Flavin Adenine Dinucleotide Status and the Effects of High-Dose Riboflavin Treatment in Short-Chain Acyl-Coa Dehydrogenase Deficiency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanistic Studies on Medium Chain Acyl-Coa Dehydrogenase
Acyl-CoA Dehydrogenases: Mechanistic studies on Medium Chain Acyl-CoA Dehydrogenase Dissertation zur Erlangung des akademischen Grades des Doktors der Naturwissenschaften (Dr. rer. nat.) an der Universität Konstanz (Fachbereich Biologie) vorgelegt von Vasile Robert Gradinaru Konstanz, im Juni 2005 Tag der mündlichen Prüfung : 9. November 2005 Referent: Prof. Dr. Sandro Ghisla Referent: Prof. Dr. Peter Macheroux Acknowledgements I am greatly indebted to my supervisor, Prof. Dr. Sandro Ghisla, for his advice and support. He has been an excellent supervisor providing insightful comments and constructive criticism throughout this PhD project. I would also like to thank my colleagues in the Universities of Konstanz and Iasi for their advice, encouragement and friendship, without which I would certainly not have completed this thesis. In particular, I would like to thank Prof. Dr. Richard Schowen, Prof. Dr. Peter Macheroux, Prof. Dr. Colin Thorpe, Prof. Dr. Jung-Ja. Kim, Prof. Dr. Tatiana Nicolaescu, Prof. Dr. Constantin Ciugureanu, Prof. Dr. Robert Bach, Dr. Olga Dmitrenko, Susanne Feindler-Boeckh, Gudrun Vogt, Elmi Leisner, Karl Janko, Lili Smau, Nasser Ibrahim, Phaneeswara Rao Kommoju, Sudarshan Rao Ande, Lakshminarayana Kaza, Cosmin Pocanschi, Paula Bulieris for their active interest during the course of this project. My gratitude also goes to Prof. Alexandru Cecal for encouraging me to embark on this PhD. I express my loving thanks to my wife Luiza whose love, support, patience and understanding made this work easier. Above all, I wish to express my sincerest gratitude to my parents, who made my studies possible and who have always encouraged me. This study was financiarlly supported by the Deutsche Forschungsgemeinschaft (Gh 2/6-4). -
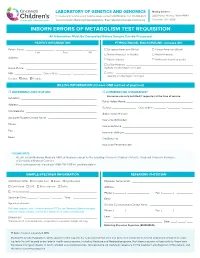
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

ACADS Rabbit Pab
Leader in Biomolecular Solutions for Life Science ACADS Rabbit pAb Catalog No.: A0945 2 Publications Basic Information Background Catalog No. This gene encodes a tetrameric mitochondrial flavoprotein, which is a member of the A0945 acyl-CoA dehydrogenase family. This enzyme catalyzes the initial step of the mitochondrial fatty acid beta-oxidation pathway. Mutations in this gene have been Observed MW associated with short-chain acyl-CoA dehydrogenase (SCAD) deficiency. Alternative 44kDa splicing results in two variants which encode different isoforms. Calculated MW 44kDa Category Primary antibody Applications WB, IHC, IF Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 35 P16219 IHC 1:50 - 1:100 Immunogen 1:50 - 1:200 IF Recombinant fusion protein containing a sequence corresponding to amino acids 1-260 of human ACADS (NP_000008.1). Synonyms ACADS;ACAD3;SCAD Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using ACADS antibody (A0945) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Detection: ECL Basic Kit (RM00020). Exposure time: 15s. Immunohistochemistry of paraffin- Immunohistochemistry of paraffin- Immunofluorescence analysis of U2OS embedded human liver cancer using embedded human liver damage using cells using ACADS antibody (A0945). Blue: ACADS antibody (A0945) at dilution of ACADS antibody (A0945) at dilution of DAPI for nuclear staining. -

Positive Carrier Sample Report
RESULTS RECIPIENT FEMALE MALE UNIVERSITY MEDICAL CENTER JANE MILLER N/A Attn: Dr. Paul Smith DOB: 11/11/1977 123 Main Street Ethnicity: Northern European City, CA 10231 Sample Type: OG-510 Saliva Phone: (800) 555-1212 Date of Collection: 02/06/2020 Fax: (800) 555-1212 Date Received: 02/16/2020 NPI: 4253506008 Date Tested: 02/16/2020 Report Date: 02/18/2020 Barcode: 55200006634190 Accession ID: FAKERQSCARFAF Indication: Screening for genetic disease carrier status Foresight® Carrier Screen POSITIVE: CARRIER ABOUT THIS TEST The Myriad Foresight Carrier Screen utilizes sequencing, maximizing coverage across all DNA regions tested, to help you learn about your chance to have a child with a genetic disease. RESULTS SUMMARY Risk Details JANE MILLER Partner Panel Information Foresight Carrier Screen N/A Universal Panel Fundamental Plus Panel Fundamental Panel Fragile X Syndrome (176 conditions tested) POSITIVE: CARRIER CARRIER* The reproductive risk presented Smith‑Lemli‑Opitz Syndrome NM_001360.2(DHCR7):c. is based on a hypothetical 964-1G>C(aka IVS8-1G>C) pairing with a partner of the Reproductive Risk: 1 in 380 heterozygote same ethnic group. Carrier Inheritance: Autosomal Recessive testing should be considered. See "Next Steps". *Carriers generally do not experience symptoms. No disease-causing mutations were detected in any other gene tested. A complete list of all conditions tested can be found on page 6. Additional Findings Single Carrier Autosomal recessive additional findings CLINICAL NOTES NEXT STEPS • None • Carrier testing should be considered for the diseases specified above for the patient's partner, as both parents must be carriers before a child is at high risk of developing the disease. -

A Computational Approach for Identifying Plant-Based Foods for Addressing Vitamin Deficiency Diseases
University of Vermont ScholarWorks @ UVM UVM Honors College Senior Theses Undergraduate Theses 2015 A Computational Approach for Identifying Plant-Based Foods for Addressing Vitamin Deficiency Diseases Christina Yu University of Vermont Indra Neil Sarkar University of Vermont Follow this and additional works at: https://scholarworks.uvm.edu/hcoltheses Recommended Citation Yu, Christina and Sarkar, Indra Neil, "A Computational Approach for Identifying Plant-Based Foods for Addressing Vitamin Deficiency Diseases" (2015). UVM Honors College Senior Theses. 212. https://scholarworks.uvm.edu/hcoltheses/212 This Honors College Thesis is brought to you for free and open access by the Undergraduate Theses at ScholarWorks @ UVM. It has been accepted for inclusion in UVM Honors College Senior Theses by an authorized administrator of ScholarWorks @ UVM. For more information, please contact [email protected]. A Computational Approach for Identifying Plant-Based Foods for Addressing Vitamin Deficiency Diseases Christina Yu1 and Indra Neil Sarkar2,3 Key words: computing methodologies, vitamin deficiency diseases, vegetarian diet 1 Undergraduate Program in Biochemistry, University of Vermont, Burlington, VT 2 Department of Microbiology and Molecular Genetics, University of Vermont, Burlington, VT 3 Center for Clinical and Translational Science, University of Vermont, Burlington, VT 1 ABSTRACT Vitamins are nutrients that are essential to human health, and deficiencies have been shown to cause severe diseases. In this study, a computational approach was used to identify vitamin deficiency diseases and plant-based foods with vitamin content. Data from the United States Department of Agriculture Standard Reference (SR27), National Library of Medicine's Medical Subject Headings and MEDLINE, and Wikipedia were combined to identify vitamin deficiency diseases and vitamin content of plant-based foods. -

Excluded Test List – As of 08/01/2016
Excluded Test List – as of 08/01/2016 CPT As Gene Code 81161 DMD, dup_del 81200 ASPA, cv 81201 APC, fgs 81202 APC, kfv 81203 APC, dup_del 81205 BCKDHA, cv 81205 BCKDHB, cv 81209 BLM, 2281del6ins7 81220 CFTR, cv 81221 CFTR, kfv 81222 CFTR, dup_del 81223 CFTR, fgs 81224 CFTR, intron 8 poly-T 81228 Microarray, CNV 81229 Microarray, SNP 81240 F2, 20210G>A 81241 F5, Leiden (1691G>A) 81242 FANCC, cv 81243 FMR1 81244 FMR1, ma 81250 G6PC, cv 81251 GBA, cv 81252 GJB2, fgs 81253 GJB2, kfv 81254 GJB6, cv 81255 HEXA, cv 81257 HBA1_HBA2, cdel or v 81260 IKBKAP, cv 81271 SRY-FISH 81280 LQT, fgs 12 genes 81281 LQT, kfv 81282 LQT, dup_del 12 genes 81290 MCOLN1, cv 81291 MTHFR, cv 81302 MECP2, fgs 81304 MECP2, dup_del 81324 PMP22, dup_del 81325 PMP22, fgs 1, V14 81326 PMP22, kfv 81330 SMPD1, cv 81331 SNRPN_UBE3A, ma 81350 UGT1A1, cv 81400 ABCC8, F1388del 81400 ACADM, K304E 81400 AGTR1, 1166A>C 81400 BCKDHA, Y438n 81400 CCR5, del 81400 CLRN1, N48K 81400 DPYD, IVS14+1G>A 81400 FGFR1, P252R 81400 FGFR3, P250R 81400 FKTN, retro ins v 81400 GNE, M712T 81400 HPA-6 81400 HPA-9 81400 IVD, A282V 81400 LCT, 13910 C>T 81400 NEB, exon 55 81400 PCDH15, R245X 81400 SHOC2, S2G 81400 SLCO1B1, V174A 81400 SMN1, exon 7 del 81400 SRY, fgs 81400 TOR1A, var 81401 ABCC8, cv 81401 ACADM, cv 81401 ADRB2, cv 81401 AFF2, detect abn 81401 APOB, cv 81401 APOE, cv 81401 AR, alleles 81401 ATN1 81401 ATXN1 81401 ATXN10 81401 ATXN2 81401 ATXN3 81401 ATXN7 81401 ATXN8OS 81401 CACNA1A 2, V14 81401 CBS, cv 81401 CFH_ARMS2, cv 81401 CNBP 81401 CSTB 81401 CYP3A4, cv 81401 CYP3A5, cv 81401 -

VITAMINS by Dr
VITAMINS BY Dr. Samy Ali Hussein Aziza Professor of Biochemistry and Clinical Biochemistry Faculty of Veterinary Medicine, Moshtohor, Benha University, Egypt. E-Mail: [email protected] Vitamins Vitamins are organic compounds characterized by: Essential for normal health and growth. Essential for biological activity in the body. Present in food in very small concentration. Not enter in the tissue structure as carbohydrates, lipids and proteins. Act as catalysts and are not oxidized to give energy as carbohydrates, lipids and proteins. Deficiency of any vitamin in the body results in production of specific diseases. Many vitamin function as coenzymes. Not synthesized in the body by anabolic reaction, therefore should be taken in the diet. Some vitamin are present in food in the form of provitamins. Provitamin They are vitamin precursors. Example: • Carotenes are provitamin A. • 7- dehydrocholesterol are provitamin D3 Vitamer When a vitamin is present in more than one chemical formula each is called a vitamers Example: • Vitamin A has Two vitamers A1 and A2. • Vitamin D has two vitamers D2 and D3. • Vitamin E has four vitamers alpha, beta, gama, delta. Vitagen These include both essential Amino acids and essential fatty acids. Classification of vitamins Vitamins can be classified according to their solubility and their function in metabolism into: I- Fat soluble vitamins II- Water soluble vitamins I- Fat Soluble Vitamins Vitamin A Vitamin D Vitamin E Vitamin K II-WATER SOLUBLE VITAMINS I- B- complex – Thiamine (B1) – Riboflavin (B2) – Niacin (B3) – Folic acid – Pyridoxine (B6) – Vitamin B12 – Pantothenic Acid – Biotin II- Non B- complex : Vitamin C (ascorbic acid). B- complex a- Energy-releasing. -

Challenges to Quantify Total Vitamin Activity: How to Combine the Contribution of Diverse Vitamers?
REVIEW CURRENT DEVELOPMENTS IN NUTRITION Challenges to Quantify Total Vitamin Activity: How to Combine the Contribution of Diverse Vitamers? Jette Jakobsen ,1 Alida Melse-Boonstra ,2 and Michael Rychlik 3,4 1National Food Institute, Technical University of Denmark, Kongens Lyngby, Denmark; 2Division of Human Nutrition and Health, Wageningen University & Research, Wageningen, the Netherlands; 3Technical University of Munich, Freising, Germany; and 4Centre for Nutrition and Food Sciences, Queensland Alliance for Agriculture and Food Innovation, The University of Queensland, Coopers Plains, Australia ABSTRACT This state-of-the-art review aims to highlight the challenges in quantifying vitamin activity in foods that contain several vitamers of a group, using as examples the fat-soluble vitamins A and D as well as the water-soluble folate. The absorption, metabolism, and physiology of these examples are described along with the current analytical methodology, with an emphasis on approaches to standardization. Moreover, the major food sources for the vitamins are numerated. The article focuses particularly on outlining the so-called SLAMENGHI factors influencing a vitamer’s’ ability to act as a vitamin, that is, molecular species, linkage, amount, matrix, effectors of absorption, nutrition status, genetics, host-related factors, and the interaction of these. After summarizing the current approaches to estimating the total content of each vitamin group, the review concludes by outlining the research gaps and future perspectives in vitamin analysis. There are no standardized methods for the quantification of the vitamers of vitamin A, vitamin D, and folate in foods. For folate and β-carotene, a difference in vitamer activity between foods and supplements has been confirmed, whereas no difference has been observed for vitamin D. -

Department of Statistics Academic Program Review Spring 2015
Department of Statistics Academic Program Review Spring 2015 Department of Statistics • Texas A&M University • 3143 TAMU • College Station, TX 77843-3143 (979) 845-3141 • www.stat.tamu.edu Table of Contents I. Introduction Brief History of the Department……………………………………………………. 4 Mission and Goals………………………………………………………………….. 8 Administrative Structure of the Department………………………………………... 11 Resources…………………………………………………………………………... 13 Analysis……………………………………………………………………………. 14 Undergraduate Program……………………………………………………………. 15 Graduate Program………………………………………………………………….. 16 Professional Education……………………………………………………………... 19 Challenges and Opportunities……………………………………………………… 20 Assessment………………………………………………………………………… 22 II. Student Report Graduate Program in Statistics……………………………………………………… 28 Master of Science Program…………………………………………………………. 29 Doctor of Philosophy Program……………………………………………………... 32 Internship Program…………………………………………………………………. 35 Undergraduate Course Offerings…………………………………………………… 36 Graduate Course Offerings………………………………………………………… 37 Scheduling Coursework…………………………………………………………….. 42 Graduate Program Admissions Criteria……………………………………………... 43 GRE Scores for First Time Students………………………………………………... 44 Graduate Students Applied, Admitted, and Enrolled ………………………………. 45 Students by GPR Range……………………………………………………………. 48 Institutional Support for Full Time Students……………………………………….. 50 Honors & Awards Received by Students…………………………………………… 51 Statistics Graduate Student Association…………………………………………….. 54 Student Publications……………………………………………………………….. -

Comprehensive Vitamer Profiling of Folate Mono
H OH metabolites OH Article Comprehensive Vitamer Profiling of Folate Mono- and Polyglutamates in Baker’s Yeast (Saccharomyces cerevisiae) as a Function of Different Sample Preparation Procedures Lena Gmelch 1, Daniela Wirtz 1, Michael Witting 1,2 , Nadine Weber 1 , Lisa Striegel 1 , Philippe Schmitt-Kopplin 1,2,* and Michael Rychlik 1,2,* 1 Chair of Analytical Food Chemistry, Technical University of Munich, 85354 Freising-Weihenstephan, Germany; [email protected] (L.G.); [email protected] (D.W.); [email protected] (M.W.); [email protected] (N.W.); [email protected] (L.S.) 2 Research Unit BioGeoChemistry, Helmholtz Zentrum Munich, 85764 Neuherberg, Germany * Correspondence: [email protected] (P.S.-K.); [email protected] (M.R.) Received: 14 June 2020; Accepted: 16 July 2020; Published: 23 July 2020 Abstract: Folates are a group of B9 vitamins playing an important role in many metabolic processes such as methylation reactions, nucleotide synthesis or oxidation and reduction processes. However, humans are not able to synthesize folates de novo and thus rely on external sources thereof. Baker’s yeast (Saccharomyces cerevisiae) has been shown to produce high amounts of this vitamin but extensive identification of its folate metabolism is still lacking. Therefore, we optimized and compared different sample preparation and purification procedures applying solid phase extraction (SPE). Strong anion exchange (SAX), C18 and hydrophilic–lipophilic-balanced (HLB) materials were tested for their applicability in future metabolomics studies. SAX turned out to be the preferred material for the quantitative purification of folates. Qualification of several folate vitamers was achieved by ultra-high pressure liquid chromatography quadrupole time of flight mass spectrometry (UHPLC-Q-ToF-MS) measurements and quantification was performed by liquid chromatography tandem mass spectrometry (LC-MS/MS) applying stable isotope dilution assays (SIDAs). -

1 Supplemental Information Development of an in Vitro Human
Supplemental Information Development of an In Vitro Human Liver System for Interrogating Non-Alcoholic Steatohepatitis Ryan Feaver1, Banumathi K. Cole1, Mark J. Lawson1, Stephen A. Hoang1, Svetlana Marukian1, Robert A. Figler1, Arun J. Sanyal2, Brian R. Wamhoff*1, Ajit Dash1 1HemoShear Therapeutics LLC, Charlottesville, VA 2Virginia Commonwealth University School of Medicine Richmond, VA *Corresponding Author: Brian R. Wamhoff, 501 Locust Ave., Charlottesville, VA 22902 [email protected] 434-872-0196 1 Supplemental Figures and Tables: log2 Fold Change Values ● ● ● ● ● ● ● ● 5 ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●● ● ● ● ● ● ● ● ● ● ● ● ●● ● ● ● ● ● ● ● ● ● ● ● ● ● ●● ● ● ● ●● ● ● ● ● ● ● ●● ● ● ● ●●●● ●● ● ● ● ● ●●● ● ● ● ● ●● ●●●● ●●●●●● ● ● ● ● ● ●● ● ● ● ● ●● ●●●●●●●●●●●●●●●● ● ● ● ● ● ●●● ●●●●●●●●●●●●●● ● ● ● ●●●●●●●●●●●●●●●●● ● ●● ● ● ●●● ●● ●●●●●●●● ●●●●●●●●●●● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●● ● ● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ●● ●●● ● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ● ● ● ● ●●●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●●● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●● ● ● ● ● ●● ●● ● ●●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●●●●●● ● ● ●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ●●● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ● ● ● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ● ●● ●●●●●●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ●●● ●●●● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● ● ● ●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●●● -

Serum Levels of Lycopene, Beta-Carotene, and Retinol and Their Correlation with Sperm DNA Damage in Normospermic and Infertile Men
Int J Reprod BioMed Vol. 13. No. 12. pp: 787-792, December 2015 Original article Serum levels of lycopene, beta-carotene, and retinol and their correlation with sperm DNA damage in normospermic and infertile men Taiebeh Ghyasvand1 M.Sc., Mohammad Taghi Goodarzi2 Ph.D., Iraj Amiri3 Ph.D., Jamshid Karimi1 Ph.D., Marzieh Ghorbani3 M.Sc. 1. Department of Clinical Abstract Biochemistry, Hamadan University of Medical Sciences, Background: Oxidative stress in reproductive system leads to sperm DNA damage Hamadan, Iran. and sperm membrane lipid peroxidation and may play an important role in the 2. Research Center for Molecular pathogenesis of male infertility, especially in idiopathic cases. Antioxidants such as Medicine, Hamadan University carotenoids function against free radical damages. of Medical Sciences, Hamadan, Iran. Objective: The aim of this study was to determine the levels of lycopene, beta- 3. Endometer and Endometriosis carotene and retinol in serum and their relationship with sperm DNA damage and Centre, Fatemieh Hospital, lipid peroxidation in infertile and normospermic males. Hamadan University of Medical Materials and Methods: Sixty two infertile men and 71 normospermic men Sciences, Hamadan, Iran. participated in this study. Blood and semen samples were collected from all subjects. Sperm DNA damage was measured using TUNEL method. Carotenoids, retinol, and malonedildehyde in serum were also determined. Results: DNA fragmentation was higher in infertile group comparing to control group. Serum levels of lycopene, beta-carotene and, vitamin A in infertile men were significantly lower than normospermic men (p< 0.001, =0.005, and =0.003 respectively). While serum MDA was not significantly different between two groups, MDA in seminal plasma of infertile men was significantly higher than Corresponding Author: Mohammad Taghi Goodarzi, control group (p< 0.001).