Development of a Targeted Second-Tier Genetic Test For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DBT Gene Dihydrolipoamide Branched Chain Transacylase E2
DBT gene dihydrolipoamide branched chain transacylase E2 Normal Function The DBT gene provides instructions for making part of a group of enzymes called the branched-chain alpha-keto acid dehydrogenase (BCKD) enzyme complex. Specifically, the protein produced from the DBT gene forms a critical piece of the enzyme complex called the E2 component. The BCKD enzyme complex is responsible for one step in the normal breakdown of three protein building blocks (amino acids). These amino acids—leucine, isoleucine, and valine—are obtained from the diet. They are present in many kinds of food, particularly protein-rich foods such as milk, meat, and eggs. The BCKD enzyme complex is active in mitochondria, which are specialized structures inside cells that serve as energy-producing centers. The breakdown of leucine, isoleucine, and valine produces molecules that can be used for energy. Health Conditions Related to Genetic Changes Maple syrup urine disease More than 70 mutations in the DBT gene have been identified in people with maple syrup urine disease, most often in individuals with mild variants of the disorder. These variant forms become apparent later in infancy or childhood, and they lead to delayed development and other health problems if not treated. Mutations in the DBT gene include changes in single DNA building blocks (base pairs) and insertions or deletions of a small amount of DNA in the DBT gene. These changes disrupt the normal function of the E2 component, preventing the BCKD enzyme complex from effectively breaking down leucine, isoleucine, and valine. As a result, these amino acids and their byproducts build up in the body. -
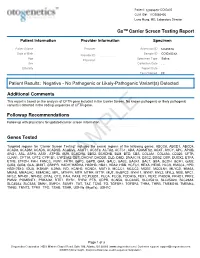
PDF Document Created by Pdffiller
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -

Thiamine Dependency and Related Gene Mutations: Recent Aspects
Int J Anal Bio-Sci Vol. 3, No 4 (2015) 〈Review Article〉 Thiamine dependency and related gene mutations: recent aspects Sachiko Kiuchi1, Hiroshi Ihara1, Yoshikazu Nishiguchi2, Nobue Ito3, Hiromitsu Yokota3 and Naotaka Hashizume4 Summary Thiamine dependency is an inherited metabolic disorder from which patients exhibit severe symptoms of deficiency, although they are fed more than the normal requirement of this vitamin. Deficiency symptoms can be treated with pharmacologic doses of thiamine as high as 100 to 1,000 times the Dietary Reference Values. Thiamine dependency is nowadays classified as a disorder caused by genetic mutations affecting thiamine-dependent enzymes or thiamine transporter, which transports thiamine to cells. The former mutation on enzyme is known as a pyruvate dehydrogenase complex deficiency (i.e., congenital lactic acidemia and Leigh syndrome) and a deficiency in branched- chain α-ketoacid dehydrogenase complex (i.e., maple syrup urine disease). The latter are known as mutations in thiamine transporter gene that makes protein transporting thiamine into cells (encoded by SLC19A2 and SLC19A3 genes) and protein transporting thiamine diphosphate into the mitochon- dria (encoded by SLC25A19 gene). Thiamine-responsive megaloblastic anemia (TRMA), an autosomal recessive disease, is caused by loss of functional mutation in the SLC19A2 (ThTr-1). Key words: Vitamin B1 dependency, Thiamine deficiency, Maple syrup urine disease, Megaloblastic anemia, Thiamine transporter 1. Introduction the normal daily requirement from diets, dietary supplements, or intravenous dosage. The deficiency To maintain normal carbohydrate metabolism in symptoms were better treated by taking amounts of the body, we have to ingest thiamine from our diet. thiamine 100-fold greater or more than that of the The daily required amounts are 1.4 mg (4.2 µmol) for daily requirement, but the symptoms would reappear men and 1.1 mg (3.3 µmol) for women for Japanese if the treatment was stopped4. -

Upregulation of Peroxisome Proliferator-Activated Receptor-Α And
Upregulation of peroxisome proliferator-activated receptor-α and the lipid metabolism pathway promotes carcinogenesis of ampullary cancer Chih-Yang Wang, Ying-Jui Chao, Yi-Ling Chen, Tzu-Wen Wang, Nam Nhut Phan, Hui-Ping Hsu, Yan-Shen Shan, Ming-Derg Lai 1 Supplementary Table 1. Demographics and clinical outcomes of five patients with ampullary cancer Time of Tumor Time to Age Differentia survival/ Sex Staging size Morphology Recurrence recurrence Condition (years) tion expired (cm) (months) (months) T2N0, 51 F 211 Polypoid Unknown No -- Survived 193 stage Ib T2N0, 2.41.5 58 F Mixed Good Yes 14 Expired 17 stage Ib 0.6 T3N0, 4.53.5 68 M Polypoid Good No -- Survived 162 stage IIA 1.2 T3N0, 66 M 110.8 Ulcerative Good Yes 64 Expired 227 stage IIA T3N0, 60 M 21.81 Mixed Moderate Yes 5.6 Expired 16.7 stage IIA 2 Supplementary Table 2. Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis of an ampullary cancer microarray using the Database for Annotation, Visualization and Integrated Discovery (DAVID). This table contains only pathways with p values that ranged 0.0001~0.05. KEGG Pathway p value Genes Pentose and 1.50E-04 UGT1A6, CRYL1, UGT1A8, AKR1B1, UGT2B11, UGT2A3, glucuronate UGT2B10, UGT2B7, XYLB interconversions Drug metabolism 1.63E-04 CYP3A4, XDH, UGT1A6, CYP3A5, CES2, CYP3A7, UGT1A8, NAT2, UGT2B11, DPYD, UGT2A3, UGT2B10, UGT2B7 Maturity-onset 2.43E-04 HNF1A, HNF4A, SLC2A2, PKLR, NEUROD1, HNF4G, diabetes of the PDX1, NR5A2, NKX2-2 young Starch and sucrose 6.03E-04 GBA3, UGT1A6, G6PC, UGT1A8, ENPP3, MGAM, SI, metabolism -

Downloaded from GEO
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Oxylipin metabolism is controlled by mitochondrial b-oxidation during bacterial inflammation. Mariya Misheva1, Konstantinos Kotzamanis1*, Luke C Davies1*, Victoria J Tyrrell1, Patricia R S Rodrigues1, Gloria A Benavides2, Christine Hinz1, Robert C Murphy3, Paul Kennedy4, Philip R Taylor1,5, Marcela Rosas1, Simon A Jones1, Sumukh Deshpande1, Robert Andrews1, Magdalena A Czubala1, Mark Gurney1, Maceler Aldrovandi1, Sven W Meckelmann1, Peter Ghazal1, Victor Darley-Usmar2, Daniel White1, and Valerie B O’Donnell1 1Systems Immunity Research Institute and Division of Infection and Immunity, and School of Medicine, Cardiff University, UK, 2Department of Pathology, University of Alabama at Birmingham, Birmingham, AL 35294, USA, 3Department of Pharmacology, University of Colorado Denver, Aurora, CO 80045, USA, 4Cayman Chemical 1180 E Ellsworth Rd, Ann Arbor, MI 48108, United States, 5UK Dementia Research Institute at Cardiff, Cardiff University, UK Address correspondence: Valerie O’Donnell, [email protected] or Daniel White, [email protected], Systems Immunity Research Institute, Cardiff University *Both authors contributed equally to the study 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Maple Syrup Urine Disease with a Novel DBT Gene Mutation Wei Feng1, Jinfu Jia1, Heyang Guan2 and Qing Tian3*
Feng et al. BMC Pediatrics (2019) 19:494 https://doi.org/10.1186/s12887-019-1880-1 CASE REPORT Open Access Case report: maple syrup urine disease with a novel DBT gene mutation Wei Feng1, Jinfu Jia1, Heyang Guan2 and Qing Tian3* Abstract Background: Maple syrup urine disease (MSUD) is a potentially life-threatening metabolic disorder caused by decreased activity of the branched-chain α-ketoacid dehydrogenase (BCKD) complex. Mutations in four genes (BCKDHA, BCKDHB, DLD and DBT) are associated with MSUD. Here, the presenting symptoms and clinical course of a case of MSUD with a novel DBT gene mutation are described. Case presentation: We describe an infant with MSUD with the DBT gene mutation who had drowsiness and poor appetite as well as abnormal findings upon head magnetic resonance imaging (MRI), plasma amino acid analysis and urine organic acid analysis. Genetic testing revealed that both parents had the heterozygous mutation c.1132C > T (p.378X) in chr1:100672078, and the patient had the homozygous mutations c.1132C > T (p.378X) in chr1:100672078. Once diagnosed with MSUD, the patient’s disease was controlled with a diet of BCAA-free enteral formula and thiamine. Conclusion: The mutation c.1132C > T (p.378X) is a novel DBT gene mutation that is associated with MSUD and always has mild clinical manifestations. After timely BCAA-free nutrition and supplementation with thiamine for the patient, the plasma levels of BCAAs reached a safe level, the abnormal range of the multiple intracranial abnormalities was significantly smaller than before, and the symptoms of drowsiness and poor appetite disappeared. -

Mechanistic Studies on Medium Chain Acyl-Coa Dehydrogenase
Acyl-CoA Dehydrogenases: Mechanistic studies on Medium Chain Acyl-CoA Dehydrogenase Dissertation zur Erlangung des akademischen Grades des Doktors der Naturwissenschaften (Dr. rer. nat.) an der Universität Konstanz (Fachbereich Biologie) vorgelegt von Vasile Robert Gradinaru Konstanz, im Juni 2005 Tag der mündlichen Prüfung : 9. November 2005 Referent: Prof. Dr. Sandro Ghisla Referent: Prof. Dr. Peter Macheroux Acknowledgements I am greatly indebted to my supervisor, Prof. Dr. Sandro Ghisla, for his advice and support. He has been an excellent supervisor providing insightful comments and constructive criticism throughout this PhD project. I would also like to thank my colleagues in the Universities of Konstanz and Iasi for their advice, encouragement and friendship, without which I would certainly not have completed this thesis. In particular, I would like to thank Prof. Dr. Richard Schowen, Prof. Dr. Peter Macheroux, Prof. Dr. Colin Thorpe, Prof. Dr. Jung-Ja. Kim, Prof. Dr. Tatiana Nicolaescu, Prof. Dr. Constantin Ciugureanu, Prof. Dr. Robert Bach, Dr. Olga Dmitrenko, Susanne Feindler-Boeckh, Gudrun Vogt, Elmi Leisner, Karl Janko, Lili Smau, Nasser Ibrahim, Phaneeswara Rao Kommoju, Sudarshan Rao Ande, Lakshminarayana Kaza, Cosmin Pocanschi, Paula Bulieris for their active interest during the course of this project. My gratitude also goes to Prof. Alexandru Cecal for encouraging me to embark on this PhD. I express my loving thanks to my wife Luiza whose love, support, patience and understanding made this work easier. Above all, I wish to express my sincerest gratitude to my parents, who made my studies possible and who have always encouraged me. This study was financiarlly supported by the Deutsche Forschungsgemeinschaft (Gh 2/6-4). -
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

ACADS Rabbit Pab
Leader in Biomolecular Solutions for Life Science ACADS Rabbit pAb Catalog No.: A0945 2 Publications Basic Information Background Catalog No. This gene encodes a tetrameric mitochondrial flavoprotein, which is a member of the A0945 acyl-CoA dehydrogenase family. This enzyme catalyzes the initial step of the mitochondrial fatty acid beta-oxidation pathway. Mutations in this gene have been Observed MW associated with short-chain acyl-CoA dehydrogenase (SCAD) deficiency. Alternative 44kDa splicing results in two variants which encode different isoforms. Calculated MW 44kDa Category Primary antibody Applications WB, IHC, IF Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 35 P16219 IHC 1:50 - 1:100 Immunogen 1:50 - 1:200 IF Recombinant fusion protein containing a sequence corresponding to amino acids 1-260 of human ACADS (NP_000008.1). Synonyms ACADS;ACAD3;SCAD Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using ACADS antibody (A0945) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Detection: ECL Basic Kit (RM00020). Exposure time: 15s. Immunohistochemistry of paraffin- Immunohistochemistry of paraffin- Immunofluorescence analysis of U2OS embedded human liver cancer using embedded human liver damage using cells using ACADS antibody (A0945). Blue: ACADS antibody (A0945) at dilution of ACADS antibody (A0945) at dilution of DAPI for nuclear staining. -

Genes Investigated
BabyNEXTTM EXTENDED Investigated genes and associated diseases Gene Disease OMIM OMIM Condition RUSP gene Disease ABCC8 Familial hyperinsulinism 600509 256450 Metabolic disorder - ABCC8-related Inborn error of amino acid metabolism ABCD1 Adrenoleukodystrophy 300371 300100 Miscellaneous RUSP multisystem (C) * diseases ABCD4 Methylmalonic aciduria and 603214 614857 Metabolic disorder - homocystinuria, cblJ type Inborn error of amino acid metabolism ACAD8 Isobutyryl-CoA 604773 611283 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of (S) ** organic acid metabolism ACAD9 acyl-CoA dehydrogenase-9 611103 611126 Metabolic Disorder - (ACAD9) deficiency Inborn error of fatty acid metabolism ACADM Acyl-CoA dehydrogenase, 607008 201450 Metabolic Disorder - RUSP medium chain, deficiency of Inborn error of fatty (C) acid metabolism ACADS Acyl-CoA dehydrogenase, 606885 201470 Metabolic Disorder - RUSP short-chain, deficiency of Inborn error of fatty (S) acid metabolism ACADSB 2-methylbutyrylglycinuria 600301 610006 Metabolic Disorder - RUSP Inborn error of (S) organic acid metabolism ACADVL very long-chain acyl-CoA 609575 201475 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of fatty (C) acid metabolism ACAT1 Alpha-methylacetoacetic 607809 203750 Metabolic Disorder - RUSP aciduria Inborn error of (C) organic acid metabolism ACSF3 Combined malonic and 614245 614265 Metabolic Disorder - methylmalonic aciduria Inborn error of organic acid metabolism 1 ADA Severe combined 608958 102700 Primary RUSP immunodeficiency due -
Deciphering the Gene Expression Profile of Peroxisome Proliferator
Chen et al. J Transl Med (2016) 14:157 DOI 10.1186/s12967-016-0871-3 Journal of Translational Medicine RESEARCH Open Access Deciphering the gene expression profile of peroxisome proliferator‑activated receptor signaling pathway in the left atria of patients with mitral regurgitation Mien‑Cheng Chen1*, Jen‑Ping Chang2, Yu‑Sheng Lin3, Kuo‑Li Pan3, Wan‑Chun Ho1, Wen‑Hao Liu1, Tzu‑Hao Chang4, Yao‑Kuang Huang5, Chih‑Yuan Fang1 and Chien‑Jen Chen1 Abstract Background: Differentially expressed genes in the left atria of mitral regurgitation (MR) pigs have been linked to peroxisome proliferator-activated receptor (PPAR) signaling pathway in the KEGG pathway. However, specific genes of the PPAR signaling pathway in the left atria of MR patients have never been explored. Methods: This study enrolled 15 MR patients with heart failure, 7 patients with aortic valve disease and heart failure, and 6 normal controls. We used PCR assay (84 genes) for PPAR pathway and quantitative RT-PCR to study specific genes of the PPAR pathway in the left atria. Results: Gene expression profiling analysis through PCR assay identified 23 genes to be differentially expressed in the left atria of MR patients compared to normal controls. The expressions of APOA1, ACADM, FABP3, ETFDH, ECH1, CPT1B, CPT2, SLC27A6, ACAA2, SMARCD3, SORBS1, EHHADH, SLC27A1, PPARGC1B, PPARA and CPT1A were significantly up-regulated, whereas the expression of PLTP was significantly down-regulated in the MR patients compared to normal controls. The expressions of HMGCS2, ACADM, FABP3, MLYCD, ECH1, ACAA2, EHHADH, CPT1A and PLTP were significantly up-regulated in the MR patients compared to patients with aortic valve disease.