Lipid Myopathies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Targeted Genes and Methodology Details for Neuromuscular Genetic Panels
Targeted Genes and Methodology Details for Neuromuscular Genetic Panels Reference transcripts based on build GRCh37 (hg19) interrogated by Neuromuscular Genetic Panels Next-generation sequencing (NGS) and/or Sanger sequencing is performed Motor Neuron Disease Panel to test for the presence of a mutation in these genes. Gene GenBank Accession Number Regions of homology, high GC-rich content, and repetitive sequences may ALS2 NM_020919 not provide accurate sequence. Therefore, all reported alterations detected ANG NM_001145 by NGS are confirmed by an independent reference method based on laboratory developed criteria. However, this does not rule out the possibility CHMP2B NM_014043 of a false-negative result in these regions. ERBB4 NM_005235 Sanger sequencing is used to confirm alterations detected by NGS when FIG4 NM_014845 appropriate.(Unpublished Mayo method) FUS NM_004960 HNRNPA1 NM_031157 OPTN NM_021980 PFN1 NM_005022 SETX NM_015046 SIGMAR1 NM_005866 SOD1 NM_000454 SQSTM1 NM_003900 TARDBP NM_007375 UBQLN2 NM_013444 VAPB NM_004738 VCP NM_007126 ©2018 Mayo Foundation for Medical Education and Research Page 1 of 14 MC4091-83rev1018 Muscular Dystrophy Panel Muscular Dystrophy Panel Gene GenBank Accession Number Gene GenBank Accession Number ACTA1 NM_001100 LMNA NM_170707 ANO5 NM_213599 LPIN1 NM_145693 B3GALNT2 NM_152490 MATR3 NM_199189 B4GAT1 NM_006876 MYH2 NM_017534 BAG3 NM_004281 MYH7 NM_000257 BIN1 NM_139343 MYOT NM_006790 BVES NM_007073 NEB NM_004543 CAPN3 NM_000070 PLEC NM_000445 CAV3 NM_033337 POMGNT1 NM_017739 CAVIN1 NM_012232 POMGNT2 -

Mechanistic Studies on Medium Chain Acyl-Coa Dehydrogenase
Acyl-CoA Dehydrogenases: Mechanistic studies on Medium Chain Acyl-CoA Dehydrogenase Dissertation zur Erlangung des akademischen Grades des Doktors der Naturwissenschaften (Dr. rer. nat.) an der Universität Konstanz (Fachbereich Biologie) vorgelegt von Vasile Robert Gradinaru Konstanz, im Juni 2005 Tag der mündlichen Prüfung : 9. November 2005 Referent: Prof. Dr. Sandro Ghisla Referent: Prof. Dr. Peter Macheroux Acknowledgements I am greatly indebted to my supervisor, Prof. Dr. Sandro Ghisla, for his advice and support. He has been an excellent supervisor providing insightful comments and constructive criticism throughout this PhD project. I would also like to thank my colleagues in the Universities of Konstanz and Iasi for their advice, encouragement and friendship, without which I would certainly not have completed this thesis. In particular, I would like to thank Prof. Dr. Richard Schowen, Prof. Dr. Peter Macheroux, Prof. Dr. Colin Thorpe, Prof. Dr. Jung-Ja. Kim, Prof. Dr. Tatiana Nicolaescu, Prof. Dr. Constantin Ciugureanu, Prof. Dr. Robert Bach, Dr. Olga Dmitrenko, Susanne Feindler-Boeckh, Gudrun Vogt, Elmi Leisner, Karl Janko, Lili Smau, Nasser Ibrahim, Phaneeswara Rao Kommoju, Sudarshan Rao Ande, Lakshminarayana Kaza, Cosmin Pocanschi, Paula Bulieris for their active interest during the course of this project. My gratitude also goes to Prof. Alexandru Cecal for encouraging me to embark on this PhD. I express my loving thanks to my wife Luiza whose love, support, patience and understanding made this work easier. Above all, I wish to express my sincerest gratitude to my parents, who made my studies possible and who have always encouraged me. This study was financiarlly supported by the Deutsche Forschungsgemeinschaft (Gh 2/6-4). -
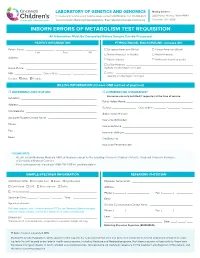
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

ACADS Rabbit Pab
Leader in Biomolecular Solutions for Life Science ACADS Rabbit pAb Catalog No.: A0945 2 Publications Basic Information Background Catalog No. This gene encodes a tetrameric mitochondrial flavoprotein, which is a member of the A0945 acyl-CoA dehydrogenase family. This enzyme catalyzes the initial step of the mitochondrial fatty acid beta-oxidation pathway. Mutations in this gene have been Observed MW associated with short-chain acyl-CoA dehydrogenase (SCAD) deficiency. Alternative 44kDa splicing results in two variants which encode different isoforms. Calculated MW 44kDa Category Primary antibody Applications WB, IHC, IF Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 35 P16219 IHC 1:50 - 1:100 Immunogen 1:50 - 1:200 IF Recombinant fusion protein containing a sequence corresponding to amino acids 1-260 of human ACADS (NP_000008.1). Synonyms ACADS;ACAD3;SCAD Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using ACADS antibody (A0945) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Detection: ECL Basic Kit (RM00020). Exposure time: 15s. Immunohistochemistry of paraffin- Immunohistochemistry of paraffin- Immunofluorescence analysis of U2OS embedded human liver cancer using embedded human liver damage using cells using ACADS antibody (A0945). Blue: ACADS antibody (A0945) at dilution of ACADS antibody (A0945) at dilution of DAPI for nuclear staining. -

Positive Carrier Sample Report
RESULTS RECIPIENT FEMALE MALE UNIVERSITY MEDICAL CENTER JANE MILLER N/A Attn: Dr. Paul Smith DOB: 11/11/1977 123 Main Street Ethnicity: Northern European City, CA 10231 Sample Type: OG-510 Saliva Phone: (800) 555-1212 Date of Collection: 02/06/2020 Fax: (800) 555-1212 Date Received: 02/16/2020 NPI: 4253506008 Date Tested: 02/16/2020 Report Date: 02/18/2020 Barcode: 55200006634190 Accession ID: FAKERQSCARFAF Indication: Screening for genetic disease carrier status Foresight® Carrier Screen POSITIVE: CARRIER ABOUT THIS TEST The Myriad Foresight Carrier Screen utilizes sequencing, maximizing coverage across all DNA regions tested, to help you learn about your chance to have a child with a genetic disease. RESULTS SUMMARY Risk Details JANE MILLER Partner Panel Information Foresight Carrier Screen N/A Universal Panel Fundamental Plus Panel Fundamental Panel Fragile X Syndrome (176 conditions tested) POSITIVE: CARRIER CARRIER* The reproductive risk presented Smith‑Lemli‑Opitz Syndrome NM_001360.2(DHCR7):c. is based on a hypothetical 964-1G>C(aka IVS8-1G>C) pairing with a partner of the Reproductive Risk: 1 in 380 heterozygote same ethnic group. Carrier Inheritance: Autosomal Recessive testing should be considered. See "Next Steps". *Carriers generally do not experience symptoms. No disease-causing mutations were detected in any other gene tested. A complete list of all conditions tested can be found on page 6. Additional Findings Single Carrier Autosomal recessive additional findings CLINICAL NOTES NEXT STEPS • None • Carrier testing should be considered for the diseases specified above for the patient's partner, as both parents must be carriers before a child is at high risk of developing the disease. -
Deciphering the Gene Expression Profile of Peroxisome Proliferator
Chen et al. J Transl Med (2016) 14:157 DOI 10.1186/s12967-016-0871-3 Journal of Translational Medicine RESEARCH Open Access Deciphering the gene expression profile of peroxisome proliferator‑activated receptor signaling pathway in the left atria of patients with mitral regurgitation Mien‑Cheng Chen1*, Jen‑Ping Chang2, Yu‑Sheng Lin3, Kuo‑Li Pan3, Wan‑Chun Ho1, Wen‑Hao Liu1, Tzu‑Hao Chang4, Yao‑Kuang Huang5, Chih‑Yuan Fang1 and Chien‑Jen Chen1 Abstract Background: Differentially expressed genes in the left atria of mitral regurgitation (MR) pigs have been linked to peroxisome proliferator-activated receptor (PPAR) signaling pathway in the KEGG pathway. However, specific genes of the PPAR signaling pathway in the left atria of MR patients have never been explored. Methods: This study enrolled 15 MR patients with heart failure, 7 patients with aortic valve disease and heart failure, and 6 normal controls. We used PCR assay (84 genes) for PPAR pathway and quantitative RT-PCR to study specific genes of the PPAR pathway in the left atria. Results: Gene expression profiling analysis through PCR assay identified 23 genes to be differentially expressed in the left atria of MR patients compared to normal controls. The expressions of APOA1, ACADM, FABP3, ETFDH, ECH1, CPT1B, CPT2, SLC27A6, ACAA2, SMARCD3, SORBS1, EHHADH, SLC27A1, PPARGC1B, PPARA and CPT1A were significantly up-regulated, whereas the expression of PLTP was significantly down-regulated in the MR patients compared to normal controls. The expressions of HMGCS2, ACADM, FABP3, MLYCD, ECH1, ACAA2, EHHADH, CPT1A and PLTP were significantly up-regulated in the MR patients compared to patients with aortic valve disease. -

NICU Gene List Generator.Xlsx
Neonatal Crisis Sequencing Panel Gene List Genes: A2ML1 - B3GLCT A2ML1 ADAMTS9 ALG1 ARHGEF15 AAAS ADAMTSL2 ALG11 ARHGEF9 AARS1 ADAR ALG12 ARID1A AARS2 ADARB1 ALG13 ARID1B ABAT ADCY6 ALG14 ARID2 ABCA12 ADD3 ALG2 ARL13B ABCA3 ADGRG1 ALG3 ARL6 ABCA4 ADGRV1 ALG6 ARMC9 ABCB11 ADK ALG8 ARPC1B ABCB4 ADNP ALG9 ARSA ABCC6 ADPRS ALK ARSL ABCC8 ADSL ALMS1 ARX ABCC9 AEBP1 ALOX12B ASAH1 ABCD1 AFF3 ALOXE3 ASCC1 ABCD3 AFF4 ALPK3 ASH1L ABCD4 AFG3L2 ALPL ASL ABHD5 AGA ALS2 ASNS ACAD8 AGK ALX3 ASPA ACAD9 AGL ALX4 ASPM ACADM AGPS AMELX ASS1 ACADS AGRN AMER1 ASXL1 ACADSB AGT AMH ASXL3 ACADVL AGTPBP1 AMHR2 ATAD1 ACAN AGTR1 AMN ATL1 ACAT1 AGXT AMPD2 ATM ACE AHCY AMT ATP1A1 ACO2 AHDC1 ANK1 ATP1A2 ACOX1 AHI1 ANK2 ATP1A3 ACP5 AIFM1 ANKH ATP2A1 ACSF3 AIMP1 ANKLE2 ATP5F1A ACTA1 AIMP2 ANKRD11 ATP5F1D ACTA2 AIRE ANKRD26 ATP5F1E ACTB AKAP9 ANTXR2 ATP6V0A2 ACTC1 AKR1D1 AP1S2 ATP6V1B1 ACTG1 AKT2 AP2S1 ATP7A ACTG2 AKT3 AP3B1 ATP8A2 ACTL6B ALAS2 AP3B2 ATP8B1 ACTN1 ALB AP4B1 ATPAF2 ACTN2 ALDH18A1 AP4M1 ATR ACTN4 ALDH1A3 AP4S1 ATRX ACVR1 ALDH3A2 APC AUH ACVRL1 ALDH4A1 APTX AVPR2 ACY1 ALDH5A1 AR B3GALNT2 ADA ALDH6A1 ARFGEF2 B3GALT6 ADAMTS13 ALDH7A1 ARG1 B3GAT3 ADAMTS2 ALDOB ARHGAP31 B3GLCT Updated: 03/15/2021; v.3.6 1 Neonatal Crisis Sequencing Panel Gene List Genes: B4GALT1 - COL11A2 B4GALT1 C1QBP CD3G CHKB B4GALT7 C3 CD40LG CHMP1A B4GAT1 CA2 CD59 CHRNA1 B9D1 CA5A CD70 CHRNB1 B9D2 CACNA1A CD96 CHRND BAAT CACNA1C CDAN1 CHRNE BBIP1 CACNA1D CDC42 CHRNG BBS1 CACNA1E CDH1 CHST14 BBS10 CACNA1F CDH2 CHST3 BBS12 CACNA1G CDK10 CHUK BBS2 CACNA2D2 CDK13 CILK1 BBS4 CACNB2 CDK5RAP2 -

AGPAT2 Gene 1-Acylglycerol-3-Phosphate O-Acyltransferase 2
AGPAT2 gene 1-acylglycerol-3-phosphate O-acyltransferase 2 Normal Function The AGPAT2 gene provides instructions for making an enzyme that is found in many of the body's cells and tissues. It plays a critical role in the growth and development of adipocytes, which are cells that store fats for energy. Adipocytes are the major component of the body's fatty (adipose) tissue. The AGPAT2 enzyme is part of a chemical pathway in many cells that produces two important types of fats (lipids): glycerophospholipids and triacylglycerols. Glycerophospholipids are the major component of cell membranes and are involved in chemical signaling within cells. Triacylglycerols (also known as triglycerides) are fat molecules that are stored in adipocytes for later conversion to energy. The AGPAT2 enzyme is responsible for a particular chemical reaction in the production of these two types of lipids. Specifically, the enzyme helps convert a molecule called lysophosphatidic acid (LPA) to another molecule, phosphatidic acid (PA). Additional reactions convert phosphatidic acid to glycerophospholipids and triacylglycerols. Health Conditions Related to Genetic Changes Congenital generalized lipodystrophy At least 26 mutations in the AGPAT2 gene have been identified in people with congenital generalized lipodystrophy (also called Berardinelli-Seip congenital lipodystrophy) type 1. This rare condition is characterized by an almost total absence of adipose tissue and a very muscular appearance. A shortage of adipose tissue leads to multiple health problems, including high levels of triglycerides circulating in the bloodstream (hypertriglyceridemia) and diabetes mellitus. The AGPAT2 gene mutations that cause congenital generalized lipodystrophy type 1 greatly reduce or eliminate the activity of the AGPAT2 enzyme. -

The Metabolic Serine Hydrolases and Their Functions in Mammalian Physiology and Disease Jonathan Z
REVIEW pubs.acs.org/CR The Metabolic Serine Hydrolases and Their Functions in Mammalian Physiology and Disease Jonathan Z. Long* and Benjamin F. Cravatt* The Skaggs Institute for Chemical Biology and Department of Chemical Physiology, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, California 92037, United States CONTENTS 2.4. Other Phospholipases 6034 1. Introduction 6023 2.4.1. LIPG (Endothelial Lipase) 6034 2. Small-Molecule Hydrolases 6023 2.4.2. PLA1A (Phosphatidylserine-Specific 2.1. Intracellular Neutral Lipases 6023 PLA1) 6035 2.1.1. LIPE (Hormone-Sensitive Lipase) 6024 2.4.3. LIPH and LIPI (Phosphatidic Acid-Specific 2.1.2. PNPLA2 (Adipose Triglyceride Lipase) 6024 PLA1R and β) 6035 2.1.3. MGLL (Monoacylglycerol Lipase) 6025 2.4.4. PLB1 (Phospholipase B) 6035 2.1.4. DAGLA and DAGLB (Diacylglycerol Lipase 2.4.5. DDHD1 and DDHD2 (DDHD Domain R and β) 6026 Containing 1 and 2) 6035 2.1.5. CES3 (Carboxylesterase 3) 6026 2.4.6. ABHD4 (Alpha/Beta Hydrolase Domain 2.1.6. AADACL1 (Arylacetamide Deacetylase-like 1) 6026 Containing 4) 6036 2.1.7. ABHD6 (Alpha/Beta Hydrolase Domain 2.5. Small-Molecule Amidases 6036 Containing 6) 6027 2.5.1. FAAH and FAAH2 (Fatty Acid Amide 2.1.8. ABHD12 (Alpha/Beta Hydrolase Domain Hydrolase and FAAH2) 6036 Containing 12) 6027 2.5.2. AFMID (Arylformamidase) 6037 2.2. Extracellular Neutral Lipases 6027 2.6. Acyl-CoA Hydrolases 6037 2.2.1. PNLIP (Pancreatic Lipase) 6028 2.6.1. FASN (Fatty Acid Synthase) 6037 2.2.2. PNLIPRP1 and PNLIPR2 (Pancreatic 2.6.2. -

Chain Acyl-Coa Dehydrogenase (Mcad) Deficiency
EXPLORING THERAPEUTIC APPROACHES FOR TREATMENT OF MEDIUM- CHAIN ACYL-COA DEHYDROGENASE (MCAD) DEFICIENCY by Heejung Kang BS, Sungkyunkwan University, South Korea, 2003 MS, Sungkyunkwan University, South Korea, 2005 MS, University of Minnesota, 2008 Submitted to the Graduate Faculty of Graduate School of Public Health in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2014 UNIVERSITY OF PITTSBURGH GRADUATE SCHOOL OF PUBLIC HEALTH This dissertation was presented by Heejung Kang It was defended on April 15, 2014 and approved by Dissertation Advisor: Jerry Vockley, M.D. Ph.D., Professor, Pediatrics, School of Medicine, University of Pittsburgh Committee Chair: Robert Ferrell, Ph.D., Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh David Finegold, Ph.D., Professor, Pediatrics, School of Medicine, University of Pittsburgh Al-Walid A. Mohsen, Ph.D., Research Associate Professor of Pediatrics School of Medicine, University of Pittsburgh Zsolt Urban, Ph.D., Associate Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh ii Copyright © by Heejung Kang 2014 iii Jerry Vockley, MD, PhD EXPLORING THERAPEUTIC APPROACHES FOR TREATMENT OF MEDIUM- CHAIN ACYL-COA DEHYDROGENASE (MCAD) DEFICIENCY Heejung Kang, PhD University of Pittsburgh, 2014 ABSTRACT Medium chain acyl-CoA dehydrogenase deficiency (MCADD) is a common biochemical genetic disorder in the US. Nearly 90% of alleles from MCADD patients contain a common mutation in the ACADM (c.985A>G). The change replaces a lysine with a glutamate (K304E), causing improper folding. The K304E protein can fold to a mature form and is then stable and active when expressed in a prokaryotic system with molecular chaperonins. -

Biomolecules
biomolecules Article The Vitamin D Receptor Regulates Glycerolipid and Phospholipid Metabolism in Human Hepatocytes Teresa Martínez-Sena 1, Polina Soluyanova 1, Carla Guzmán 1, José Manuel Valdivielso 2 , José Vicente Castell 1,3,4 and Ramiro Jover 1,3,4,* 1 Experimental Hepatology Unit, IIS Hospital La Fe, 46026 Valencia, Spain; [email protected] (T.M.-S.); [email protected] (P.S.); [email protected] (C.G.); [email protected] (J.V.C.) 2 Vascular and Renal Translational Research Group, Experimental Medicine Department, IRBLleida, 25196 Lleida, Spain; [email protected] 3 Departamento de Bioquímica y Biología Molecular, Facultad de Medicina, Universidad de Valencia, 46010 Valencia, Spain 4 Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas (CIBERehd), ISCIII, 28029 Madrid, Spain * Correspondence: [email protected]; Tel.: +34-96124-6653 Received: 21 February 2020; Accepted: 20 March 2020; Published: 24 March 2020 Abstract: The vitamin D receptor (VDR) must be relevant to liver lipid metabolism because VDR deficient mice are protected from hepatosteatosis. Therefore, our objective was to define the role of VDR on the overall lipid metabolism in human hepatocytes. We developed an adenoviral vector for human VDR and performed transcriptomic and metabolomic analyses of cultured human hepatocytes upon VDR activation by vitamin D (VitD). Twenty percent of the VDR responsive genes were related to lipid metabolism, including MOGAT1, LPGAT1, AGPAT2, and DGAT1 (glycerolipid metabolism); CDS1, PCTP, and MAT1A (phospholipid metabolism); and FATP2, SLC6A12, and AQP3 (uptake of fatty acids, betaine, and glycerol, respectively). They were rapidly induced (4–6 h) upon VDR activation by 10 nM VitD or 100 µM lithocholic acid (LCA). -

Thiazolidinediones Upregulate Fatty Acid Uptake and Oxidation in Adipose Tissue of Diabetic Patients Guenther Boden,1,2 Carol Homko,2 Maria Mozzoli,1,2 Louise C
Thiazolidinediones Upregulate Fatty Acid Uptake and Oxidation in Adipose Tissue of Diabetic Patients Guenther Boden,1,2 Carol Homko,2 Maria Mozzoli,1,2 Louise C. Showe,3 Calen Nichols,3 and Peter Cheung1,2 Thiazolidinediones (TZDs) are a new class of insulin- TZDs produce insulin sensitization, which takes place sensitizing drugs. To explore how and in which tissues primarily in skeletal muscle (6). Lowering plasma free they improve insulin action, we obtained fat and muscle fatty acid (FFA) levels improves insulin sensitivity (7). The biopsies from eight patients with type 2 diabetes before well-established TZD lowering of plasma FFAs has there- -fore been widely considered to be a major factor respon (5 ؍ and 2 months after treatment with rosiglitazone (n ,TZD treatment was associated sible for their insulin sensitizing effect (8–12). It is .(3 ؍ or troglitazone (n with a coordinated upregulation in the expression of however, not clear how TZDs lower FFA levels. Since they genes and synthesis of proteins involved in fatty acid  seem to have little or no effect on basal rates of lipolysis uptake, binding, -oxidation and electron transport, (11,13,14), the decrease in plasma FFA levels is probably and oxidative phosphorylation in subcutaneous fat but not in skeletal muscle. These changes were accompa- due to an increase in FFA clearance (oxidation and/or nied by a 13% increase in total body fat oxidation, a 20% esterification). Supporting this notion, we have recently decrease in plasma free fatty acid levels, and a 46% found that TZD-induced lowering of plasma FFAs was increase in insulin-stimulated glucose uptake.