《 Appendix 》 Code No
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

In Vitro Differentiation of Bone Marrow Mesenchymal Stem Cells Into Endometrial Epithelial Cells in Mouse: a Proteomic Analysis
Int J Clin Exp Pathol 2014;7(7):3662-3672 www.ijcep.com /ISSN:1936-2625/IJCEP0000322 Original Article In vitro differentiation of bone marrow mesenchymal stem cells into endometrial epithelial cells in mouse: a proteomic analysis Qing Cong1,2, Bin Li1,2, Yisheng Wang1,2, Wenbi Zhang1,2, Mingjun Cheng1,2, Zhiyong Wu1,2, Xiaoyan Zhang1,2, Wei Jiang1,2, Congjian Xu1,2,3,4 1Obstetrics and Gynecology Hospital of Fudan University, 2Shanghai Key Laboratory of Female Reproductive Endocrine Related Diseases, 3Department of Obstetrics and Gynecology of Shanghai Medical School, 4Institute of Biomedical Sciences, Fudan University, Shanghai, P.R. China Received March 24, 2014; Accepted June 23, 2014; Epub June 15, 2014; Published July 1, 2014 Abstract: Objective: Mouse bone marrow mesenchymal stem cells (BMSCs) have been demonstrated to differenti- ate into female endometrial epithelial cells (EECs) in vivo. Our previous studies demonstrated that BMSCs can differentiate in the direction of EECs when co-cultured with endometrial stromal cells in vitro. Here, we obtain and analyse differential proteins and their relevant pathways in the process of BMSCs differentiating into EECs by iso- baric tags for relative and absolute quantitation (iTRAQ) proteomic analysis. Methods: A 0.4-µm pore size indirect co- culture system was established with female mice endometrial stromal cells (EStCs) restricted in the upper Transwell chamber and BMSCs in the lower well plate. After indirect co-culture for several days, the BMSCs were revealed to progressively differentiate towards EECs in vitro. Then, four groups were divided according to different co-culture days with single culture groups of BMSCs as controls. -

Table S1 the Four Gene Sets Derived from Gene Expression Profiles of Escs and Differentiated Cells
Table S1 The four gene sets derived from gene expression profiles of ESCs and differentiated cells Uniform High Uniform Low ES Up ES Down EntrezID GeneSymbol EntrezID GeneSymbol EntrezID GeneSymbol EntrezID GeneSymbol 269261 Rpl12 11354 Abpa 68239 Krt42 15132 Hbb-bh1 67891 Rpl4 11537 Cfd 26380 Esrrb 15126 Hba-x 55949 Eef1b2 11698 Ambn 73703 Dppa2 15111 Hand2 18148 Npm1 11730 Ang3 67374 Jam2 65255 Asb4 67427 Rps20 11731 Ang2 22702 Zfp42 17292 Mesp1 15481 Hspa8 11807 Apoa2 58865 Tdh 19737 Rgs5 100041686 LOC100041686 11814 Apoc3 26388 Ifi202b 225518 Prdm6 11983 Atpif1 11945 Atp4b 11614 Nr0b1 20378 Frzb 19241 Tmsb4x 12007 Azgp1 76815 Calcoco2 12767 Cxcr4 20116 Rps8 12044 Bcl2a1a 219132 D14Ertd668e 103889 Hoxb2 20103 Rps5 12047 Bcl2a1d 381411 Gm1967 17701 Msx1 14694 Gnb2l1 12049 Bcl2l10 20899 Stra8 23796 Aplnr 19941 Rpl26 12096 Bglap1 78625 1700061G19Rik 12627 Cfc1 12070 Ngfrap1 12097 Bglap2 21816 Tgm1 12622 Cer1 19989 Rpl7 12267 C3ar1 67405 Nts 21385 Tbx2 19896 Rpl10a 12279 C9 435337 EG435337 56720 Tdo2 20044 Rps14 12391 Cav3 545913 Zscan4d 16869 Lhx1 19175 Psmb6 12409 Cbr2 244448 Triml1 22253 Unc5c 22627 Ywhae 12477 Ctla4 69134 2200001I15Rik 14174 Fgf3 19951 Rpl32 12523 Cd84 66065 Hsd17b14 16542 Kdr 66152 1110020P15Rik 12524 Cd86 81879 Tcfcp2l1 15122 Hba-a1 66489 Rpl35 12640 Cga 17907 Mylpf 15414 Hoxb6 15519 Hsp90aa1 12642 Ch25h 26424 Nr5a2 210530 Leprel1 66483 Rpl36al 12655 Chi3l3 83560 Tex14 12338 Capn6 27370 Rps26 12796 Camp 17450 Morc1 20671 Sox17 66576 Uqcrh 12869 Cox8b 79455 Pdcl2 20613 Snai1 22154 Tubb5 12959 Cryba4 231821 Centa1 17897 -

Regulation of Skeletal Muscle Glucose Transport and Glucose Metabolism by Exercise Training
nutrients Review Regulation of Skeletal Muscle Glucose Transport and Glucose Metabolism by Exercise Training Parker L. Evans 1,2,3, Shawna L. McMillin 1,2,3 , Luke A. Weyrauch 1,2,3 and Carol A. Witczak 1,2,3,4,* 1 Department of Kinesiology, East Carolina University, Greenville, NC 27858, USA; [email protected] (P.L.E.); [email protected] (S.L.M.); [email protected] (L.A.W.) 2 Department of Physiology, Brody School of Medicine, East Carolina University, Greenville, NC 27834, USA 3 East Carolina Diabetes & Obesity Institute, East Carolina University, Greenville, NC 27834, USA 4 Department of Biochemistry & Molecular Biology, Brody School of Medicine, East Carolina University, Greenville, NC 27834, USA * Correspondence: [email protected]; Tel.: +1-252-744-1224 Received: 8 September 2019; Accepted: 8 October 2019; Published: 12 October 2019 Abstract: Aerobic exercise training and resistance exercise training are both well-known for their ability to improve human health; especially in individuals with type 2 diabetes. However, there are critical differences between these two main forms of exercise training and the adaptations that they induce in the body that may account for their beneficial effects. This article reviews the literature and highlights key gaps in our current understanding of the effects of aerobic and resistance exercise training on the regulation of systemic glucose homeostasis, skeletal muscle glucose transport and skeletal muscle glucose metabolism. Keywords: aerobic exercise; blood glucose; functional overload; GLUT; hexokinase; insulin resistance; resistance exercise; SGLT; type 2 diabetes; weightlifting 1. Introduction Exercise training is defined as planned bouts of physical activity which repeatedly occur over a duration of time lasting from weeks to years. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Gene Expression Patterns and Tumor Uptake of 18F-FDG, 18F-FLT, and 18F-FEC in PET/MRI of an Orthotopic Mouse Xenotransplantation Model of Pancreatic Cancer
Journal of Nuclear Medicine, published on July 16, 2008 as doi:10.2967/jnumed.107.050021 Gene Expression Patterns and Tumor Uptake of 18F-FDG, 18F-FLT, and 18F-FEC in PET/MRI of an Orthotopic Mouse Xenotransplantation Model of Pancreatic Cancer Corinna von Forstner*1, Jan-Hendrik Egberts*2, Ole Ammerpohl2, Dagmara Niedzielska3, Ralph Buchert3, Pal Mikecz3, Udo Schumacher4, Kersten Peldschus5, Gerhard Adam5, Christian Pilarsky6, Robert Grutzmann6, Holger Kalthoff2, Eberhard Henze1, and Winfried Brenner3 1Department of Nuclear Medicine, University Hospital of Schleswig-Holstein, Campus Kiel, Kiel, Germany; 2Department of General Surgery and Thoracic Surgery, University Hospital of Schleswig-Holstein, Campus Kiel, Kiel, Germany; 3Department of Nuclear Medicine, University Medical Center Hamburg-Eppendorf, Hamburg, Germany; 4Department of Anatomy II Experimental Morphology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany; 5Department of Diagnostic and Interventional Radiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany; and 6Department of Visceral, Thoracic, and Vascular Surgery, University Hospital Carl Gustav Carus, Technical University of Dresden, Dresden, Germany the highest and most consistent uptake in various human pan- Our aim was to use PET/MRI to evaluate and compare the uptake creatic tumor cell lines in SCID mice. The imaging results could of 18F-FDG, 3-deoxy-3-18F-fluorothymidine (18F-FLT), and 18F- be explained by gene expression patterns of membrane trans- fluorethylcholine (18F-FEC) in human pancreatic tumor cell lines porters and enzymes for tracer uptake and retention as mea- after xenotransplantation into SCID mice and to correlate tumor sured by gene array analysis and quantitative polymerase uptake with gene expression of membrane transporters and chain reaction in the respective cell lines. -

Protein Identities in Evs Isolated from U87-MG GBM Cells As Determined by NG LC-MS/MS
Protein identities in EVs isolated from U87-MG GBM cells as determined by NG LC-MS/MS. No. Accession Description Σ Coverage Σ# Proteins Σ# Unique Peptides Σ# Peptides Σ# PSMs # AAs MW [kDa] calc. pI 1 A8MS94 Putative golgin subfamily A member 2-like protein 5 OS=Homo sapiens PE=5 SV=2 - [GG2L5_HUMAN] 100 1 1 7 88 110 12,03704523 5,681152344 2 P60660 Myosin light polypeptide 6 OS=Homo sapiens GN=MYL6 PE=1 SV=2 - [MYL6_HUMAN] 100 3 5 17 173 151 16,91913397 4,652832031 3 Q6ZYL4 General transcription factor IIH subunit 5 OS=Homo sapiens GN=GTF2H5 PE=1 SV=1 - [TF2H5_HUMAN] 98,59 1 1 4 13 71 8,048185945 4,652832031 4 P60709 Actin, cytoplasmic 1 OS=Homo sapiens GN=ACTB PE=1 SV=1 - [ACTB_HUMAN] 97,6 5 5 35 917 375 41,70973209 5,478027344 5 P13489 Ribonuclease inhibitor OS=Homo sapiens GN=RNH1 PE=1 SV=2 - [RINI_HUMAN] 96,75 1 12 37 173 461 49,94108966 4,817871094 6 P09382 Galectin-1 OS=Homo sapiens GN=LGALS1 PE=1 SV=2 - [LEG1_HUMAN] 96,3 1 7 14 283 135 14,70620005 5,503417969 7 P60174 Triosephosphate isomerase OS=Homo sapiens GN=TPI1 PE=1 SV=3 - [TPIS_HUMAN] 95,1 3 16 25 375 286 30,77169764 5,922363281 8 P04406 Glyceraldehyde-3-phosphate dehydrogenase OS=Homo sapiens GN=GAPDH PE=1 SV=3 - [G3P_HUMAN] 94,63 2 13 31 509 335 36,03039959 8,455566406 9 Q15185 Prostaglandin E synthase 3 OS=Homo sapiens GN=PTGES3 PE=1 SV=1 - [TEBP_HUMAN] 93,13 1 5 12 74 160 18,68541938 4,538574219 10 P09417 Dihydropteridine reductase OS=Homo sapiens GN=QDPR PE=1 SV=2 - [DHPR_HUMAN] 93,03 1 1 17 69 244 25,77302971 7,371582031 11 P01911 HLA class II histocompatibility antigen, -

Differential Expression of Hydroxyurea Transporters in Normal and Polycythemia Vera Hematopoietic Stem and Progenitor Cell Subpopulations
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2021 Differential expression of hydroxyurea transporters in normal and polycythemia vera hematopoietic stem and progenitor cell subpopulations Tan, Ge ; Meier-Abt, Fabienne Abstract: Polycythemia vera (PV) is a myeloproliferative neoplasm marked by hyperproliferation of the myeloid lineages and the presence of an activating JAK2 mutation. Hydroxyurea (HU) is a standard treat- ment for high-risk patients with PV. Because disease-driving mechanisms are thought to arise in PV stem cells, effective treatments should target primarily the stem cell compartment. We tested for theantipro- liferative effect of patient treatment with HU in fluorescence-activated cell sorting-isolated hematopoietic stem/multipotent progenitor cells (HSC/MPPs) and more committed erythroid progenitors (common myeloid/megakaryocyte-erythrocyte progenitors [CMP/MEPs]) in PV using RNA-sequencing and gene set enrichment analysis. HU treatment led to significant downregulation of gene sets associated with cell proliferation in PV HSCs/MPPs, but not in PV CMP/MEPs. To explore the mechanism underlying this finding, we assessed for expression of solute carrier membrane transporters, which mediate trans- membrane movement of drugs such as HU into target cells. The active HU uptake transporter OCTN1 was upregulated in HSC/MPPs compared with CMP/MEPs of untreated patients with PV, and the HU diffusion facilitator urea transporter B (UTB) was downregulated in HSC/MPPs compared withCM- P/MEPs in all patient and control groups tested. These findings indicate a higher accumulation ofHU within PV HSC/MPPs compared with PV CMP/MEPs and provide an explanation for the differential effects of HU in HSC/MPPs and CMP/MEPs of patients with PV. -
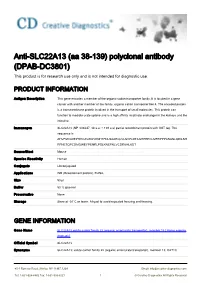
Anti-SLC22A13 (Aa 38-139) Polyclonal Antibody (DPAB-DC3801) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-SLC22A13 (aa 38-139) polyclonal antibody (DPAB-DC3801) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description This gene encodes a member of the organic-cation transporter family. It is located in a gene cluster with another member of the family, organic cation transporter like 4. The encoded protein is a transmembrane protein involved in the transport of small molecules. This protein can function to mediate urate uptake and is a high affinity nicotinate exchanger in the kidneys and the intestine. Immunogen SLC22A13 (NP_004247, 38 a.a. ~ 139 a.a) partial recombinant protein with GST tag. The sequence is AHVFMVLDEPHHCAVAWVKNHTFNLSAAEQLVLSVPLDTAGHPEPCLMFRPPPANASLQDILSH RFNETQPCDMGWEYPENRLPSLKNEFNLVCDRKHLKDT Source/Host Mouse Species Reactivity Human Conjugate Unconjugated Applications WB (Recombinant protein), ELISA, Size 50 μl Buffer 50 % glycerol Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. GENE INFORMATION Gene Name SLC22A13 solute carrier family 22 (organic anion/urate transporter), member 13 [ Homo sapiens (human) ] Official Symbol SLC22A13 Synonyms SLC22A13; solute carrier family 22 (organic anion/urate transporter), member 13; OAT10; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved OCTL1; OCTL3; ORCTL3; ORCTL-3; solute carrier family 22 member 13; organic cation transporter-like 3; organic-cation transporter like 3; organic cationic transporter-like 3; solute carrier family 22, member 13; solute carrier family 22 (organic anion transporter), member 13; Entrez Gene ID 9390 Protein Refseq NP_004247 UniProt ID Q9Y226 Chromosome Location 3p21.3 Function nicotinate transporter activity; organic cation transmembrane transporter activity; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 2 © Creative Diagnostics All Rights Reserved. -

The Concise Guide to Pharmacology 2019/20
Edinburgh Research Explorer THE CONCISE GUIDE TO PHARMACOLOGY 2019/20 Citation for published version: Cgtp Collaborators 2019, 'THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Transporters', British Journal of Pharmacology, vol. 176 Suppl 1, pp. S397-S493. https://doi.org/10.1111/bph.14753 Digital Object Identifier (DOI): 10.1111/bph.14753 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: British Journal of Pharmacology General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 28. Sep. 2021 S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2019/20: Transporters. British Journal of Pharmacology (2019) 176, S397–S493 THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Transporters Stephen PH Alexander1 , Eamonn Kelly2, Alistair Mathie3 ,JohnAPeters4 , Emma L Veale3 , Jane F Armstrong5 , Elena Faccenda5 ,SimonDHarding5 ,AdamJPawson5 , Joanna L -

(HMGB1) Deletion Leads to Small Heart and Glycolipid Metabolic
Yu et al. Cell Death Discovery (2020) 6:106 https://doi.org/10.1038/s41420-020-00340-9 Cell Death Discovery ARTICLE Open Access Cardiomyocyte-restricted high-mobility group box 1 (HMGB1) deletion leads to small heart and glycolipid metabolic disorder through GR/PGC-1α signalling Peng Yu 1, Ming Liu2,BaoliZhang3,YingYu2,EnyongSu3,ShiyaoXie3,LeiZhang3,XueYang3,HongJiang 3, Ruizhen Chen3, Yunzeng Zou3 and Junbo Ge3 Abstract Cardiac growth and remodelling are key biological processes influencing the physiological performance of the heart, and a previous study showed a critical role for intracellular HMGB1 in vitro. However, the in vivo study, which used conditional Hmgb1 ablation, did not show a significant effect on cellular or organic function. We have demonstrated the extracellular effect of HMGB1 as a pro-inflammatory molecule on cardiac remodelling. In this study, we found that HMGB1 deletion by cTnT-Cre in mouse hearts altered glucocorticoid receptor (GR) function and glycolipid metabolism, eventually leading to growth retardation, small heart and heart failure. The subcellular morphology did not show a significant change caused by HMGB1 knockout. The heart showed significant elevation of glycolysis, free fatty acid deposition and related enzyme changes. Transcriptomic analysis revealed a list of differentially expressed genes that coincide with glucocorticoid receptor function in neonatal mice and a significant increase in inflammatory genes in 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; adult mice. Cardiac HMGB1 knockout led to a series of changes in PGC-1α, UCP3 and GyK, which were the cause of metabolic changes and further impacted cardiac function. Ckmm-Cre Hmgb1fl/fl mice did not show a specific phenotype, which was consistent with the reported negative result of cardiomyocyte-specific Hmgb1 deletion via MHC-Cre. -

Towards the Elucidation of Orphan Lysosomal Transporters Quentin Verdon
Towards the Elucidation of Orphan Lysosomal Transporters Quentin Verdon To cite this version: Quentin Verdon. Towards the Elucidation of Orphan Lysosomal Transporters. Cancer. Université Paris Saclay (COmUE), 2016. English. NNT : 2016SACLS144. tel-01827233 HAL Id: tel-01827233 https://tel.archives-ouvertes.fr/tel-01827233 Submitted on 2 Jul 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. NNT : 2016SACLS144 THESE DE DOCTORAT DE L’UNIVERSITE PARIS-SACLAY PREPAREE A L’UNIVERSITE PARIS-SUD ECOLE DOCTORALE N°568 BIOSIGNE | Signalisations et réseaux intégratifs en biologie Spécialité de doctorat : aspects moléculaires et cellulaires de la biologie Par Mr Quentin Verdon Towards the elucidation of orphan lysosomal transporters: several shots on target and one goal Thèse présentée et soutenue à Paris le 29/06/2016 » : Composition du Jury : Mr Le Maire Marc Professeur, Université Paris-Sud Président Mr Birman Serge Directeur de recherche, CNRS Rapporteur Mr Murray James Assistant professor, Trinity college Dublin Rapporteur Mr Goud Bruno Directeur de recherche, CNRS Examinateur Mr Gasnier Bruno Directeur de recherche, CNRS Directeur de thèse Mme Sagné Corinne Chargée de recherche, INSERM Co-directeur de thèse Table of contents Remerciements (acknowledgements) 6 Abbreviations 7 Abstracts 10 Introduction 12 1 Physiology of lysosomes 12 1.1 Discovery and generalities 12 1.2 Degradative function 13 1.3. -

Expression of SLC2A9 Isoforms in the Kidney and Their Localization in Polarized Epithelial Cells
Expression of SLC2A9 Isoforms in the Kidney and Their Localization in Polarized Epithelial Cells Toru Kimura1, Michi Takahashi1, Kunimasa Yan2, Hiroyuki Sakurai1* 1 Department of Pharmacology and Toxicology, Kyorin University School of Medicine, Mitaka, Tokyo, Japan, 2 Department of Pediatrics, Kyorin University School of Medicine, Mitaka, Tokyo, Japan Abstract Background: Many genome-wide association studies pointed out that SLC2A9 gene, which encodes a voltage-driven urate transporter, SLC2A9/GLUT9 (a.k.a. URATv1), as one of the most influential genes for serum urate levels. SLC2A9 is reported to encode two splice variants: SLC2A9-S (512 amino acids) and SLC2A9-L (540 amino acids), only difference being at their N- termini. We investigated isoform-specific localization of SLC2A9 in the human kidney and role of N-terminal amino acids in differential sorting in vitro. Methodology/Principal Findings: Isoform specific antibodies against SLC2A9 were developed and human kidney sections were stained. SLC2A9-S was expressed in the apical side of the collecting duct while SLC2A9-L was expressed in the basolateral side of the proximal tubule. GFP fused SLC2A9s were expressed in MDCK cells and intracellular localization was observed. SLC2A9-S was expressed at both apical and basolateral membranes, whereas SLC2A9-L was expressed only at the basolateral membrane. Although SLC2A9-L has a putative di-leucine motif at 33th and 34th leucine, deletion of the motif or replacement of leucine did not affect its subcellular localization. When up to 16 amino acids were removed from the N- terminal of SLC2A9-S or when up to 25 amino acids were removed from the N-terminal of SLC2A9-L, there was no change in their sorting.