Proteomics Analysis to Identify and Characterize the Molecular Signatures of Hepatic Steatosis in Ovariectomized Rats As a Model of Postmenopausal Status
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanistic Studies on Medium Chain Acyl-Coa Dehydrogenase
Acyl-CoA Dehydrogenases: Mechanistic studies on Medium Chain Acyl-CoA Dehydrogenase Dissertation zur Erlangung des akademischen Grades des Doktors der Naturwissenschaften (Dr. rer. nat.) an der Universität Konstanz (Fachbereich Biologie) vorgelegt von Vasile Robert Gradinaru Konstanz, im Juni 2005 Tag der mündlichen Prüfung : 9. November 2005 Referent: Prof. Dr. Sandro Ghisla Referent: Prof. Dr. Peter Macheroux Acknowledgements I am greatly indebted to my supervisor, Prof. Dr. Sandro Ghisla, for his advice and support. He has been an excellent supervisor providing insightful comments and constructive criticism throughout this PhD project. I would also like to thank my colleagues in the Universities of Konstanz and Iasi for their advice, encouragement and friendship, without which I would certainly not have completed this thesis. In particular, I would like to thank Prof. Dr. Richard Schowen, Prof. Dr. Peter Macheroux, Prof. Dr. Colin Thorpe, Prof. Dr. Jung-Ja. Kim, Prof. Dr. Tatiana Nicolaescu, Prof. Dr. Constantin Ciugureanu, Prof. Dr. Robert Bach, Dr. Olga Dmitrenko, Susanne Feindler-Boeckh, Gudrun Vogt, Elmi Leisner, Karl Janko, Lili Smau, Nasser Ibrahim, Phaneeswara Rao Kommoju, Sudarshan Rao Ande, Lakshminarayana Kaza, Cosmin Pocanschi, Paula Bulieris for their active interest during the course of this project. My gratitude also goes to Prof. Alexandru Cecal for encouraging me to embark on this PhD. I express my loving thanks to my wife Luiza whose love, support, patience and understanding made this work easier. Above all, I wish to express my sincerest gratitude to my parents, who made my studies possible and who have always encouraged me. This study was financiarlly supported by the Deutsche Forschungsgemeinschaft (Gh 2/6-4). -
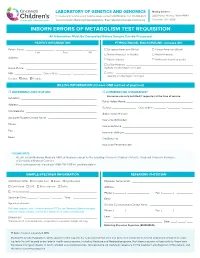
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

ACADS Rabbit Pab
Leader in Biomolecular Solutions for Life Science ACADS Rabbit pAb Catalog No.: A0945 2 Publications Basic Information Background Catalog No. This gene encodes a tetrameric mitochondrial flavoprotein, which is a member of the A0945 acyl-CoA dehydrogenase family. This enzyme catalyzes the initial step of the mitochondrial fatty acid beta-oxidation pathway. Mutations in this gene have been Observed MW associated with short-chain acyl-CoA dehydrogenase (SCAD) deficiency. Alternative 44kDa splicing results in two variants which encode different isoforms. Calculated MW 44kDa Category Primary antibody Applications WB, IHC, IF Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 35 P16219 IHC 1:50 - 1:100 Immunogen 1:50 - 1:200 IF Recombinant fusion protein containing a sequence corresponding to amino acids 1-260 of human ACADS (NP_000008.1). Synonyms ACADS;ACAD3;SCAD Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using ACADS antibody (A0945) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Detection: ECL Basic Kit (RM00020). Exposure time: 15s. Immunohistochemistry of paraffin- Immunohistochemistry of paraffin- Immunofluorescence analysis of U2OS embedded human liver cancer using embedded human liver damage using cells using ACADS antibody (A0945). Blue: ACADS antibody (A0945) at dilution of ACADS antibody (A0945) at dilution of DAPI for nuclear staining. -

Positive Carrier Sample Report
RESULTS RECIPIENT FEMALE MALE UNIVERSITY MEDICAL CENTER JANE MILLER N/A Attn: Dr. Paul Smith DOB: 11/11/1977 123 Main Street Ethnicity: Northern European City, CA 10231 Sample Type: OG-510 Saliva Phone: (800) 555-1212 Date of Collection: 02/06/2020 Fax: (800) 555-1212 Date Received: 02/16/2020 NPI: 4253506008 Date Tested: 02/16/2020 Report Date: 02/18/2020 Barcode: 55200006634190 Accession ID: FAKERQSCARFAF Indication: Screening for genetic disease carrier status Foresight® Carrier Screen POSITIVE: CARRIER ABOUT THIS TEST The Myriad Foresight Carrier Screen utilizes sequencing, maximizing coverage across all DNA regions tested, to help you learn about your chance to have a child with a genetic disease. RESULTS SUMMARY Risk Details JANE MILLER Partner Panel Information Foresight Carrier Screen N/A Universal Panel Fundamental Plus Panel Fundamental Panel Fragile X Syndrome (176 conditions tested) POSITIVE: CARRIER CARRIER* The reproductive risk presented Smith‑Lemli‑Opitz Syndrome NM_001360.2(DHCR7):c. is based on a hypothetical 964-1G>C(aka IVS8-1G>C) pairing with a partner of the Reproductive Risk: 1 in 380 heterozygote same ethnic group. Carrier Inheritance: Autosomal Recessive testing should be considered. See "Next Steps". *Carriers generally do not experience symptoms. No disease-causing mutations were detected in any other gene tested. A complete list of all conditions tested can be found on page 6. Additional Findings Single Carrier Autosomal recessive additional findings CLINICAL NOTES NEXT STEPS • None • Carrier testing should be considered for the diseases specified above for the patient's partner, as both parents must be carriers before a child is at high risk of developing the disease. -

Excluded Test List – As of 08/01/2016
Excluded Test List – as of 08/01/2016 CPT As Gene Code 81161 DMD, dup_del 81200 ASPA, cv 81201 APC, fgs 81202 APC, kfv 81203 APC, dup_del 81205 BCKDHA, cv 81205 BCKDHB, cv 81209 BLM, 2281del6ins7 81220 CFTR, cv 81221 CFTR, kfv 81222 CFTR, dup_del 81223 CFTR, fgs 81224 CFTR, intron 8 poly-T 81228 Microarray, CNV 81229 Microarray, SNP 81240 F2, 20210G>A 81241 F5, Leiden (1691G>A) 81242 FANCC, cv 81243 FMR1 81244 FMR1, ma 81250 G6PC, cv 81251 GBA, cv 81252 GJB2, fgs 81253 GJB2, kfv 81254 GJB6, cv 81255 HEXA, cv 81257 HBA1_HBA2, cdel or v 81260 IKBKAP, cv 81271 SRY-FISH 81280 LQT, fgs 12 genes 81281 LQT, kfv 81282 LQT, dup_del 12 genes 81290 MCOLN1, cv 81291 MTHFR, cv 81302 MECP2, fgs 81304 MECP2, dup_del 81324 PMP22, dup_del 81325 PMP22, fgs 1, V14 81326 PMP22, kfv 81330 SMPD1, cv 81331 SNRPN_UBE3A, ma 81350 UGT1A1, cv 81400 ABCC8, F1388del 81400 ACADM, K304E 81400 AGTR1, 1166A>C 81400 BCKDHA, Y438n 81400 CCR5, del 81400 CLRN1, N48K 81400 DPYD, IVS14+1G>A 81400 FGFR1, P252R 81400 FGFR3, P250R 81400 FKTN, retro ins v 81400 GNE, M712T 81400 HPA-6 81400 HPA-9 81400 IVD, A282V 81400 LCT, 13910 C>T 81400 NEB, exon 55 81400 PCDH15, R245X 81400 SHOC2, S2G 81400 SLCO1B1, V174A 81400 SMN1, exon 7 del 81400 SRY, fgs 81400 TOR1A, var 81401 ABCC8, cv 81401 ACADM, cv 81401 ADRB2, cv 81401 AFF2, detect abn 81401 APOB, cv 81401 APOE, cv 81401 AR, alleles 81401 ATN1 81401 ATXN1 81401 ATXN10 81401 ATXN2 81401 ATXN3 81401 ATXN7 81401 ATXN8OS 81401 CACNA1A 2, V14 81401 CBS, cv 81401 CFH_ARMS2, cv 81401 CNBP 81401 CSTB 81401 CYP3A4, cv 81401 CYP3A5, cv 81401 -

Flavin Adenine Dinucleotide Status and the Effects of High-Dose Riboflavin Treatment in Short-Chain Acyl-Coa Dehydrogenase Deficiency
0031-3998/10/6703-0304 Vol. 67, No. 3, 2010 PEDIATRIC RESEARCH Printed in U.S.A. Copyright © 2010 International Pediatric Research Foundation, Inc. Flavin Adenine Dinucleotide Status and the Effects of High-Dose Riboflavin Treatment in Short-Chain Acyl-CoA Dehydrogenase Deficiency BIANCA T. VAN MALDEGEM, MARINUS DURAN, RONALD J. A. WANDERS, HANS R. WATERHAM, AND FRITS A. WIJBURG Department of Pediatrics [B.T.M, F.A.W.] and Laboratory Genetic Metabolic Diseases [M.D., R.J.A.W., H.R.W.], University of Amsterdam, 1105 AZ Amsterdam, the Netherlands ABSTRACT: Short-chain acyl-CoA dehydrogenase deficiency most US states (15). In addition, potential treatment options (SCADD) is an inborn error, biochemically characterized by in- for SCADD have never been systematically studied. creased plasma butyrylcarnitine (C4-C) concentration and increased SCADD is caused by decreased activity of the first enzyme ethylmalonic acid (EMA) excretion and caused by rare mutations of the short-chain fatty acid -oxidation spiral, which cata- and/or common gene variants in the SCAD encoding gene. Although lyzes the dehydrogenation of butyryl-CoA (C4-CoA). When its clinical relevance is not clear, SCADD is included in most US SCAD activity is impaired, C4-CoA will accumulate and is newborn screening programs. Riboflavin, the precursor of flavin subsequently converted into different metabolites including 1) adenine dinucleotide (FAD, cofactor), might be effective for treating the corresponding carnitine-ester, i.e. butyrylcarnitine (C4-C); SCADD. We assessed the FAD status and evaluated the effects of riboflavin treatment in a prospective open-label cohort study involv- 2) the corresponding glycine ester (butyrylglycine); 3) bu- ing 16 patients with SCADD, subdivided into mutation/mutation tyrate; and 4) ethylmalonic acid (EMA). -

Activation of Pparα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis
Tohoku J. Exp. Med., 2016, 240, 113-122PPARα Activation in Cells due to VLCAD Deficiency 113 Activation of PPARα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis * * Yang Yang,1, Yuyao Feng,1, Xiaowei Zhang,2 Takero Nakajima,1 Naoki Tanaka,1 Eiko Sugiyama,3 Yuji Kamijo4 and Toshifumi Aoyama1 1Department of Metabolic Regulation, Shinshu University Graduate School of Medicine, Matsumoto, Nagano, Japan 2Department of Neurosurgery, The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, China 3Department of Nutritional Science, Nagano Prefectural College, Nagano, Nagano, Japan 4Department of Nephrology, Shinshu University School of Medicine, Matsumoto, Nagano, Japan Very-long-chain acyl-CoA dehydrogenase (VLCAD) catalyzes the first reaction in the mitochondrial fatty acid β-oxidation pathway. VLCAD deficiency is associated with the accumulation of fat in multiple organs and tissues, which results in specific clinical features including cardiomyopathy, cardiomegaly, muscle weakness, and hepatic dysfunction in infants. We speculated that the abnormal fatty acid metabolism in VLCAD-deficient individuals might cause cell necrosis by fatty acid toxicity. The accumulation of fatty acids may activate peroxisome proliferator-activated receptor (PPAR), a master regulator of fatty acid metabolism and a potent nuclear receptor for free fatty acids. We examined six skin fibroblast lines, derived from VLCAD-deficient patients and identified fatty acid accumulation and PPARα activation in these cell lines. We then found that the expression levels of three enzymes involved in fatty acid degradation, including long-chain acyl-CoA synthetase (LACS), were increased in a PPARα-dependent manner. This increased expression of LACS might enhance the fatty acyl-CoA supply to fatty acid degradation and sulfatide synthesis pathways. -

Suppression of Fatty Acid Oxidation by Thioesterase Superfamily Member
bioRxiv preprint doi: https://doi.org/10.1101/2021.04.21.440732; this version posted April 21, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Suppression of Fatty Acid Oxidation by Thioesterase Superfamily Member 2 in Skeletal Muscle Promotes Hepatic Steatosis and Insulin Resistance Norihiro Imai1, Hayley T. Nicholls1, Michele Alves-Bezerra1, Yingxia Li1, Anna A. Ivanova2, Eric A. Ortlund2, and David E. Cohen1 1Division of Gastroenterology and Hepatology, Joan & Sanford I. Weill Department of Medicine, Weill Cornell Medical College, NY 10021 USA 2Department of Biochemistry, Emory University, Atlanta, GA 30322 USA Current addresses: Norihiro Imai - Department of Gastroenterology and Hepatology, Nagoya University School of Medicine, Aichi 4668560 Japan Michele Alves-Bezerra - Department of Molecular Physiology and Biophysics, Baylor College of Medicine, Houston, TX 77030 USA bioRxiv preprint doi: https://doi.org/10.1101/2021.04.21.440732; this version posted April 21, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Figure number: 8 Supplemental figure number: 10 Supplemental table number: 2 References: 48 Keywords: Hepatic steatosis, obesity, acyl-CoA thioesterase, fatty acid oxidation, insulin resistance Conflict of interest: The authors have declared that no conflict of interest exists. Author contributions: N.I.: designed research studies, conducted experiments, acquired data, analyzed data and wrote manuscript. H.T.N.: conducted experiments and analyzed data, M.A.B.: designed research studies and conducted experiments, Y.L.: acquired data, A.A.I.: conducted experiments and analyzed data, E.A.O.: analyzed data, D.E.C.: designed research studies, analyzed data and wrote manuscript. -

1 Supplemental Information Development of an in Vitro Human
Supplemental Information Development of an In Vitro Human Liver System for Interrogating Non-Alcoholic Steatohepatitis Ryan Feaver1, Banumathi K. Cole1, Mark J. Lawson1, Stephen A. Hoang1, Svetlana Marukian1, Robert A. Figler1, Arun J. Sanyal2, Brian R. Wamhoff*1, Ajit Dash1 1HemoShear Therapeutics LLC, Charlottesville, VA 2Virginia Commonwealth University School of Medicine Richmond, VA *Corresponding Author: Brian R. Wamhoff, 501 Locust Ave., Charlottesville, VA 22902 [email protected] 434-872-0196 1 Supplemental Figures and Tables: log2 Fold Change Values ● ● ● ● ● ● ● ● 5 ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●● ● ● ● ● ● ● ● ● ● ● ● ●● ● ● ● ● ● ● ● ● ● ● ● ● ● ●● ● ● ● ●● ● ● ● ● ● ● ●● ● ● ● ●●●● ●● ● ● ● ● ●●● ● ● ● ● ●● ●●●● ●●●●●● ● ● ● ● ● ●● ● ● ● ● ●● ●●●●●●●●●●●●●●●● ● ● ● ● ● ●●● ●●●●●●●●●●●●●● ● ● ● ●●●●●●●●●●●●●●●●● ● ●● ● ● ●●● ●● ●●●●●●●● ●●●●●●●●●●● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●● ● ● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ●● ●●● ● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ● ● ● ● ●●●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●●● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●● ● ● ● ● ●● ●● ● ●●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●●●●●● ● ● ●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ●●● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ● ● ● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ● ●● ●●●●●●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●●● ●●●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● -

Role of Metabolism in Bone Development and Homeostasis
International Journal of Molecular Sciences Review Role of Metabolism in Bone Development and Homeostasis Akiko Suzuki 1,2 , Mina Minamide 1,2, Chihiro Iwaya 1,2, Kenichi Ogata 1,2 and Junichi Iwata 1,2,3,* 1 Department of Diagnostic & Biomedical Sciences, School of Dentistry, The University of Texas Health Science Center at Houston, Houston, TX 77054, USA; [email protected] (A.S.); [email protected] (M.M.); [email protected] (C.I.); [email protected] (K.O.) 2 Center for Craniofacial Research, The University of Texas Health Science Center at Houston, Houston, TX 77054, USA 3 MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences, Houston, TX 77030, USA * Correspondence: [email protected] Received: 16 October 2020; Accepted: 25 November 2020; Published: 26 November 2020 Abstract: Carbohydrates, fats, and proteins are the underlying energy sources for animals and are catabolized through specific biochemical cascades involving numerous enzymes. The catabolites and metabolites in these metabolic pathways are crucial for many cellular functions; therefore, an imbalance and/or dysregulation of these pathways causes cellular dysfunction, resulting in various metabolic diseases. Bone, a highly mineralized organ that serves as a skeleton of the body, undergoes continuous active turnover, which is required for the maintenance of healthy bony components through the deposition and resorption of bone matrix and minerals. This highly coordinated event is regulated throughout life by bone cells such as osteoblasts, osteoclasts, and osteocytes, and requires synchronized activities from different metabolic pathways. Here, we aim to provide a comprehensive review of the cellular metabolism involved in bone development and homeostasis, as revealed by mouse genetic studies. -

Tissue Specific Roles of Fatty Acid Oxidation
TISSUE SPECIFIC ROLES OF FATTY ACID OXIDATION by Jieun Lee A dissertation submitted to Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland September, 2016 © 2016 Jieun Lee All Rights Reserved ABSTRACT The oxidation of long chain fatty acids facilitates mitochondrial respiration in diverse cell types. In this thesis, the role of fatty acid oxidation primarily in the adipose tissue and liver are discussed. To address this question, we generated mice with an adipose- or liver-specific knockout of carnitine palmitoyltransferase 2 (Cpt2), an obligate step in long chain mitochondrial fatty acid oxidation. In adipocyte-specific KO mice (Cpt2A-/-), the brown adipose tissue (BAT) of Cpt2A-/- mice was unable to utilize fatty acids and therefore caused hypothermia after an acute cold challenge. Surprisingly, Cpt2A-/- BAT was also unable to up-regulate thermogenic genes such as Ucp1 and Pgc1a in response to agonist-induced stimulation in vivo or ex vivo. The adipose specific loss of CPT2 did not result in changes in body weight on low or high fat diets, although paradoxically, low fat diets promoted and high fat diets suppressed adiposity. Additionally, a high fat diet increased oxidative stress and inflammation in gonadal white adipose tissue (WAT) of control mice but this effect was greatly suppressed in Cpt2A-/- mice. However, this suppression did not improve high fat diet induced glucose intolerance. In hepatocyte-specific KO (Cpt2L-/-) mice, fasting induced hepatic steatosis and serum dyslipidemia with an absence of circulating ketones while blood glucose remained normal. Systemic energy homeostasis was largely maintained in fasting Cpt2L-/- mice by adaptations in hepatic and systemic oxidative gene expression mediated in part by Pparα target genes including procatabolic hepatokines Fgf21, Gdf15 and Igfbp1. -

Construction and Validation of a Prognostic Gene-Based Model For
Article Construction and Validation of a Prognostic Gene-Based Model for Overall Survival Prediction in Hepatocellular Carcinoma Using an Integrated Statistical and Bioinformatic Approach Eskezeia Y. Dessie 1, Siang-Jyun Tu2, Hui-Shan Chiang2, Jeffrey J.P. Tsai1, Ya-Sian Chang2,*, Jan-Gowth Chang2,* and Ka-Lok Ng 1, 3, 4,* 1 Department of Bioinformatics and Medical Engineering, Asia University, Taichung, Taiwan; No. 500, Li- oufeng Rd., Wufeng, Taichung 41354, Taiwan; [email protected] (E.Y.D.); [email protected] (J.-P.T.); [email protected] (K.-L.N.) 2 Department of Laboratory Medicine, and Center for Precision Medicine, China Medical University and Hospital, Taichung, Taiwan; No. 2, Yude Rd., North Dist., Taichung City 404332, Taiwan; [email protected] (S.-J.T.); [email protected] (H.-S.C.); [email protected] (Y.-S.C.); [email protected] (J.-G.C.) 3 Department of Medical Research, China Medical University Hospital, China Medical University, Taichung, Taiwan; No. 2, Yude Rd., North Dist., Taichung City 404332, Taiwan; [email protected] (K.-L.N.) 4 Center for Artificial Intelligence and Precision Medicine Research, Asia University, Taichung, Taiwan; No. 500, Lioufeng Rd., Wufeng, Taichung 41354, Taiwan; [email protected] (K.-L.N.) * Correspondence: [email protected] (Y.-S.C.); [email protected] (K.-L.N.); [email protected] (J.-G.C.) Int. J. Mol. Sci. 2021, 22, 1632. https://doi.org/10.3390/ijms22041632 www.mdpi.com/journal/ijms Int. J. Mol. Sci. 2021, 22, 1632 2 of 7 Int. J. Mol. Sci.