Chain Acyl-Coa Dehydrogenase (Mcad) Deficiency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
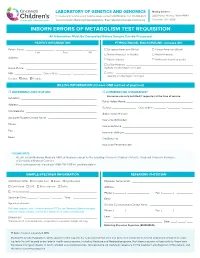
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

Genes Investigated
BabyNEXTTM EXTENDED Investigated genes and associated diseases Gene Disease OMIM OMIM Condition RUSP gene Disease ABCC8 Familial hyperinsulinism 600509 256450 Metabolic disorder - ABCC8-related Inborn error of amino acid metabolism ABCD1 Adrenoleukodystrophy 300371 300100 Miscellaneous RUSP multisystem (C) * diseases ABCD4 Methylmalonic aciduria and 603214 614857 Metabolic disorder - homocystinuria, cblJ type Inborn error of amino acid metabolism ACAD8 Isobutyryl-CoA 604773 611283 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of (S) ** organic acid metabolism ACAD9 acyl-CoA dehydrogenase-9 611103 611126 Metabolic Disorder - (ACAD9) deficiency Inborn error of fatty acid metabolism ACADM Acyl-CoA dehydrogenase, 607008 201450 Metabolic Disorder - RUSP medium chain, deficiency of Inborn error of fatty (C) acid metabolism ACADS Acyl-CoA dehydrogenase, 606885 201470 Metabolic Disorder - RUSP short-chain, deficiency of Inborn error of fatty (S) acid metabolism ACADSB 2-methylbutyrylglycinuria 600301 610006 Metabolic Disorder - RUSP Inborn error of (S) organic acid metabolism ACADVL very long-chain acyl-CoA 609575 201475 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of fatty (C) acid metabolism ACAT1 Alpha-methylacetoacetic 607809 203750 Metabolic Disorder - RUSP aciduria Inborn error of (C) organic acid metabolism ACSF3 Combined malonic and 614245 614265 Metabolic Disorder - methylmalonic aciduria Inborn error of organic acid metabolism 1 ADA Severe combined 608958 102700 Primary RUSP immunodeficiency due -
Deciphering the Gene Expression Profile of Peroxisome Proliferator
Chen et al. J Transl Med (2016) 14:157 DOI 10.1186/s12967-016-0871-3 Journal of Translational Medicine RESEARCH Open Access Deciphering the gene expression profile of peroxisome proliferator‑activated receptor signaling pathway in the left atria of patients with mitral regurgitation Mien‑Cheng Chen1*, Jen‑Ping Chang2, Yu‑Sheng Lin3, Kuo‑Li Pan3, Wan‑Chun Ho1, Wen‑Hao Liu1, Tzu‑Hao Chang4, Yao‑Kuang Huang5, Chih‑Yuan Fang1 and Chien‑Jen Chen1 Abstract Background: Differentially expressed genes in the left atria of mitral regurgitation (MR) pigs have been linked to peroxisome proliferator-activated receptor (PPAR) signaling pathway in the KEGG pathway. However, specific genes of the PPAR signaling pathway in the left atria of MR patients have never been explored. Methods: This study enrolled 15 MR patients with heart failure, 7 patients with aortic valve disease and heart failure, and 6 normal controls. We used PCR assay (84 genes) for PPAR pathway and quantitative RT-PCR to study specific genes of the PPAR pathway in the left atria. Results: Gene expression profiling analysis through PCR assay identified 23 genes to be differentially expressed in the left atria of MR patients compared to normal controls. The expressions of APOA1, ACADM, FABP3, ETFDH, ECH1, CPT1B, CPT2, SLC27A6, ACAA2, SMARCD3, SORBS1, EHHADH, SLC27A1, PPARGC1B, PPARA and CPT1A were significantly up-regulated, whereas the expression of PLTP was significantly down-regulated in the MR patients compared to normal controls. The expressions of HMGCS2, ACADM, FABP3, MLYCD, ECH1, ACAA2, EHHADH, CPT1A and PLTP were significantly up-regulated in the MR patients compared to patients with aortic valve disease. -

CDH12 Cadherin 12, Type 2 N-Cadherin 2 RPL5 Ribosomal
5 6 6 5 . 4 2 1 1 1 2 4 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 2 2 A A A A A A A A A A A A A A A A A A A A C C C C C C C C C C C C C C C C C C C C R R R R R R R R R R R R R R R R R R R R B , B B B B B B B B B B B B B B B B B B B , 9 , , , , 4 , , 3 0 , , , , , , , , 6 2 , , 5 , 0 8 6 4 , 7 5 7 0 2 8 9 1 3 3 3 1 1 7 5 0 4 1 4 0 7 1 0 2 0 6 7 8 0 2 5 7 8 0 3 8 5 4 9 0 1 0 8 8 3 5 6 7 4 7 9 5 2 1 1 8 2 2 1 7 9 6 2 1 7 1 1 0 4 5 3 5 8 9 1 0 0 4 2 5 0 8 1 4 1 6 9 0 0 6 3 6 9 1 0 9 0 3 8 1 3 5 6 3 6 0 4 2 6 1 0 1 2 1 9 9 7 9 5 7 1 5 8 9 8 8 2 1 9 9 1 1 1 9 6 9 8 9 7 8 4 5 8 8 6 4 8 1 1 2 8 6 2 7 9 8 3 5 4 3 2 1 7 9 5 3 1 3 2 1 2 9 5 1 1 1 1 1 1 5 9 5 3 2 6 3 4 1 3 1 1 4 1 4 1 7 1 3 4 3 2 7 6 4 2 7 2 1 2 1 5 1 6 3 5 6 1 3 6 4 7 1 6 5 1 1 4 1 6 1 7 6 4 7 e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e e l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l l p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p p m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m m -

Dietary Amylose:Amylopectin Ratio Influences the Expression of Amino Acid Transporters and Enzyme Activities for Amino Acid Meta
Downloaded from British Journal of Nutrition, page 1 of 11 doi:10.1017/S0007114521002087 https://www.cambridge.org/core © The Author(s), 2021. Published by Cambridge University Press on behalf of The Nutrition Society. This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited. Dietary amylose:amylopectin ratio influences the expression of amino acid transporters and enzyme activities for amino acid metabolism in the gastrointestinal tract of goats . IP address: 170.106.202.226 Xiaokang Lv1,2, Chuanshe Zhou1,2*, Tao Ran3, Jinzhen Jiao1, Yong Liu1, Zhiliang Tan1, Shaoxun Tang1, Jinhe Kang1, Jingjing Xie1, Liang Chen1, Ao Ren4, Qixiang Xv1,2 and Zhiwei Kong1 1CAS Key Laboratory of Agro-ecological Processes in Subtropical Region, National Engineering Laboratory for Pollution Control and Waste Utilization in Livestock and Poultry Production, Hunan Provincial Key Laboratory of Animal Nutrition & Physiology , on and Metabolism, Institute of Subtropical Agriculture, the Chinese Academy of Sciences, Changsha 410125, People’s Republic of 28 Sep 2021 at 13:00:40 China 2University of Chinese Academy of Sciences, Beijing 100049, People’s Republic of China 3College of Pastoral Agriculture Science and Technology, Lanzhou University, Lanzhou 730020, People’s Republic of China 4Department of Animal Science and Technology, University of Hunan Agricultural University, Changsha 410128, People’s Republic of China , subject to the Cambridge Core terms of use, available at (Submitted 12 March 2021 – Final revision received 25 May 2021 – Accepted 8 June 2021) Abstract This study was designed to investigate the effects of dietary starch structure on muscle protein synthesis and gastrointestinal amino acid (AA) transport and metabolism of goats. -

Supplementary Materials
Supplementary Materials COMPARATIVE ANALYSIS OF THE TRANSCRIPTOME, PROTEOME AND miRNA PROFILE OF KUPFFER CELLS AND MONOCYTES Andrey Elchaninov1,3*, Anastasiya Lokhonina1,3, Maria Nikitina2, Polina Vishnyakova1,3, Andrey Makarov1, Irina Arutyunyan1, Anastasiya Poltavets1, Evgeniya Kananykhina2, Sergey Kovalchuk4, Evgeny Karpulevich5,6, Galina Bolshakova2, Gennady Sukhikh1, Timur Fatkhudinov2,3 1 Laboratory of Regenerative Medicine, National Medical Research Center for Obstetrics, Gynecology and Perinatology Named after Academician V.I. Kulakov of Ministry of Healthcare of Russian Federation, Moscow, Russia 2 Laboratory of Growth and Development, Scientific Research Institute of Human Morphology, Moscow, Russia 3 Histology Department, Medical Institute, Peoples' Friendship University of Russia, Moscow, Russia 4 Laboratory of Bioinformatic methods for Combinatorial Chemistry and Biology, Shemyakin-Ovchinnikov Institute of Bioorganic Chemistry of the Russian Academy of Sciences, Moscow, Russia 5 Information Systems Department, Ivannikov Institute for System Programming of the Russian Academy of Sciences, Moscow, Russia 6 Genome Engineering Laboratory, Moscow Institute of Physics and Technology, Dolgoprudny, Moscow Region, Russia Figure S1. Flow cytometry analysis of unsorted blood sample. Representative forward, side scattering and histogram are shown. The proportions of negative cells were determined in relation to the isotype controls. The percentages of positive cells are indicated. The blue curve corresponds to the isotype control. Figure S2. Flow cytometry analysis of unsorted liver stromal cells. Representative forward, side scattering and histogram are shown. The proportions of negative cells were determined in relation to the isotype controls. The percentages of positive cells are indicated. The blue curve corresponds to the isotype control. Figure S3. MiRNAs expression analysis in monocytes and Kupffer cells. Full-length of heatmaps are presented. -

Term Description FDR Matching Proteins in the Network Metabolic Pathways 2.40E-81 AADAT,AASS,ABAT,ACAA2, ACADL, ACADM, ACADS, AC
Term description FDR Matching proteins in the network Metabolic pathways 2.40e-81 AADAT,AASS,ABAT,ACAA2, ACADL, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACO2, ACOT1, ACOT2, ACOX1, ACSL5, ACSL6, ACSM1, ACSM3, ACSM5, ACSS2, ACSS3, AGMAT, AGXT2, AK4, ALAS1, ALDH1B1, ALDH2, ALDH4A1, ALDH5A1, ALDH6A1, ALDOB, AMACR, AMT, APRT, ARG1, ATP5A1, ATP5B, ATP5C1, ATP5E, ATP5F1, ATP5H, ATP5J, ATP5L, ATP5O, AUH, BCKDHA, BDH1, CHDH, COX4I1, COX7C, CPS1, CS, CYCS, CYP1A2, CYP27A1, DBT, DHRS4, DLAT, DLD, DLST, DMGDH, ECHS1, EHHADH, ENO1, EPHX2, FAHD1, FASN, FDPS, FECH, FH, GBE1, GCDH, GLDC, GLS, GLS2, GLUD1, GOT2, GPAM, GPI, GPT2, H6PD, HADH, HADHA, HADHB, HIBADH, HIBCH, HMGCL, HMGCS2, HSD17B10, HSD17B12, IDH1, IDH2, IDH3A, IDH3G, IVD, MCCC1, MCCC2, MCEE, MDH2, ME1, ME3, MECR, MLYCD, MMAB, MPST, MT-ATP8, MTHFD1L, MUT, NDUFA10, NDUFA12, NDUFA13, NDUFA2, NDUFA5, NDUFA7, NDUFA9, NDUFAB1, NDUFB11, NDUFB3, NDUFS1, NDUFS2, NDUFS3, NDUFS6, NDUFS7, NDUFS8, NDUFV1, NDUFV2, NDUFV3, NNT, OAT, OGDH, OTC, OXSM, PC, PCCA, PCCB, PDHA1, PDHB, PDHX, PRODH2, PYCR2, PYGL, SARDH, SDHA, SDHB, SHMT2, SLC27A5, SUCLA2, SUCLG1, SUCLG2, TST, UGP2, UQCRC2, UQCRFS1, UQCRQ Carbon metabolism 4.12e-43 ACADM, ACADS, ACAT1, ACO2, ACSS2, ALDH6A1, ALDOB, AMT, CAT, CPS1, CS, DLAT, DLD, DLST, ECHS1, EHHADH, ENO1, FH, GLDC, GLUD1, GOT2, GPI, GPT2, H6PD, HADHA, HIBCH, IDH1, IDH2, IDH3A, IDH3G, MCEE, MDH2, ME1, ME2, ME3, MUT, OGDH, PC, PCCA, PCCB, PDHA1, PDHB, SDHA, SDHB, SHMT2, SUCLA2, SUCLG1, SUCLG2 Valine, leucine, and isoleucine degradation 1.44e-33 ABAT, ACAA2, ACADM, ACADS, ACADSB, ACAT1, ACSF3, -

Thiazolidinediones Upregulate Fatty Acid Uptake and Oxidation in Adipose Tissue of Diabetic Patients Guenther Boden,1,2 Carol Homko,2 Maria Mozzoli,1,2 Louise C
Thiazolidinediones Upregulate Fatty Acid Uptake and Oxidation in Adipose Tissue of Diabetic Patients Guenther Boden,1,2 Carol Homko,2 Maria Mozzoli,1,2 Louise C. Showe,3 Calen Nichols,3 and Peter Cheung1,2 Thiazolidinediones (TZDs) are a new class of insulin- TZDs produce insulin sensitization, which takes place sensitizing drugs. To explore how and in which tissues primarily in skeletal muscle (6). Lowering plasma free they improve insulin action, we obtained fat and muscle fatty acid (FFA) levels improves insulin sensitivity (7). The biopsies from eight patients with type 2 diabetes before well-established TZD lowering of plasma FFAs has there- -fore been widely considered to be a major factor respon (5 ؍ and 2 months after treatment with rosiglitazone (n ,TZD treatment was associated sible for their insulin sensitizing effect (8–12). It is .(3 ؍ or troglitazone (n with a coordinated upregulation in the expression of however, not clear how TZDs lower FFA levels. Since they genes and synthesis of proteins involved in fatty acid  seem to have little or no effect on basal rates of lipolysis uptake, binding, -oxidation and electron transport, (11,13,14), the decrease in plasma FFA levels is probably and oxidative phosphorylation in subcutaneous fat but not in skeletal muscle. These changes were accompa- due to an increase in FFA clearance (oxidation and/or nied by a 13% increase in total body fat oxidation, a 20% esterification). Supporting this notion, we have recently decrease in plasma free fatty acid levels, and a 46% found that TZD-induced lowering of plasma FFAs was increase in insulin-stimulated glucose uptake. -

Identification of Isobutyryl-Coa Dehydrogenase and Its Deficiency
Molecular Genetics and Metabolism 77 (2002) 68–79 www.academicpress.com Identification of isobutyryl-CoA dehydrogenase and its deficiency in humans Tien V. Nguyen,a Brage S. Andresen,b,c Thomas J. Corydon,b Sandro Ghisla,d Nasser Abd-El Razik,d Al-Walid A. Mohsen,a Stephen D. Cederbaum,e Diane S. Roe,f Charles R. Roe,f Nicolas J. Lench,g and Jerry Vockleya,* a Department of Medical Genetics, Mayo Clinic, Rochester, MN 55905, USA b Institute for Human Genetics, Aarhus University, Aarhus, Denmark c Research Unit for Molecular Medicine, Skejby Sygehus and Aarhus University, Aarhus, Denmark d Faculty of Biology, University of Konstanz, Konstanz, Germany e Department of Pediatrics, UCLA Medical Center, Los Angeles, CA, USA f Institute of Metabolic Disease, Baylor University, Dallas, TX, USA g Molecular Medicine Unit, University of Leeds, St. JamesÕ University Hospital, Leeds, UK Received 19 July 2002; received in revised form 31 July 2002; accepted 1 August 2002 Abstract The acyl-CoA dehydrogenases (ACDs) are a family of related enzymes that catalyze the a,b-dehydrogenation of acyl-CoA esters. Two homologues active in branched chain amino acid metabolism have previously been identified. We have used expression in Escherichia coli to produce a previously uncharacterized ACD-like sequence (ACAD8) and define its substrate specificity. Purified À1 À1 recombinant enzyme had a kcat=Km of 0.8, 0.23, and 0.04 (lM s ) with isobutyryl-CoA, (S) 2-methylbutyryl-CoA, and n-propionyl- CoA, respectively, as substrates. Thus, this enzyme is an isobutyryl-CoA dehydrogenase. A single patient has previously been described whose fibroblasts exhibit a specific deficit in the oxidation of valine. -

Activation of Pparα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis
Tohoku J. Exp. Med., 2016, 240, 113-122PPARα Activation in Cells due to VLCAD Deficiency 113 Activation of PPARα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis * * Yang Yang,1, Yuyao Feng,1, Xiaowei Zhang,2 Takero Nakajima,1 Naoki Tanaka,1 Eiko Sugiyama,3 Yuji Kamijo4 and Toshifumi Aoyama1 1Department of Metabolic Regulation, Shinshu University Graduate School of Medicine, Matsumoto, Nagano, Japan 2Department of Neurosurgery, The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, China 3Department of Nutritional Science, Nagano Prefectural College, Nagano, Nagano, Japan 4Department of Nephrology, Shinshu University School of Medicine, Matsumoto, Nagano, Japan Very-long-chain acyl-CoA dehydrogenase (VLCAD) catalyzes the first reaction in the mitochondrial fatty acid β-oxidation pathway. VLCAD deficiency is associated with the accumulation of fat in multiple organs and tissues, which results in specific clinical features including cardiomyopathy, cardiomegaly, muscle weakness, and hepatic dysfunction in infants. We speculated that the abnormal fatty acid metabolism in VLCAD-deficient individuals might cause cell necrosis by fatty acid toxicity. The accumulation of fatty acids may activate peroxisome proliferator-activated receptor (PPAR), a master regulator of fatty acid metabolism and a potent nuclear receptor for free fatty acids. We examined six skin fibroblast lines, derived from VLCAD-deficient patients and identified fatty acid accumulation and PPARα activation in these cell lines. We then found that the expression levels of three enzymes involved in fatty acid degradation, including long-chain acyl-CoA synthetase (LACS), were increased in a PPARα-dependent manner. This increased expression of LACS might enhance the fatty acyl-CoA supply to fatty acid degradation and sulfatide synthesis pathways. -

Common Genetic Variants in the Vitamin D Pathway Including Genome-Wide Associated Variants Are Not Associated with Breast Cancer Risk Among Chinese Women
Author Manuscript Published OnlineFirst on August 9, 2011; DOI: 10.1158/1055-9965.EPI-11-0704 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Null Results in Brief Common genetic variants in the vitamin D pathway including genome-wide associated variants are not associated with breast cancer risk among Chinese women Tsogzolmaa Dorjgochoo1, Ryan Delahanty1, Wei Lu2, Jirong Long1, Qiuyin Cai1, Ying Zheng2, Kai Gu2, Yu-Tang Gao3, Wei Zheng1, Xiao Ou Shu1 1Division of Epidemiology, Department of Medicine, Vanderbilt Epidemiology Center, and Vanderbilt-Ingram Cancer Center, Vanderbilt University School of Medicine, Nashville, TN 37232, USA 2Shanghai Center for Disease Control and Prevention, Shanghai, China 3Department of Epidemiology, Shanghai Cancer Institute, Shanghai, China Running title: Vitamin D pathway gene polymorphisms and breast cancer risk Keywords: breast cancer, risk, polymorphisms, vitamin D pathway genes, 25(OH)D, GWAS. Financial Support: This research was supported by USPHS grants R01CA064277, R01CA090899, and R01CA124558. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. Sample preparation and genotyping assays, using Affymetrix arrays, were conducted at the Survey and Biospecimen Shared Resource and the Vanderbilt Microarray Shared Resource, respectively, which are supported in part by the Vanderbilt-Ingram Cancer Center (P30CA68485). Corresponding author: Xiao Ou Shu Professor of Medicine Vanderbilt Epidemiology Center Vanderbilt Ingram-Cancer Center Vanderbilt University 2525 West End Avenue, 6th Floor Nashville, TN 37203, USA Tel: 615-936-0713 Fax: 615-936-8291 Email: [email protected] Conflicts of Interest: No potential conflicts of interest. -

Ab118182 – Fatty Acid Oxidation Human In-Cell ELISA
ab118182 – Fatty Acid Oxidation Human In-Cell ELISA Kit (ACADVL, ACADM, HADHA) Instructions for Use For measuring in high throughput very long chain specific acyl-CoA dehydrogenase, medium-chain specific acyl-CoA dehydrogenase and long-chain 3-hydroxyl-CoA dehydrogenase This product is for research use only and is not intended for diagnostic use. 1 Table of Contents 1. Introduction 3 2. Assay Summary 6 3. Kit Contents 7 4. Storage and Handling 7 5. Additional Materials Required 8 6. Preparation of Reagents 8 7. Sample Preparation 9 8. Assay Procedure 11 9. Data Analysis 14 10. Assay Performance and Specificity 14 11. Frequently Asked Questions 18 12. Troubleshooting 21 2 1. Introduction Principle: ab118182 uses quantitative immunocytochemistry to measure protein levels or post-translational modifications in cultured cells. Cells are fixed in a microplate and targets of interest are detected with highly specific, well-characterized monoclonal antibodies, and levels are quantified with IRDye®-labeled Secondary Antibodies. IR imaging and quantitation is performed using a LI- COR® Odyssey® or Aerius® system. Background: The Fatty acid B-oxidation (FAO) pathway is a key metabolic pathway that plays an important role in energy homeostasis particularly in organs such as the liver, heart and skeletal muscle. Oxidation of fatty acids occurs inside the mitochondria where acyl-CoA esters (activated fatty acids) of various lengths are shortened into units of acetyl-CoA each time a cycle is fully completed. Each unit of acetyl-CoA is then oxidized by the mitochondria into CO 2 and H 2O via the citric acid cycle and the mitochondria respiratory chain.