambridge, CB2 0QQ, United Kingdom Edited by R. Michael Roberts, University of Missouri-Columbia, Columbia, MO, and approved May 5, 2017 (received for review February 14, 2017) The yolk sac is phylogenetically the oldest of the extraembryonic yolk sac plays a critical role during organogenesis (3–5, 8–10), membranes. The human embryo retains a yolk sac, which goes there are limited data to support this claim. Obtaining experi- through primary and secondary phases of development, but its mental data for the human is impossible for ethical reasons, and importance is controversial. Although it is known to synthesize thus we adopted an alternative strategy. Here, we report RNA proteins, its transport functions are widely considered vestigial. sequencing (RNA-seq) data derived from human and murine yolk Here, we report RNA-sequencing (RNA-seq) data for the human sacs and compare them with published data from the yolk sac of and murine yolk sacs and compare those data with data for the the chicken. -

Autocrine IFN Signaling Inducing Profibrotic Fibroblast Responses By
Downloaded from http://www.jimmunol.org/ by guest on September 23, 2021 Inducing is online at: average * The Journal of Immunology , 11 of which you can access for free at: 2013; 191:2956-2966; Prepublished online 16 from submission to initial decision 4 weeks from acceptance to publication August 2013; doi: 10.4049/jimmunol.1300376 http://www.jimmunol.org/content/191/6/2956 A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Autocrine IFN Signaling Feng Fang, Kohtaro Ooka, Xiaoyong Sun, Ruchi Shah, Swati Bhattacharyya, Jun Wei and John Varga J Immunol cites 49 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2013/08/20/jimmunol.130037 6.DC1 This article http://www.jimmunol.org/content/191/6/2956.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2013 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 23, 2021. The Journal of Immunology A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Inducing Autocrine IFN Signaling Feng Fang,* Kohtaro Ooka,* Xiaoyong Sun,† Ruchi Shah,* Swati Bhattacharyya,* Jun Wei,* and John Varga* Activation of TLR3 by exogenous microbial ligands or endogenous injury-associated ligands leads to production of type I IFN. -

Temporal Profiling of Astrocyte Precursors Reveals Parallel Roles for Asef During Development and After Injury
11904 • The Journal of Neuroscience, November 23, 2016 • 36(47):11904–11917 Development/Plasticity/Repair Temporal Profiling of Astrocyte Precursors Reveals Parallel Roles for Asef during Development and after Injury Lesley S. Chaboub,1,2 Jeanne M. Manalo,2 XHyun Kyoung Lee,5 X Stacey M. Glasgow,2 XFengju Chen,4 Yoshihiro Kawasaki,6 Tetsu Akiyama,6 Chay T. Kuo,7 Chad J. Creighton,4,8 XCarrie A. Mohila,9 and Benjamin Deneen1,2,3,5 1Program in Developmental Biology, 2Center for Cell and Gene Therapy, 3Department of Neuroscience, and 4Dan L. Duncan Cancer Center, Division of Biostatistics, Baylor College of Medicine, Houston, Texas 77030, 5Jan and Dan Duncan Neurological Research Institute at Texas Children’s Hospital, Houston, Texas 77230, 6Laboratory of Molecular and Genetic Information, Institute for Molecular and Cellular Biosciences, University of Tokyo, Tokyo 113-0033, Japan, 7Department of Cell Biology, Duke University, Durham, North Carolina 27710, and 8Department of Medicine and 9Department of Pathology, Texas Children’s Hospital, Houston, Texas 77030 Lineage development is a stepwise process, governed by stage-specific regulatory factors and associated markers. Astrocytes are one of the principle cell types in the CNS and the stages associated with their development remain very poorly defined. To identify these stages, we performed gene-expression profiling on astrocyte precursor populations in the spinal cord, identifying distinct patterns of gene induction during their development that are strongly correlated with human astrocytes. Validation studies identified a new cohort of astrocyte-associated genes during development and demonstrated their expression in reactive astro- cytes in human white matter injury (WMI). -

The Fundamental Role of Bicarbonate Transporters and Associated Carbonic Anhydrase Enzymes in Maintaining Ion and Ph Homeostasis in Non-Secretory Organs
International Journal of Molecular Sciences Review The Fundamental Role of Bicarbonate Transporters and Associated Carbonic Anhydrase Enzymes in Maintaining Ion and pH Homeostasis in Non-Secretory Organs Dongun Lee and Jeong Hee Hong * Department of Physiology, Lee Gil Ya Cancer and Diabetes Institute, College of Medicine, Gachon University, Incheon 21999, Korea; [email protected] * Correspondence: [email protected]; Tel.: +82-32-899-6682; Fax: +82-32-899-6039 Received: 17 December 2019; Accepted: 3 January 2020; Published: 4 January 2020 Abstract: The bicarbonate ion has a fundamental role in vital systems. Impaired bicarbonate transport leads to various diseases, including immune disorders, cystic fibrosis, tumorigenesis, kidney diseases, brain dysfunction, tooth fracture, ischemic reperfusion injury, hypertension, impaired reproductive system, and systemic acidosis. Carbonic anhydrases are involved in the mechanism of bicarbonate movement and consist of complex of bicarbonate transport systems including bicarbonate transporters. This review focused on the convergent regulation of ion homeostasis through various ion transporters including bicarbonate transporters, their regulatory enzymes, such as carbonic anhydrases, pH regulatory role, and the expression pattern of ion transporters in non-secretory systems throughout the body. Understanding the correlation between these systems will be helpful in order to obtain new insights and design potential therapeutic strategies for the treatment of pH-related disorders. In this review, we have discussed the broad prospects and challenges that remain in elucidation of bicarbonate-transport-related biological and developmental systems. Keywords: bicarbonate; ion transporters; carbonic anhydrase; intracellular pH; maturation 1. Convergent Regulation of Ion Homeostasis Ion homeostasis is an important process involved in various organ functions, including modulation of sensitivity to blood pressure, immune cell differentiation, fluid secretion, and fertilization of reproductive cells such as sperm and eggs. -

Download Thesis
This electronic thesis or dissertation has been downloaded from the King’s Research Portal at https://kclpure.kcl.ac.uk/portal/ Investigations into the effects of berry flavonoids on nutrient transport processes in Caco-2 enterocytes Alzaid, Fawaz Awarding institution: King's College London The copyright of this thesis rests with the author and no quotation from it or information derived from it may be published without proper acknowledgement. END USER LICENCE AGREEMENT Unless another licence is stated on the immediately following page this work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International licence. https://creativecommons.org/licenses/by-nc-nd/4.0/ You are free to copy, distribute and transmit the work Under the following conditions: Attribution: You must attribute the work in the manner specified by the author (but not in any way that suggests that they endorse you or your use of the work). Non Commercial: You may not use this work for commercial purposes. No Derivative Works - You may not alter, transform, or build upon this work. Any of these conditions can be waived if you receive permission from the author. Your fair dealings and other rights are in no way affected by the above. Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 06. Oct. 2021 This electronic theses or dissertation has been downloaded from the King’s Research Portal at https://kclpure.kcl.ac.uk/portal/ Title: Investigations into the effects of berry flavonoids on nutrient transport processes in Caco-2 enterocytes Author: Fawaz Alzaid The copyright of this thesis rests with the author and no quotation from it or information derived from it may be published without proper acknowledgement. -

The Molecular Characterization and Expression of New Human SLC26 Anion Transporters Minna Kujala-Myllynen
Helsinki University Biomedical Dissertations No. 69 The Molecular Characterization and Expression of New Human SLC26 Anion Transporters Minna Kujala-Myllynen Department of Medical Genetics University of Helsinki Finland Academic dissertation To be publicly discussed with the permission of the Faculty of Medicine, University of Helsinki, in the large lecture hall of Haartman Institute, Haartmaninkatu 3, Helsinki, on November 18th 2005, at 12 noon. Supervised by: Juha Kere, Professor Department of Biosciences at Novum Karolinska Institute Stockholm, Sweden and Department of Medical Genetics University of Helsinki Helsinki, Finland Reviewed by: Hannu Jalanko, MD, PhD, Adjunct Professor Hospital for Children and Adolescents University of Helsinki Helsinki, Finland and Anne Räisänen-Sokolowski, MD, PhD, Adjunct Professor Department of Pathology University of Helsinki, and Helsinki University Central Hospital Helsinki, Finland Official opponent: Per-Henrik Groop, MD, DMSc, Adjunct Professor Folkhälsan Research Center University of Helsinki Helsinki, Finland ISSN 1457-8433 ISBN 952-10-2735-5 (paperback) ISBN 952-10-2736-3 (PDF) Yliopistopaino Helsinki 2005 To My Family Table of Contents List of Original Publications ................................................................................. 13 Abstract ................................................................................................................. 16 Introduction .......................................................................................................... -

Ncomms4622.Pdf
ARTICLE Received 23 Oct 2013 | Accepted 11 Mar 2014 | Published 8 Apr 2014 DOI: 10.1038/ncomms4622 OPEN Molecular architecture and the structural basis for anion interaction in prestin and SLC26 transporters Dmitry Gorbunov1,*, Mattia Sturlese2,*, Florian Nies1, Murielle Kluge1, Massimo Bellanda2, Roberto Battistutta2,3 & Dominik Oliver1 Prestin (SLC26A5) is a member of the SLC26/SulP anion transporter family. Its unique quasi-piezoelectric mechanical activity generates fast cellular motility of cochlear outer hair cells, a key process underlying active amplification in the mammalian ear. Despite its established physiological role, it is essentially unknown how prestin can generate mechanical force, since structural information on SLC26/SulP proteins is lacking. Here we derive a structural model of prestin and related transporters by combining homology modelling, MD simulations and cysteine accessibility scanning. Prestin’s transmembrane core region is organized in a 7 þ 7 inverted repeat architecture. The model suggests a central cavity as the substrate-binding site located midway of the anion permeation pathway, which is supported by experimental solute accessibility and mutational analysis. Anion binding to this site also controls the electromotile activity of prestin. The combined structural and functional data provide a framework for understanding electromotility and anion transport by SLC26 transporters. 1 Department of Neurophysiology, Institute of Physiology and Pathophysiology, Philipps University, 35037 Marburg, Germany. 2 Department of Chemical Sciences, University of Padua, via Marzolo 1, Padova 35131, Italy. 3 Venetian Institute for Molecular Medicine (VIMM), via Orus 2, Padova 35129, Italy. * These authors contributed equally. Correspondence and requests for materials should be addressed to D.O. (email: [email protected]). -

Expression of Ion Transport-Associated Proteins in Human Efferent and Epididymal Ducts
REPRODUCTIONRESEARCH Expression of ion transport-associated proteins in human efferent and epididymal ducts Minna Kujala1,2, Satu Hihnala1,3, Jukka Tienari4, Kari Kaunisto5, Johanna Ha¨stbacka1,3, Christer Holmberg3, Juha Kere1,6 and Pia Ho¨glund1,3 1Department of Medical Genetics, University of Helsinki, Helsinki, Finland, 2Helsinki University Central Hospital Laboratory Division, Helsinki, Finland, 3Hospital for Children and Adolescents, University of Helsinki, Helsinki, Finland, 4Department of Pathology, Helsinki University Central Hospital/Peijas Hospital and HUSLAB, Vantaa, Finland, 5Departments of Anatomy and Cell Biology and Pediatrics, University of Oulu, Oulu, Finland and 6Department of Biosciences at Novum, Karolinska Institute, Stockholm, Sweden Correspondence should be addressed to M Kujala, Department of Medical Genetics, POB 63, 00014 University of Helsinki, Finland; Email: minna.kujala@helsinki.fi Abstract Appropriate intraluminal microenvironment in the epididymis is essential for maturation of sperm. To clarify whether the anion transporters SLC26A2, SLC26A6, SLC26A7, and SLC26A8 might participate in generating this proper intraluminal milieu, we studied the localization of these proteins in the human efferent and the epididymal ducts by immunohistochemistry. In addition, C C K immunohistochemistry of several SLC26-interacting proteins was performed: the Na /H exchanger 3 (NHE3), the Cl channel C C cystic fibrosis transmembrane conductance regulator (CFTR), the proton pump V-ATPase, their regulator Na /H exchanger regulating factor 1 (NHERF-1), and carbonic anhydrase II (CAII). Our results show that SLC26A6, CFTR, NHE3, and NHERF-1 are co-expressed on the apical side of the nonciliated cells, and SLC26A2 appears in the cilia of the ciliated cells in the human efferent ducts. In the epididymal ducts, SLC26A6, CFTR, NHERF-1, CAII, and V-ATPase (B and E subunits) were co-localized to the apical mitochondria rich cells, while SLC26A7 was expressed in a subgroup of basal cells. -

D-Serine, an Emerging Biomarker of Kidney Diseases, Is a Hidden Substrate of Sodium-Coupled Monocarboxylate Transporters
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.10.244822; this version posted August 10, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Wiriyasermkul, et al. 1 D-Serine, an emerging biomarker of kidney diseases, is a hidden substrate of 2 sodium-coupled monocarboxylate transporters 3 4 Pattama Wiriyasermkul1, Satomi Moriyama1, Yoko Tanaka1, Pornparn Kongpracha1, Nodoka 5 Nakamae1, Masataka Suzuki2, Tomonori Kimura3,4, Masashi Mita5, Jumpei Sasabe2, Shushi 6 Nagamori1,# 7 8 1Department of Collaborative Research for Biomolecular Dynamics, Nara Medical 9 University, Nara, Japan 10 2Department of Pharmacology, Keio University School of Medicine, Tokyo, Japan 11 3KAGAMI Project, 4Reverse Translational Research Project, Center for Rare Disease 12 Research, National Institutes of Biomedical Innovation, Health and Nutrition (NIBIOHN). 13 Osaka, Japan 14 5KAGAMI Inc., Osaka, Japan 15 16 # Corresponding contact information: [email protected] 17 18 19 20 21 Keywords: transporter, proteome, ischemia-reperfusion injury (IRI), acute kidney injury 22 (AKI), chronic kidney diseases (CKD), membrane 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.10.244822; this version posted August 10, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Wiriyasermkul, et al. 23 Abstract 24 Delay in diagnosis of renal injury has profound impacts on morbidity and mortality. -
Protein List (6009)
Protein Accession Protein Id Protein Name Q9CQV8 1433B 14-3-3 protein beta/alpha OS=Mus musculus OX=10090 GN=Ywhab PE=1 SV=3 P62259 1433E 14-3-3 protein epsilon OS=Mus musculus OX=10090 GN=Ywhae PE=1 SV=1 P68510 1433F 14-3-3 protein eta OS=Mus musculus OX=10090 GN=Ywhah PE=1 SV=2 P61982 1433G 14-3-3 protein gamma OS=Mus musculus OX=10090 GN=Ywhag PE=1 SV=2 P68254 1433T 14-3-3 protein theta OS=Mus musculus OX=10090 GN=Ywhaq PE=1 SV=1 P63101 1433Z 14-3-3 protein zeta/delta OS=Mus musculus OX=10090 GN=Ywhaz PE=1 SV=1 Q6PD03 2A5A Serine/threonine-protein phosphatase 2A 56 kDa regulatory subunit alpha isoform OS=Mus musculus OX=10090 GN=Ppp2r5a PE=1 SV=1 Q6PD28 2A5B Serine/threonine-protein phosphatase 2A 56 kDa regulatory subunit beta isoform OS=Mus musculus OX=10090 GN=Ppp2r5b PE=1 SV=1 Q61151 2A5E Serine/threonine-protein phosphatase 2A 56 kDa regulatory subunit epsilon isoform OS=Mus musculus OX=10090 GN=Ppp2r5e PE=1 SV=3 Q60996 2A5G Serine/threonine-protein phosphatase 2A 56 kDa regulatory subunit gamma isoform OS=Mus musculus OX=10090 GN=Ppp2r5c PE=1 SV=2 Q76MZ3 2AAA Serine/threonine-protein phosphatase 2A 65 kDa regulatory subunit A alpha isoform OS=Mus musculus OX=10090 GN=Ppp2r1a PE=1 SV=3 Q7TNP2 2AAB Serine/threonine-protein phosphatase 2A 65 kDa regulatory subunit A beta isoform OS=Mus musculus OX=10090 GN=Ppp2r1b PE=1 SV=2 Q6P1F6 2ABA Serine/threonine-protein phosphatase 2A 55 kDa regulatory subunit B alpha isoform OS=Mus musculus OX=10090 GN=Ppp2r2a PE=1 SV=1 Q925E7 2ABD Serine/threonine-protein phosphatase 2A 55 kDa regulatory subunit B delta isoform OS=Mus musculus OX=10090 GN=Ppp2r2d PE=1 SV=1 P55194 3BP1 SH3 domain-binding protein 1 OS=Mus musculus OX=10090 GN=Sh3bp1 PE=1 SV=3 Q06649 3BP2 SH3 domain-binding protein 2 OS=Mus musculus OX=10090 GN=Sh3bp2 PE=1 SV=1 Q99L13 3HIDH 3-hydroxyisobutyrate dehydrogenase, mitochondrial OS=Mus musculus OX=10090 GN=Hibadh PE=1 SV=1 P48193 41 Protein 4.