HOOVER-THESIS-2016.Pdf (6.708Mb)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Np63 Activates the Fanconi Anemia DNA Repair Pathway and Limits the Efficacy of Cisplatin Treatment in Squamous Cell Carcinoma Anne Catherine Bretz1, Miriam P
3204–3218 Nucleic Acids Research, 2016, Vol. 44, No. 7 Published online 26 January 2016 doi: 10.1093/nar/gkw036 Np63 activates the Fanconi anemia DNA repair pathway and limits the efficacy of cisplatin treatment in squamous cell carcinoma Anne Catherine Bretz1, Miriam P. Gittler1,Joel¨ P. Charles1, Niklas Gremke1, Ines Eckhardt1, Marco Mernberger1, Robert Mandic2,Jurgen¨ Thomale3, Andrea Nist4, Michael Wanzel1,5 and Thorsten Stiewe1,4,5,* 1Institute of Molecular Oncology, Philipps-University Marburg, 35043 Marburg, Germany, 2Department of Otorhinolaryngology, Head & Neck Surgery, University Hospital Giessen and Marburg, Philipps-University, 35033 Marburg, Germany, 3Institute of Cell Biology, University Duisburg-Essen, 45122 Essen, Germany, 4Genomics Core Facility, Philipps-University Marburg, 35043 Marburg, Germany and 5Universities of Giessen and Marburg Lung Center, member of the German Center for Lung Research (DZL), 35043 Marburg, Germany Received September 03, 2015; Revised December 18, 2015; Accepted January 12, 2016 ABSTRACT INTRODUCTION TP63, a member of the p53 gene family gene, encodes Squamous cell carcinoma (SCC) is a common and lethal the Np63 protein and is one of the most frequently human cancer, and relatively little progress has been made amplified genes in squamous cell carcinomas (SCC) in improving outcomes for SCC due to a poor understand- of the head and neck (HNSCC) and lungs (LUSC). ing of its underlying molecular pathogenesis (1,2). While Using an epiallelic series of siRNAs with intrinsically SCCs typically lack somatic oncogene-activating mutations, they exhibit frequent amplification of the p53 gene fam- different knockdown abilities, we show that the com- ily member TP63 (1–6). Recent tumor genome sequencing plete loss of Np63 strongly impaired cell prolifera- studies have revealed TP63 amplification in 20–25% of head tion, whereas partial Np63 depletion rendered cells and neck SCC (HNSCC) and 25–50% of lung SCC (LUSC) hypersensitive to cisplatin accompanied by an ac- (4,6). -

Viewed Under 23 (B) Or 203 (C) fi M M Male Cko Mice, and Largely Unaffected Magni Cation; Scale Bars, 500 M (B) and 50 M (C)
BRIEF COMMUNICATION www.jasn.org Renal Fanconi Syndrome and Hypophosphatemic Rickets in the Absence of Xenotropic and Polytropic Retroviral Receptor in the Nephron Camille Ansermet,* Matthias B. Moor,* Gabriel Centeno,* Muriel Auberson,* † † ‡ Dorothy Zhang Hu, Roland Baron, Svetlana Nikolaeva,* Barbara Haenzi,* | Natalya Katanaeva,* Ivan Gautschi,* Vladimir Katanaev,*§ Samuel Rotman, Robert Koesters,¶ †† Laurent Schild,* Sylvain Pradervand,** Olivier Bonny,* and Dmitri Firsov* BRIEF COMMUNICATION *Department of Pharmacology and Toxicology and **Genomic Technologies Facility, University of Lausanne, Lausanne, Switzerland; †Department of Oral Medicine, Infection, and Immunity, Harvard School of Dental Medicine, Boston, Massachusetts; ‡Institute of Evolutionary Physiology and Biochemistry, St. Petersburg, Russia; §School of Biomedicine, Far Eastern Federal University, Vladivostok, Russia; |Services of Pathology and ††Nephrology, Department of Medicine, University Hospital of Lausanne, Lausanne, Switzerland; and ¶Université Pierre et Marie Curie, Paris, France ABSTRACT Tight control of extracellular and intracellular inorganic phosphate (Pi) levels is crit- leaves.4 Most recently, Legati et al. have ical to most biochemical and physiologic processes. Urinary Pi is freely filtered at the shown an association between genetic kidney glomerulus and is reabsorbed in the renal tubule by the action of the apical polymorphisms in Xpr1 and primary fa- sodium-dependent phosphate transporters, NaPi-IIa/NaPi-IIc/Pit2. However, the milial brain calcification disorder.5 How- molecular identity of the protein(s) participating in the basolateral Pi efflux remains ever, the role of XPR1 in the maintenance unknown. Evidence has suggested that xenotropic and polytropic retroviral recep- of Pi homeostasis remains unknown. Here, tor 1 (XPR1) might be involved in this process. Here, we show that conditional in- we addressed this issue in mice deficient for activation of Xpr1 in the renal tubule in mice resulted in impaired renal Pi Xpr1 in the nephron. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

It Was Hypothesized That Hybrid Synthetic/Adenoviral Nanoparticles
Electronic Supplementary Material (ESI) for Nanoscale. This journal is © The Royal Society of Chemistry 2020 SUPPORTING INFORMATION Lana Papafilippou,a Andrew Claxton,b Paul Dark,b,c Kostas Kostarelos*a,d and Marilena Hadjidemetriou*a aNanomedicine Lab, Faculty of Biology, Medicine & Health, AV Hill Building, The University of Manchester, Manchester, M13 9PT, UK bCentre for Acute Care Trauma, Manchester Academic Health Science Centre, Health Innovation Manchester, Division of Critical Care, Salford Royal NHS Foundation Trust, Greater Manchester, UK cDivision of Infection, Immunity and Respiratory Medicine, Faculty of Biology, Medicine & Health, AV Hill Building, The University of Manchester, Manchester, M13 9PT, UK. d Catalan Institute of Nanoscience and Nanotechnology (ICN2), Campus UAB, Bellaterra, 08193 Barcelona, Spain. _______________________________________ * Correspondence should be addressed to: [email protected],uk; [email protected] 1 Supporting Figure 1 Figure S1: Physicochemical characterization of corona-coated Amphotericin B-intercalated liposomes (AmBisome®). Mean hydrodynamic diameter (nm) and ζ-potential (mV) distributions are depicted for corona-coated liposomal formulation AmBisome® recovered post-incubation with human plasma from 12 healthy volunteers, 7 SIRS patients and 12 sepsis patients. 2 Supporting Figure 2 Figure S2: Proteomic analysis of corona profiles. (A) Heatmap of normalized abundance values of all corona proteins identified in healthy controls, SIRS patients and sepsis patients, as identified by LC-MS/MS (Progenesis QI). Protein columns are sorted according to the abundance values (from highest to lowest) of the first sample. The list of proteins shown in the heatmap, their respective accession numbers and their mean normalized abundance values are shown in Table S5; (B) Volcano plot represents the potential protein biomarkers differentially abundant between healthy donors and sepsis patients (n=135) identified in corona samples. -

The Role of Lamin Associated Domains in Global Chromatin Organization and Nuclear Architecture
THE ROLE OF LAMIN ASSOCIATED DOMAINS IN GLOBAL CHROMATIN ORGANIZATION AND NUCLEAR ARCHITECTURE By Teresa Romeo Luperchio A dissertation submitted to The Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland March 2016 © 2016 Teresa Romeo Luperchio All Rights Reserved ABSTRACT Nuclear structure and scaffolding have been implicated in expression and regulation of the genome (Elcock and Bridger 2010; Fedorova and Zink 2008; Ferrai et al. 2010; Li and Reinberg 2011; Austin and Bellini 2010). Discrete domains of chromatin exist within the nuclear volume, and are suggested to be organized by patterns of gene activity (Zhao, Bodnar, and Spector 2009). The nuclear periphery, which consists of the inner nuclear membrane and associated proteins, forms a sub- nuclear compartment that is mostly associated with transcriptionally repressed chromatin and low gene expression (Guelen et al. 2008). Previous studies from our lab and others have shown that repositioning genes to the nuclear periphery is sufficient to induce transcriptional repression (K L Reddy et al. 2008; Finlan et al. 2008). In addition, a number of studies have provided evidence that many tissue types, including muscle, brain and blood, use the nuclear periphery as a compartment during development to regulate expression of lineage specific genes (Meister et al. 2010; Szczerbal, Foster, and Bridger 2009; Yao et al. 2011; Kosak et al. 2002; Peric-Hupkes et al. 2010). These large regions of chromatin that come in molecular contact with the nuclear periphery are called Lamin Associated Domains (LADs). The studies described in this dissertation have furthered our understanding of maintenance and establishment of LADs as well as the relationship of LADs with the epigenome and other factors that influence three-dimensional chromatin structure. -

White Matter DNA Methylation Profiling Reveals Deregulation Of
Acta Neuropathologica (2020) 139:135–156 https://doi.org/10.1007/s00401-019-02074-0 ORIGINAL PAPER White matter DNA methylation profling reveals deregulation of HIP1, LMAN2, MOBP, and other loci in multiple system atrophy Conceição Bettencourt1,2 · Sandrine C. Foti1,3 · Yasuo Miki1,4 · Juan Botia5 · Aparajita Chatterjee1 · Thomas T. Warner1,2,6 · Tamas Revesz1,3 · Tammaryn Lashley1,3 · Robert Balazs1,3 · Emmanuelle Viré7 · Janice L. Holton1,2 Received: 2 July 2019 / Revised: 29 August 2019 / Accepted: 9 September 2019 / Published online: 18 September 2019 © The Author(s) 2019 Abstract Multiple system atrophy (MSA) is a fatal late-onset neurodegenerative disease. Although presenting with distinct pathological hallmarks, which in MSA consist of glial cytoplasmic inclusions (GCIs) containing fbrillar α-synuclein in oligodendro- cytes, both MSA and Parkinson’s disease are α-synucleinopathies. Pathologically, MSA can be categorized into striatonigral degeneration (SND), olivopontocerebellar atrophy (OPCA) or mixed subtypes. Despite extensive research, the regional vulnerability of the brain to MSA pathology remains poorly understood. Genetic, epigenetic and environmental factors have been proposed to explain which brain regions are afected by MSA, and to what extent. Here, we explored for the frst time epigenetic changes in post-mortem brain tissue from MSA cases. We conducted a case–control study, and profled DNA methylation in white mater from three brain regions characterized by severe-to-mild GCIs burden in the MSA mixed subtype (cerebellum, frontal lobe and occipital lobe). Our genome-wide approach using Illumina MethylationEPIC arrays and a powerful cross-region analysis identifed 157 CpG sites and 79 genomic regions where DNA methylation was signifcantly altered in the MSA mixed-subtype cases. -

Us 2018 / 0305689 A1
US 20180305689A1 ( 19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2018 /0305689 A1 Sætrom et al. ( 43 ) Pub . Date: Oct. 25 , 2018 ( 54 ) SARNA COMPOSITIONS AND METHODS OF plication No . 62 /150 , 895 , filed on Apr. 22 , 2015 , USE provisional application No . 62/ 150 ,904 , filed on Apr. 22 , 2015 , provisional application No. 62 / 150 , 908 , (71 ) Applicant: MINA THERAPEUTICS LIMITED , filed on Apr. 22 , 2015 , provisional application No. LONDON (GB ) 62 / 150 , 900 , filed on Apr. 22 , 2015 . (72 ) Inventors : Pål Sætrom , Trondheim (NO ) ; Endre Publication Classification Bakken Stovner , Trondheim (NO ) (51 ) Int . CI. C12N 15 / 113 (2006 .01 ) (21 ) Appl. No. : 15 /568 , 046 (52 ) U . S . CI. (22 ) PCT Filed : Apr. 21 , 2016 CPC .. .. .. C12N 15 / 113 ( 2013 .01 ) ; C12N 2310 / 34 ( 2013. 01 ) ; C12N 2310 /14 (2013 . 01 ) ; C12N ( 86 ) PCT No .: PCT/ GB2016 /051116 2310 / 11 (2013 .01 ) $ 371 ( c ) ( 1 ) , ( 2 ) Date : Oct . 20 , 2017 (57 ) ABSTRACT The invention relates to oligonucleotides , e . g . , saRNAS Related U . S . Application Data useful in upregulating the expression of a target gene and (60 ) Provisional application No . 62 / 150 ,892 , filed on Apr. therapeutic compositions comprising such oligonucleotides . 22 , 2015 , provisional application No . 62 / 150 ,893 , Methods of using the oligonucleotides and the therapeutic filed on Apr. 22 , 2015 , provisional application No . compositions are also provided . 62 / 150 ,897 , filed on Apr. 22 , 2015 , provisional ap Specification includes a Sequence Listing . SARNA sense strand (Fessenger 3 ' SARNA antisense strand (Guide ) Mathew, Si Target antisense RNA transcript, e . g . NAT Target Coding strand Gene Transcription start site ( T55 ) TY{ { ? ? Targeted Target transcript , e . -

Dizertační Práce
PÍRODOVDECKÁ FAKULTA Dizertační práce MARKÉTA WAYHELOVÁ Brno 2019 PÍRODOVDECKÁ FAKULTA Analýza patogenních genetických variant u dtí s mentálními retardacemi pomocí metod komparativní genomové hybridizace na mikročipech (array-CGH) a sekvenování "nové generace" (NGS) Dizertační práce MARKÉTA WAYHELOVÁ Vedoucí práce: doc. RNDr. Petr Kuglík, CSc. Ústav experimentální biologie Brno 2019 1 Bibliografický záznam Autorka: Markéta Wayhelová Přírodovědecká fakulta, Masarykova univerzita Ústav experimentální biologie Název práce: Analýza patogenních genetických variant u dětí s mentálními retardacemi pomocí metod komparativní genomové hybridizace na mikročipech (array-CGH) a sekvenování "nové generace" (NGS) Studijní program: Molekulární a buněčná biologie a genetika Vedoucí práce: doc. RNDr. Petr Kuglík, CSc. Akademický rok: 2019/2020 Počet stran: 164 + 19 Klíčová slova: Poruchy intelektuálního vývoje; array-CGH; varianty v počtu kopií; sekvenování „nové generace“; sekvenční varianty 2 Bibliographic entry Author: Markéta Wayhelová Faculty of Science, Masaryk University Department of Experimental Biology Název práce: The analysis of pathogenic genetic variants in children with disorders of intellectual development using methods of array-based comparative genomic hybridization (array-CGH) and „next-generation“ sequencing (NGS) Degree programme: Molecular and cell biology and genetics Supervisor: doc. RNDr. Petr Kuglík, CSc. Academic Year: 2019/2020 Number of pages: 164 + 19 Keywords: Disorders of intellectual development; array-CGH; copy-number variations; „next-generation“ sequencing; sequence variants 3 Abstrakt Poruchy intelektuálního vývoje (disorders of intellectual development, DID) se svojí průměrnou prevalencí u 1-3 % populace představují jedno z nejzávažnějších témat v oblasti zdravotní péče a každodenního života lidské společnosti. DID zahrnují soubor geneticky a fenotypově různorodých onemocnění s nástupem obvykle již v raném dětském věku, jež negativně ovlivňují život postiženého jedince ve všech aspektech života. -
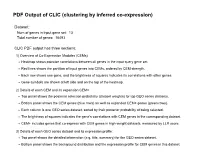
PDF Output of CLIC (Clustering by Inferred Co-Expression)
PDF Output of CLIC (clustering by inferred co-expression) Dataset: Num of genes in input gene set: 13 Total number of genes: 16493 CLIC PDF output has three sections: 1) Overview of Co-Expression Modules (CEMs) Heatmap shows pairwise correlations between all genes in the input query gene set. Red lines shows the partition of input genes into CEMs, ordered by CEM strength. Each row shows one gene, and the brightness of squares indicates its correlations with other genes. Gene symbols are shown at left side and on the top of the heatmap. 2) Details of each CEM and its expansion CEM+ Top panel shows the posterior selection probability (dataset weights) for top GEO series datasets. Bottom panel shows the CEM genes (blue rows) as well as expanded CEM+ genes (green rows). Each column is one GEO series dataset, sorted by their posterior probability of being selected. The brightness of squares indicates the gene's correlations with CEM genes in the corresponding dataset. CEM+ includes genes that co-express with CEM genes in high-weight datasets, measured by LLR score. 3) Details of each GEO series dataset and its expression profile: Top panel shows the detailed information (e.g. title, summary) for the GEO series dataset. Bottom panel shows the background distribution and the expression profile for CEM genes in this dataset. Overview of Co-Expression Modules (CEMs) with Dataset Weighting Scale of average Pearson correlations Num of Genes in Query Geneset: 13. Num of CEMs: 1. 0.0 0.2 0.4 0.6 0.8 1.0 Dnah6 Dnali1 Dnah7a Dnah2 Dnah1 Dnah8 Dnah5 Dnah9 -

Genetic, Transcriptome, Proteomic and Epidemiological Evidence for Blood Brain Barrier Disruption
bioRxiv preprint doi: https://doi.org/10.1101/080333; this version posted October 12, 2016. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Genetic, transcriptome, proteomic and epidemiological evidence for blood brain barrier disruption and polymicrobial brain invasion as determinant factors in Alzheimer’s disease. C.J.Carter, PolygenicPathways, Flat 2, 40 Baldslow Road, Hastings, East Sussex, TN34 2EY, UK Key words: virus, bacteria, fungi, microbes, Alzheimer’s disease, immune system, inflammation, blood brain barrier, gene/environment Running title: Alzheimer’s disease relationship with multiple pathogens Abstract Multiple pathogens have been detected in Alzheimer’s disease (AD) brains. A bioinformatics approach was used to assess relationships between pathogens and AD genes (GWAS), the AD hippocampal transcriptome and plaque or tangle proteins. Host/pathogen interactomes (C.albicans, C.Neoformans, Bornavirus, B.Burgdorferri, cytomegalovirus, Ebola virus, HSV-1, HERV-W, HIV-1, Epstein-Barr, hepatitis C, influenza, C.Pneumoniae, P.Gingivalis, H.Pylori, T.Gondii, T.Cruzi) significantly overlap with misregulated AD hippocampal genes , with plaque and tangle proteins and, except Bornavirus, Ebola and HERV-W, with AD genes. Upregulated AD hippocampal genes match those upregulated by multiple bacteria, viruses, fungi or protozoa in immunocompetent blood cells. AD genes are enriched in bone marrow and immune locations and in GWAS datasets reflecting pathogen diversity, suggesting selection for pathogen resistance. The age of AD patients implies resistance to infections afflicting the younger. -

Supporting Materials Results Demographic
Supporting Materials Results Demographic model selection: using PSMC/MSMC We applied the pairwise sequentially Markovian coalescent (PSMC, Li and Durbin 2011) and multiple sequentially Markovian coalescent (MSMC, Schiffels and Durbin 2014) as independent means to explore the demographic history of our populations (Materials and Methods). PSMC infers effective population size over time from a single diploid genome, while MSMC measures genetic separation of populations using relative cross coalescence rates between pairs of haplotypes from two populations. We applied both PSMC and MSMC to our quality-controlled intergenic data. The PSMC curves of the farmers begin to separate from those of the Pygmies roughly 100–200 kya (Figure S3A), suggesting that the ancestors of the farmers and Pygmies began differentiating from each other as early as 100–200 kya, consistent with the inferred divergence time in Model-1. The MSMC curves indicate declining genetic exchange between Pygmies and farmers ~40-60 kya, suggesting that these two populations may have diverged from each other at this time (Figure S3D-E). To test if Model-1 and Model-2 recapitulate the divergence times between farmers and Pygmies indicated by PSMC/MSMC, we applied both methods to simulated genomes under both models (Figure S3B-E). Under Model-1, the PSMC curves of the simulated Pygmy and farmer genomes split at about the same time as in the PSMC analysis of the real data (Figure S3B), while the two simulated populations of Model-2 do not show clear separation until ~70 kya (Figure S3C). The MSMC curves of Model-1 and those of real data agree well, but Model-2 seems to fit the MSMC curve from the real data poorly (Figure S3D-E). -

You Can Check If Genes Are Captured by the Agilent Sureselect V5 Exome
IIHG Clinical Exome Sequencing Test Gene Coverage • Whole Exome Sequencing is a targeted capture platform which does not capture the entire exome. Regions not captured by the exome will not be analyzed. o Please note, it is important to understand the absence of a reportable variant in a given gene does not mean there are not pathogenic variants in that gene. • Data sensitivity and specificity for exome testing is variable as gene coverage is not uniform throughout the exome. • The Agilent SureSelect XT Human All Exon v5 kit captures ~98% of Refseq coding base pairs, and >94% of the captured coding bases in the exome are covered at our depth-of-coverage minimum threshold (30 reads). • All test reports include the following information: o Regions of the Symptom Candidate Gene List which were not captured by the current exome capture platform. o Regions of the Symptom Candidate Gene List which were not sequenced to a sufficient depth of coverage to make a clinical diagnosis. • You can check if genes are captured by the Agilent Agilent SureSelect v5 exome capture, and how well those genes are typically covered here. • Explanations for the headings; • Symbol: Gene symbol • Chr: Chromosome • % Captured: the minimum portion of the gene captured by the Agilent SureSelect XT Human All Exon v5 kit. This includes all transcripts for a given gene. o 100.00% = the entire gene is captured o 0.00% = none of the gene is captured • % Covered: the minimum portion of the gene that has at least 30x average coverage when sequenced on the Illumina HiSeq2000 with 100 base pair (bp) paired-end reads for eight CEPH samples.