Thiazolidinediones Upregulate Fatty Acid Uptake and Oxidation in Adipose Tissue of Diabetic Patients Guenther Boden,1,2 Carol Homko,2 Maria Mozzoli,1,2 Louise C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
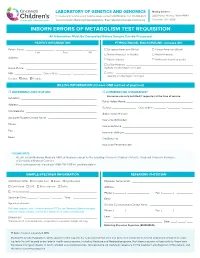
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -
Deciphering the Gene Expression Profile of Peroxisome Proliferator
Chen et al. J Transl Med (2016) 14:157 DOI 10.1186/s12967-016-0871-3 Journal of Translational Medicine RESEARCH Open Access Deciphering the gene expression profile of peroxisome proliferator‑activated receptor signaling pathway in the left atria of patients with mitral regurgitation Mien‑Cheng Chen1*, Jen‑Ping Chang2, Yu‑Sheng Lin3, Kuo‑Li Pan3, Wan‑Chun Ho1, Wen‑Hao Liu1, Tzu‑Hao Chang4, Yao‑Kuang Huang5, Chih‑Yuan Fang1 and Chien‑Jen Chen1 Abstract Background: Differentially expressed genes in the left atria of mitral regurgitation (MR) pigs have been linked to peroxisome proliferator-activated receptor (PPAR) signaling pathway in the KEGG pathway. However, specific genes of the PPAR signaling pathway in the left atria of MR patients have never been explored. Methods: This study enrolled 15 MR patients with heart failure, 7 patients with aortic valve disease and heart failure, and 6 normal controls. We used PCR assay (84 genes) for PPAR pathway and quantitative RT-PCR to study specific genes of the PPAR pathway in the left atria. Results: Gene expression profiling analysis through PCR assay identified 23 genes to be differentially expressed in the left atria of MR patients compared to normal controls. The expressions of APOA1, ACADM, FABP3, ETFDH, ECH1, CPT1B, CPT2, SLC27A6, ACAA2, SMARCD3, SORBS1, EHHADH, SLC27A1, PPARGC1B, PPARA and CPT1A were significantly up-regulated, whereas the expression of PLTP was significantly down-regulated in the MR patients compared to normal controls. The expressions of HMGCS2, ACADM, FABP3, MLYCD, ECH1, ACAA2, EHHADH, CPT1A and PLTP were significantly up-regulated in the MR patients compared to patients with aortic valve disease. -

Chain Acyl-Coa Dehydrogenase (Mcad) Deficiency
EXPLORING THERAPEUTIC APPROACHES FOR TREATMENT OF MEDIUM- CHAIN ACYL-COA DEHYDROGENASE (MCAD) DEFICIENCY by Heejung Kang BS, Sungkyunkwan University, South Korea, 2003 MS, Sungkyunkwan University, South Korea, 2005 MS, University of Minnesota, 2008 Submitted to the Graduate Faculty of Graduate School of Public Health in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2014 UNIVERSITY OF PITTSBURGH GRADUATE SCHOOL OF PUBLIC HEALTH This dissertation was presented by Heejung Kang It was defended on April 15, 2014 and approved by Dissertation Advisor: Jerry Vockley, M.D. Ph.D., Professor, Pediatrics, School of Medicine, University of Pittsburgh Committee Chair: Robert Ferrell, Ph.D., Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh David Finegold, Ph.D., Professor, Pediatrics, School of Medicine, University of Pittsburgh Al-Walid A. Mohsen, Ph.D., Research Associate Professor of Pediatrics School of Medicine, University of Pittsburgh Zsolt Urban, Ph.D., Associate Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh ii Copyright © by Heejung Kang 2014 iii Jerry Vockley, MD, PhD EXPLORING THERAPEUTIC APPROACHES FOR TREATMENT OF MEDIUM- CHAIN ACYL-COA DEHYDROGENASE (MCAD) DEFICIENCY Heejung Kang, PhD University of Pittsburgh, 2014 ABSTRACT Medium chain acyl-CoA dehydrogenase deficiency (MCADD) is a common biochemical genetic disorder in the US. Nearly 90% of alleles from MCADD patients contain a common mutation in the ACADM (c.985A>G). The change replaces a lysine with a glutamate (K304E), causing improper folding. The K304E protein can fold to a mature form and is then stable and active when expressed in a prokaryotic system with molecular chaperonins. -

Activation of Pparα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis
Tohoku J. Exp. Med., 2016, 240, 113-122PPARα Activation in Cells due to VLCAD Deficiency 113 Activation of PPARα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis * * Yang Yang,1, Yuyao Feng,1, Xiaowei Zhang,2 Takero Nakajima,1 Naoki Tanaka,1 Eiko Sugiyama,3 Yuji Kamijo4 and Toshifumi Aoyama1 1Department of Metabolic Regulation, Shinshu University Graduate School of Medicine, Matsumoto, Nagano, Japan 2Department of Neurosurgery, The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, China 3Department of Nutritional Science, Nagano Prefectural College, Nagano, Nagano, Japan 4Department of Nephrology, Shinshu University School of Medicine, Matsumoto, Nagano, Japan Very-long-chain acyl-CoA dehydrogenase (VLCAD) catalyzes the first reaction in the mitochondrial fatty acid β-oxidation pathway. VLCAD deficiency is associated with the accumulation of fat in multiple organs and tissues, which results in specific clinical features including cardiomyopathy, cardiomegaly, muscle weakness, and hepatic dysfunction in infants. We speculated that the abnormal fatty acid metabolism in VLCAD-deficient individuals might cause cell necrosis by fatty acid toxicity. The accumulation of fatty acids may activate peroxisome proliferator-activated receptor (PPAR), a master regulator of fatty acid metabolism and a potent nuclear receptor for free fatty acids. We examined six skin fibroblast lines, derived from VLCAD-deficient patients and identified fatty acid accumulation and PPARα activation in these cell lines. We then found that the expression levels of three enzymes involved in fatty acid degradation, including long-chain acyl-CoA synthetase (LACS), were increased in a PPARα-dependent manner. This increased expression of LACS might enhance the fatty acyl-CoA supply to fatty acid degradation and sulfatide synthesis pathways. -

Ab118182 – Fatty Acid Oxidation Human In-Cell ELISA
ab118182 – Fatty Acid Oxidation Human In-Cell ELISA Kit (ACADVL, ACADM, HADHA) Instructions for Use For measuring in high throughput very long chain specific acyl-CoA dehydrogenase, medium-chain specific acyl-CoA dehydrogenase and long-chain 3-hydroxyl-CoA dehydrogenase This product is for research use only and is not intended for diagnostic use. 1 Table of Contents 1. Introduction 3 2. Assay Summary 6 3. Kit Contents 7 4. Storage and Handling 7 5. Additional Materials Required 8 6. Preparation of Reagents 8 7. Sample Preparation 9 8. Assay Procedure 11 9. Data Analysis 14 10. Assay Performance and Specificity 14 11. Frequently Asked Questions 18 12. Troubleshooting 21 2 1. Introduction Principle: ab118182 uses quantitative immunocytochemistry to measure protein levels or post-translational modifications in cultured cells. Cells are fixed in a microplate and targets of interest are detected with highly specific, well-characterized monoclonal antibodies, and levels are quantified with IRDye®-labeled Secondary Antibodies. IR imaging and quantitation is performed using a LI- COR® Odyssey® or Aerius® system. Background: The Fatty acid B-oxidation (FAO) pathway is a key metabolic pathway that plays an important role in energy homeostasis particularly in organs such as the liver, heart and skeletal muscle. Oxidation of fatty acids occurs inside the mitochondria where acyl-CoA esters (activated fatty acids) of various lengths are shortened into units of acetyl-CoA each time a cycle is fully completed. Each unit of acetyl-CoA is then oxidized by the mitochondria into CO 2 and H 2O via the citric acid cycle and the mitochondria respiratory chain. -
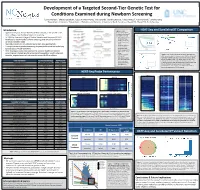
Development of a Targeted Second-Tier Genetic Test For
Development of a Targeted Second-Tier Genetic Test for Conditions Examined during Newborn Screening 1Lonna Mollison, 1Chelsea Gustafson, 1Edgar A Rivera-Munoz, 1Alicia Brandt, 1Daniela DeCristo, 1Falecia Metcalf, 2Cynthia Powell, 1Jonathan Berg 1Department of Genetics, 2Department of Pediatrics and Genetics, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina Introduction Figure 1. Library HEAT-Seq and SureSelectXT Comparison • Approximately four million children are born annually in the United States, preparation workflows for Agilent’s SureSelectXT most undergo state mandated newborn screening and Roche’s HEAT-Seq. A. B. C. • In 2006 the American College of Medical Genetics and Genomics (ACMG) • Time requirement for developed a recommended uniform screening panel (RUSP) to minimize SureSelectXT was about 32 hours, and variability between states for HEAT-Seq about 8 • Most RUSP conditions are detected by tandem mass spectrometry hours. • Recommended DNA • Through the use of genetic sequencing it is possible to detect the underlying input amount for genetic cause of RUSP conditions SureSelectXT was • Here we propose a step-wise approach to enhance traditional newborn about 3000ng, and for HEAT-Seq was about D. screening and integrate genetic screening into population health using cost- 250ng. effective, targeted sequencing to examine current RUSP conditions • Cost per sample for Figure 4. (A-C) The percent of bases at varying read depths for SureSelectXT HEAT-Seq and SureSelect when normalized to 5M reads (A), 50M (including all human reads (B) and 200M reads (C) for each of the 8 samples. (D) The exon baits) was about percent of targeted bases in all samples sequenced at 30 fold Core Condition Associated Gene(s) ACMG Code $333, and for HEAT- coverage were estimated normalizing the data to various values Maple Syrup Urine Disease BCKDHA, BCKDHB, DBT MSUD Seq (including MIPs) of sequenced reads. -

Differential Expression of Pparγ, FASN, and ACADM Genes In
10 Open Access Asian Australas. J. Anim. Sci. Vol. 27, No. 1 : 10-18 January 2014 http://dx.doi.org/10.5713/ajas.2013.13422 www.ajas.info pISSN 1011-2367 eISSN 1976-5517 Differential Expression of PPAR, FASN, and ACADM Genes in Various Adipose Tissues and Longissimus dorsi Muscle from Yanbian Yellow Cattle and Yan Yellow Cattle Shuang Ji1,2, Runjun Yang1, Chunyan Lu1, Zhengyan Qiu1, Changguo Yan2,*, and Zhihui Zhao1,* 1 College of Animal Science, Jilin Provincial Key Laboratory of Animal Embryo Engineering, Jilin University, 130062, Changchun, China ABSTRACT: The objective of this study was to investigate the correlation between cattle breeds and deposit of adipose tissues in different positions and the gene expressions of peroxisome proliferator-activated receptor gamma (PPAR), fatty acid synthase (FASN), and Acyl-CoA dehydrogenase (ACADM), which are associated with lipid metabolism and are valuable for understanding the physiology in fat depot and meat quality. Yanbian yellow cattle and Yan yellow cattle reared under the same conditions display different fat proportions in the carcass. To understand this difference, the expression of PPAR, FASN, and ACADM in different adipose tissues and longissimus dorsi muscle (LD) in these two breeds were analyzed using the Real-time quantitative polymerase chain reaction method (qRT-PCR). The result showed that PPAR gene expression was significantly higher in adipose tissue than in LD in both breeds. PPAR expression was also higher in abdominal fat, in perirenal fat than in the subcutaneous fat (p<0.05) in Yanbian yellow cattle, and was significantly higher in subcutaneous fat in Yan yellow cattle than that in Yanbian yellow cattle. -

Endoplasmic Reticulum Stress Protein GRP78 Modulates Lipid Metabolism to Control Drug Sensitivity and Antitumor Immunity in Breast Cancer Katherine L
Cancer Microenvironment and Immunology Research Endoplasmic Reticulum Stress Protein GRP78 Modulates Lipid Metabolism to Control Drug Sensitivity and Antitumor Immunity in Breast Cancer Katherine L. Cook1,2, David R. Soto-Pantoja1, Pamela A.G. Clarke2, M. Idalia Cruz2, Alan Zwart2, Anni Warri€ 2, Leena Hilakivi-Clarke2, David D. Roberts3, and Robert Clarke2 Abstract The unfolded protein response is an endoplasmic reticulum of GRP78-regulated metabolite changes by treating tumor-bear- stress pathway mediated by the protein chaperone glucose regu- ing mice with tamoxifen and/or linoleic acid. Tumors treated with lated-protein 78 (GRP78). Metabolic analysis of breast cancer linoleic acid plus tamoxifen exhibited reduced tumor area and cells shows that GRP78 silencing increases the intracellular con- tumor weight. Inhibition of either GRP78 or linoleic acid treat- centrations of essential polyunsaturated fats, including linoleic ment increased MCP-1 serum levels, decreased CD47 expression, acid. Accumulation of fatty acids is due to an inhibition of and increased macrophage infiltration, suggesting a novel role for mitochondrial fatty acid transport, resulting in a reduction GRP78 in regulating innate immunity. GRP78 control of fatty acid of fatty acid oxidation. These data suggest a novel role of oxidation may represent a new homeostatic function for GRP78. GRP78-mediating cellular metabolism. We validated the effect Cancer Res; 76(19); 5657–70. Ó2016 AACR. Introduction translocate to the Golgi complex where it is cleaved by site 1 and 2 proteases (S1P and S2P) to form the activated ATF6 Glucose-regulated protein 78 (GRP78) is a protein chaper- transcription factor. Activation of the UPR controls various cell onethatactsasamasterregulatoroftheunfoldedprotein signaling pathways, including cap-dependent protein transla- response (UPR; refs. -

Medium-Chain Acyl Coa Dehydrogenase Protects Mitochondria from Lipid Peroxidation in Glioblastoma
Author Manuscript Published OnlineFirst on May 26, 2021; DOI: 10.1158/2159-8290.CD-20-1437 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Medium-chain acyl CoA dehydrogenase protects mitochondria from lipid peroxidation in glioblastoma Francesca Puca1*, Fei Yu1, Caterina Bartolacci5, Piergiorgio Pettazzoni1, Alessandro Carugo2, Emmet Huang-Hobbs1, Jintan Liu1, Ciro Zanca2, Federica Carbone8, Edoardo Del Poggetto1, Joy Gumin3, Pushan Dasgupta1, Sahil Seth1,2, Sanjana Srinivasan1, Frederick F. Lang3, Erik P. Sulman4, Philip L. Lorenzi11, Lin Tan11, Mengrou Shan6, Zachary P. Tolstyka6, Maureen Kachman7, Li Zhang6, Sisi Gao8, Angela K. Deem2,8, Giannicola Genovese9, Pier Paolo Scaglioni5, Costas A. Lyssiotis6,10,12*, Andrea Viale1* and Giulio F. Draetta1* 1Department of Genomic Medicine, 2The Translational Research to Advance Therapeutics and Innovation in Oncology Platform, 3Department of Neurosurgery, 4Department of Radiation Oncology, 8Institute for Applied Cancer Science, 9Department of Genitourinary Medical Oncology, 11Metabolomics Core Facility, Department of Bioinformatics and Computational Biology, University of Texas MD Anderson Cancer Center, Houston, Texas, USA 5Department of Internal Medicine Division of Hematology & Oncology, University of Cincinnati, Cincinnati, OH, USA 6Department of Molecular and Integrative Physiology, 7Michigan Regional Comprehensive Metabolomics Resource Core, 10Department of Internal Medicine, Division of Gastroenterology and Hepatology, 12University -

Lipid Myopathies
Journal of Clinical Medicine Review Lipid Myopathies Elena Maria Pennisi 1,*, Matteo Garibaldi 2 and Giovanni Antonini 2 1 Unit of Neuromuscular Disorders, Neurology, San Filippo Neri Hospital, 00135 Rome, Italy 2 Unit of Neuromuscular Diseases, Department of Neurology, Mental Health and Sensory Organs (NESMOS), SAPIENZA University of Rome, Sant’ Andrea Hospital, 00189 Rome, Italy; [email protected] (M.G.); [email protected] (G.A.) * Correspondence: [email protected] or [email protected]; Tel.: +39-(06)-3306-2374 Received: 28 October 2018; Accepted: 17 November 2018; Published: 23 November 2018 Abstract: Disorders of lipid metabolism affect several tissues, including skeletal and cardiac muscle tissues. Lipid myopathies (LM) are rare multi-systemic diseases, which most often are due to genetic defects. Clinically, LM can have acute or chronic clinical presentation. Disease onset can occur in all ages, from early stages of life to late-adult onset, showing with a wide spectrum of clinical symptoms. Muscular involvement can be fluctuant or stable and can manifest as fatigue, exercise intolerance and muscular weakness. Muscular atrophy is rarely present. Acute muscular exacerbations, resulting in rhabdomyolysis crisis are triggered by several factors. Several classifications of lipid myopathies have been proposed, based on clinical involvement, biochemical defect or histopathological findings. Herein, we propose a full revision of all the main clinical entities of lipid metabolism disorders with a muscle involvement, also including some those disorders of fatty acid oxidation (FAO) with muscular symptoms not included among previous lipid myopathies classifications. Keywords: lipid myopathies; lipid storage disease; muscle lipidosis; lipid metabolism disorders; beta-oxidation defects; FAO defect; metabolic myopathies 1. -

Ab118183 Fatty Acid Oxidation Human Flow Cytometry Kit
Version 3 Last updated 17 January 2019 ab118183 Fatty Acid Oxidation Human Flow Cytometry Kit For the detection of key FAO enzymes (ACADVL, ACADM, HADHA) in live cells by flow cytometry. View kit datasheet: www.abcam.com/ab118183 (use www.abcam.cn/ab118183 for China, or www.abcam.co.jp/ab118183 for Japan) This product is for research use only and is not intended for diagnostic use. Copyright © 2019 Abcam. All rights reserved Table of Contents 1. Overview 1 2. Protocol Summary 4 3. Precautions 5 4. Storage and Stability 5 5. Limitations 6 6. Materials Supplied 6 7. Materials Required, Not Supplied 7 8. Technical Hints 8 9. Reagent Preparation 9 10. Assay Procedure 10 11. Data Analysis 13 12. Typical data 14 13. Assay Performance and Specificity 16 14. Troubleshooting 18 15. FAQs 19 16. Notes 20 Copyright © 2019 Abcam. All rights reserved 1. Overview Fatty Acid Oxidation Human Flow Cytometry Kit (ab118183) is a panel of antibodies against key enzymes of the mitochondrial fatty acid oxidation (FAO), specially designed to be used in flow cytometry. The kit measures the levels of three of the most studied enzymes in the FAO pathway: ACADVL (acyl-CoA dehydrogenase, very long chain specific), ACADM (acyl-CoA dehydrogenase, medium chain specific) and HADHA (long chain 3-hydroxyl-CoA dehydrogenase). The assay combines the power of single cell analysis obtained from flow cytometry with the specificity of antibody-based immunostaining to quantify protein levels in cultured cells. Cells are harvested and fixed/permeabilized in suspension and targets of interest are detected with highly specific monoclonal antibodies, which are detected in turn with fluorescently-labeled secondary antibodies. -

The Role of Acetyl-Coa Carboxylase Activity in Normal Liver Metabolism And
The role of acetyl-CoA carboxylase activity in normal liver metabolism and pathophysiology in the context of obesity and cancer Marin Elise Healy Austin, Texas MS, Biological and Physical Sciences, University of Virginia, 2013 MS, Exercise Science, The University of Texas at Austin, 2011 BS, Exercise Physiology, The University of Texas at San Antonio, 2008 A Dissertation Presented to the Graduate Faculty of the University of Virginia in Candidacy for the Degree of Doctor of Philosophy Department of Pharmacology University of Virginia August 2015 Kyle L. Hoehn, Ph.D. Ira G. Schulman, Ph.D. Norbert Leitinger, Ph.D. Adam N. Goldfarb, M.D. Marty W. Mayo, Ph.D. Jill K. Slack-Davis, Ph.D. David F. Kashatus, Ph.D. I ABSTRACT The liver has a high capacity to store excess nutrients, primarily in the form of fat. However, excess lipid deposition in the liver can be problematic, as it is associated with metabolic disorders including fatty liver disease, type II diabetes, and liver cancer. The acetyl-CoA carboxylase (ACC) enzymes are major regulators of liver lipid content by catalyzing the conversion of excess glucose in the liver to fat, and by inhibiting mitochondrial fat oxidation. Thus, the ACC enzymes are potential drug targets because altering their activity could correct disease states associated with excess fat deposition. Using mice with genetic inhibition of liver ACC activity, we have uncovered a novel role for these enzymes in regulating protein acetylation that contributes to broad changes in cellular metabolism. At the level of whole-body physiology, we found that when a source of dietary fat was absent, LDKO mice have increased glucose disposal into the liver, reduction of peripheral adiposity, and improved whole-body glucose tolerance compared to controls.