Abbreviations and Alternate Names for the Additional Newborn Screening Disorders
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Hyperammonemia in Review: Pathophysiology, Diagnosis, and Treatment
Pediatr Nephrol DOI 10.1007/s00467-011-1838-5 EDUCATIONAL REVIEW Hyperammonemia in review: pathophysiology, diagnosis, and treatment Ari Auron & Patrick D. Brophy Received: 23 September 2010 /Revised: 9 January 2011 /Accepted: 12 January 2011 # IPNA 2011 Abstract Ammonia is an important source of nitrogen and is the breakdown and catabolism of dietary and bodily proteins, required for amino acid synthesis. It is also necessary for respectively. In healthy individuals, amino acids that are not normal acid-base balance. When present in high concentra- needed for protein synthesis are metabolized in various tions, ammonia is toxic. Endogenous ammonia intoxication chemical pathways, with the rest of the nitrogen waste being can occur when there is impaired capacity of the body to converted to urea. Ammonia is important for normal animal excrete nitrogenous waste, as seen with congenital enzymatic acid-base balance. During exercise, ammonia is produced in deficiencies. A variety of environmental causes and medica- skeletal muscle from deamination of adenosine monophos- tions may also lead to ammonia toxicity. Hyperammonemia phate and amino acid catabolism. In the brain, the latter refers to a clinical condition associated with elevated processes plus the activity of glutamate dehydrogenase ammonia levels manifested by a variety of symptoms and mediate ammonia production. After formation of ammonium signs, including significant central nervous system (CNS) from glutamine, α-ketoglutarate, a byproduct, may be abnormalities. Appropriate and timely management requires a degraded to produce two molecules of bicarbonate, which solid understanding of the fundamental pathophysiology, are then available to buffer acids produced by dietary sources. differential diagnosis, and treatment approaches available. -

Inherited Metabolic Disease
Inherited metabolic disease Dr Neil W Hopper SRH Areas for discussion • Introduction to IEMs • Presentation • Initial treatment and investigation of IEMs • Hypoglycaemia • Hyperammonaemia • Other presentations • Management of intercurrent illness • Chronic management Inherited Metabolic Diseases • Result from a block to an essential pathway in the body's metabolism. • Huge number of conditions • All rare – very rare (except for one – 1:500) • Presentation can be non-specific so index of suspicion important • Mostly AR inheritance – ask about consanguinity Incidence (W. Midlands) • Amino acid disorders (excluding phenylketonuria) — 18.7 per 100,000 • Phenylketonuria — 8.1 per 100,000 • Organic acidemias — 12.6 per 100,000 • Urea cycle diseases — 4.5 per 100,000 • Glycogen storage diseases — 6.8 per 100,000 • Lysosomal storage diseases — 19.3 per 100,000 • Peroxisomal disorders — 7.4 per 100,000 • Mitochondrial diseases — 20.3 per 100,000 Pathophysiological classification • Disorders that result in toxic accumulation – Disorders of protein metabolism (eg, amino acidopathies, organic acidopathies, urea cycle defects) – Disorders of carbohydrate intolerance – Lysosomal storage disorders • Disorders of energy production, utilization – Fatty acid oxidation defects – Disorders of carbohydrate utilization, production (ie, glycogen storage disorders, disorders of gluconeogenesis and glycogenolysis) – Mitochondrial disorders – Peroxisomal disorders IMD presentations • ? IMD presentations • Screening – MCAD, PKU • Progressive unexplained neonatal -
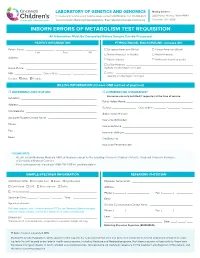
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

Summary Current Practices Report
18/10/2011 EU Tender “Evaluation of population newborn screening practices for rare disorders in Member States of the European Union” Short Executive Summary of the Report on the practices of newborn screening for rare disorders implemented in Member States of the European Union, Candidate, Potential Candidate and EFTA Countries Authors: Peter Burgard1, Martina Cornel2, Francesco Di Filippo4, Gisela Haege1, Georg F. Hoffmann1, Martin Lindner1, J. Gerard Loeber3, Tessel Rigter2, Kathrin Rupp1, 4 Domenica Taruscio4,Luciano Vittozzi , Stephanie Weinreich2 1 Department of Pediatrics , University Hospital - Heidelberg (DE) 2 VU University Medical Centre - Amsterdam (NL) 3 RIVM - Bilthoven (NL) 4 National Centre for Rare Diseases - Rome (IT) The opinions expressed in this document are those of the Contractor only and do not represent the official position of the Executive Agency for Health and Consumers. This work is funded by the European Union with a grant of Euro 399755 (Contract number 2009 62 06 of the Executive Agency for Health and Consumers) 1 18/10/2011 Abbreviations 3hmg 3-Hydroxy-3-methylglutaric aciduria 3mcc 3-Methylcrotonyl-CoA carboxylase deficiency/3-Methylglutacon aciduria/2-methyl-3-OH- butyric aciduria AAD Disorders of amino acid metabolism arg Argininemia asa Argininosuccinic aciduria bio Biotinidase deficiency bkt Beta-ketothiolase deficiency btha S, beta 0-thalassemia cah Congenital adrenal hyperplasia cf Cystic fibrosis ch Primary congenital hypothyroidism citI Citrullinemia type I citII Citrullinemia type II cpt I Carnitin -
Deciphering the Gene Expression Profile of Peroxisome Proliferator
Chen et al. J Transl Med (2016) 14:157 DOI 10.1186/s12967-016-0871-3 Journal of Translational Medicine RESEARCH Open Access Deciphering the gene expression profile of peroxisome proliferator‑activated receptor signaling pathway in the left atria of patients with mitral regurgitation Mien‑Cheng Chen1*, Jen‑Ping Chang2, Yu‑Sheng Lin3, Kuo‑Li Pan3, Wan‑Chun Ho1, Wen‑Hao Liu1, Tzu‑Hao Chang4, Yao‑Kuang Huang5, Chih‑Yuan Fang1 and Chien‑Jen Chen1 Abstract Background: Differentially expressed genes in the left atria of mitral regurgitation (MR) pigs have been linked to peroxisome proliferator-activated receptor (PPAR) signaling pathway in the KEGG pathway. However, specific genes of the PPAR signaling pathway in the left atria of MR patients have never been explored. Methods: This study enrolled 15 MR patients with heart failure, 7 patients with aortic valve disease and heart failure, and 6 normal controls. We used PCR assay (84 genes) for PPAR pathway and quantitative RT-PCR to study specific genes of the PPAR pathway in the left atria. Results: Gene expression profiling analysis through PCR assay identified 23 genes to be differentially expressed in the left atria of MR patients compared to normal controls. The expressions of APOA1, ACADM, FABP3, ETFDH, ECH1, CPT1B, CPT2, SLC27A6, ACAA2, SMARCD3, SORBS1, EHHADH, SLC27A1, PPARGC1B, PPARA and CPT1A were significantly up-regulated, whereas the expression of PLTP was significantly down-regulated in the MR patients compared to normal controls. The expressions of HMGCS2, ACADM, FABP3, MLYCD, ECH1, ACAA2, EHHADH, CPT1A and PLTP were significantly up-regulated in the MR patients compared to patients with aortic valve disease. -

Argininosuccinate Lyase Deficiency
©American College of Medical Genetics and Genomics GENETEST REVIEW Argininosuccinate lyase deficiency Sandesh C.S. Nagamani, MD1, Ayelet Erez, MD, PhD1 and Brendan Lee, MD, PhD1,2 The urea cycle consists of six consecutive enzymatic reactions that citrulline together with elevated argininosuccinic acid in the plasma convert waste nitrogen into urea. Deficiencies of any of these enzymes or urine. Molecular genetic testing of ASL and assay of ASL enzyme of the cycle result in urea cycle disorders (UCDs), a group of inborn activity are helpful when the biochemical findings are equivocal. errors of hepatic metabolism that often result in life-threatening However, there is no correlation between the genotype or enzyme hyperammonemia. Argininosuccinate lyase (ASL) catalyzes the activity and clinical outcome. Treatment of acute metabolic decom- fourth reaction in this cycle, resulting in the breakdown of arginino- pensations with hyperammonemia involves discontinuing oral pro- succinic acid to arginine and fumarate. ASL deficiency (ASLD) is the tein intake, supplementing oral intake with intravenous lipids and/ second most common UCD, with a prevalence of ~1 in 70,000 live or glucose, and use of intravenous arginine and nitrogen-scavenging births. ASLD can manifest as either a severe neonatal-onset form therapy. Dietary restriction of protein and dietary supplementation with hyperammonemia within the first few days after birth or as a with arginine are the mainstays in long-term management. Ortho- late-onset form with episodic hyperammonemia and/or long-term topic liver transplantation (OLT) is best considered only in patients complications that include liver dysfunction, neurocognitive deficits, with recurrent hyperammonemia or metabolic decompensations and hypertension. -

What Disorders Are Screened for by the Newborn Screen?
What disorders are screened for by the newborn screen? Endocrine Disorders The endocrine system is important to regulate the hormones in our bodies. Hormones are special signals sent to various parts of the body. They control many things such as growth and development. The goal of newborn screening is to identify these babies early so that treatment can be started to keep them healthy. To learn more about these specific disorders please click on the name of the disorder below: English: Congenital Adrenal Hyperplasia Esapnol Hiperplasia Suprarrenal Congenital - - http://www.newbornscreening.info/Parents/otherdisorders/CAH.html - http://www.newbornscreening.info/spanish/parent/Other_disorder/CAH.html - Congenital Hypothyroidism (Hipotiroidismo Congénito) - http://www.newbornscreening.info/Parents/otherdisorders/CH.html - http://www.newbornscreening.info/spanish/parent/Other_disorder/CH.html Hematologic Conditions Hemoglobin is a special part of our red blood cells. It is important for carrying oxygen to the parts of the body where it is needed. When people have problems with their hemoglobin they can have intense pain, and they often get sick more than other children. Over time, the lack of oxygen to the body can cause damage to the organs. The goal of newborn screening is to identify babies with these conditions so that they can get early treatment to help keep them healthy. To learn more about these specific disorders click here (XXX). - Sickle Cell Anemia (Anemia de Célula Falciforme) - http://www.newbornscreening.info/Parents/otherdisorders/SCD.html - http://www.newbornscreening.info/spanish/parent/Other_disorder/SCD.html - SC Disease (See Previous Link) - Sickle Beta Thalassemia (See Previous Link) Enzyme Deficiencies Enzymes are special proteins in our body that allow for chemical reactions to take place. -

Overview of Newborn Screening for Organic Acidemias – for Parents
Overview of Newborn Screening for Organic Acidemias – For Parents What is newborn screening? What organic acidemias are on Indiana’s newborn screen? Before babies go home from the nursery, they have a Indiana’s newborn screen tests for several organic small amount of blood taken from their heel to test for acidemias. Some of the organic acidemias on a group of conditions, including organic acidemias. Indi ana’s newborn screen are: Babies who screen positive for an organic acidemia 3-Methylcrotonyl-CoA carboxylase need follow-up tests done to confirm they have the deficiency (also called 3-MCC deficiency) condition. Not all babies with a positive newborn Glutaric acidemia, type I screen will have an organic acidemia. Isovaleric acidemia Methylmalonic acidemia What are organic acidemias? Multiple-CoA carboxylase deficiency Propionic acidemia Organic acidemias are conditions that occur when a person’s body is not able to use protein to make What are the symptoms of organic acidemias? energy. Normally, when we eat, our bodies digest (or break down) food into certain proteins. Those Every child with an organic acidemia is different. proteins are used by our bodies to make energy. Most babies with organic acidemias will look normal Enzymes (special proteins that help our bodies at birth. Symptoms of organic acidemias can appear perform chemical reactions) usually help our bodies shortly after birth, or they may show up later in break down food and create energy. infancy or childhood. Common symptoms of organic A person with an organic acidemia is missing at least acidemias include weakness, vomiting, low blood one enzyme, or his/her enzymes do not work sugar, hypotonia (weak muscles), spasticity (muscle correctly. -

Chain Acyl-Coa Dehydrogenase (Mcad) Deficiency
EXPLORING THERAPEUTIC APPROACHES FOR TREATMENT OF MEDIUM- CHAIN ACYL-COA DEHYDROGENASE (MCAD) DEFICIENCY by Heejung Kang BS, Sungkyunkwan University, South Korea, 2003 MS, Sungkyunkwan University, South Korea, 2005 MS, University of Minnesota, 2008 Submitted to the Graduate Faculty of Graduate School of Public Health in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2014 UNIVERSITY OF PITTSBURGH GRADUATE SCHOOL OF PUBLIC HEALTH This dissertation was presented by Heejung Kang It was defended on April 15, 2014 and approved by Dissertation Advisor: Jerry Vockley, M.D. Ph.D., Professor, Pediatrics, School of Medicine, University of Pittsburgh Committee Chair: Robert Ferrell, Ph.D., Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh David Finegold, Ph.D., Professor, Pediatrics, School of Medicine, University of Pittsburgh Al-Walid A. Mohsen, Ph.D., Research Associate Professor of Pediatrics School of Medicine, University of Pittsburgh Zsolt Urban, Ph.D., Associate Professor, Human Genetics, Graduate School of Public Health, University of Pittsburgh ii Copyright © by Heejung Kang 2014 iii Jerry Vockley, MD, PhD EXPLORING THERAPEUTIC APPROACHES FOR TREATMENT OF MEDIUM- CHAIN ACYL-COA DEHYDROGENASE (MCAD) DEFICIENCY Heejung Kang, PhD University of Pittsburgh, 2014 ABSTRACT Medium chain acyl-CoA dehydrogenase deficiency (MCADD) is a common biochemical genetic disorder in the US. Nearly 90% of alleles from MCADD patients contain a common mutation in the ACADM (c.985A>G). The change replaces a lysine with a glutamate (K304E), causing improper folding. The K304E protein can fold to a mature form and is then stable and active when expressed in a prokaryotic system with molecular chaperonins. -

Thiazolidinediones Upregulate Fatty Acid Uptake and Oxidation in Adipose Tissue of Diabetic Patients Guenther Boden,1,2 Carol Homko,2 Maria Mozzoli,1,2 Louise C
Thiazolidinediones Upregulate Fatty Acid Uptake and Oxidation in Adipose Tissue of Diabetic Patients Guenther Boden,1,2 Carol Homko,2 Maria Mozzoli,1,2 Louise C. Showe,3 Calen Nichols,3 and Peter Cheung1,2 Thiazolidinediones (TZDs) are a new class of insulin- TZDs produce insulin sensitization, which takes place sensitizing drugs. To explore how and in which tissues primarily in skeletal muscle (6). Lowering plasma free they improve insulin action, we obtained fat and muscle fatty acid (FFA) levels improves insulin sensitivity (7). The biopsies from eight patients with type 2 diabetes before well-established TZD lowering of plasma FFAs has there- -fore been widely considered to be a major factor respon (5 ؍ and 2 months after treatment with rosiglitazone (n ,TZD treatment was associated sible for their insulin sensitizing effect (8–12). It is .(3 ؍ or troglitazone (n with a coordinated upregulation in the expression of however, not clear how TZDs lower FFA levels. Since they genes and synthesis of proteins involved in fatty acid  seem to have little or no effect on basal rates of lipolysis uptake, binding, -oxidation and electron transport, (11,13,14), the decrease in plasma FFA levels is probably and oxidative phosphorylation in subcutaneous fat but not in skeletal muscle. These changes were accompa- due to an increase in FFA clearance (oxidation and/or nied by a 13% increase in total body fat oxidation, a 20% esterification). Supporting this notion, we have recently decrease in plasma free fatty acid levels, and a 46% found that TZD-induced lowering of plasma FFAs was increase in insulin-stimulated glucose uptake. -

Activation of Pparα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis
Tohoku J. Exp. Med., 2016, 240, 113-122PPARα Activation in Cells due to VLCAD Deficiency 113 Activation of PPARα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis * * Yang Yang,1, Yuyao Feng,1, Xiaowei Zhang,2 Takero Nakajima,1 Naoki Tanaka,1 Eiko Sugiyama,3 Yuji Kamijo4 and Toshifumi Aoyama1 1Department of Metabolic Regulation, Shinshu University Graduate School of Medicine, Matsumoto, Nagano, Japan 2Department of Neurosurgery, The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, China 3Department of Nutritional Science, Nagano Prefectural College, Nagano, Nagano, Japan 4Department of Nephrology, Shinshu University School of Medicine, Matsumoto, Nagano, Japan Very-long-chain acyl-CoA dehydrogenase (VLCAD) catalyzes the first reaction in the mitochondrial fatty acid β-oxidation pathway. VLCAD deficiency is associated with the accumulation of fat in multiple organs and tissues, which results in specific clinical features including cardiomyopathy, cardiomegaly, muscle weakness, and hepatic dysfunction in infants. We speculated that the abnormal fatty acid metabolism in VLCAD-deficient individuals might cause cell necrosis by fatty acid toxicity. The accumulation of fatty acids may activate peroxisome proliferator-activated receptor (PPAR), a master regulator of fatty acid metabolism and a potent nuclear receptor for free fatty acids. We examined six skin fibroblast lines, derived from VLCAD-deficient patients and identified fatty acid accumulation and PPARα activation in these cell lines. We then found that the expression levels of three enzymes involved in fatty acid degradation, including long-chain acyl-CoA synthetase (LACS), were increased in a PPARα-dependent manner. This increased expression of LACS might enhance the fatty acyl-CoA supply to fatty acid degradation and sulfatide synthesis pathways. -

Pancytopenia: a Rare Presentation of Late Onset Isovaleric Acidemia
Karami H et al. IJBC 2020; 12(1): 38-40 Iranian Journal of Blood & Cancer Journal Home Page: www.ijbc.ir Letter to Editor Pancytopenia: A Rare Presentation of Late Onset Isovaleric Acidemia Hossein Karami1, Daniel Zamanfar2, Mohammad Reza Navaifar3, Parastoo Jamallivani4, Kimia Rasoli4, Mohammad Naderisorki1* 1Thalassemia Research Center, Department of Pediatrics Hematology and Oncology, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran 2Diabetes Research Center, Department of Pediatrics, Bou Ali Sina Hospital, Mazandaran University of Medical Sciences, Sari, Iran 3Pediatric Infectious Diseases Research Center, Mazandaran University of Medical Sciences, Sari, Iran 4Student Research Committe, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran ARTICLE INFO *Corresponding author: Mohammad Naderisorki, Article History: Bou Ali Sina Hospital, Mazandaran Received: 27.11.2019 University of Medical Sciences, Pasdaran Boulevard, P.O. Box: 48158- Accepted: 28.12.2019 38477, Sari, Iran Tel/Fax: +98 11 33342331 Email: [email protected] Please cite this article as: Karami H, Zamanfar D, Navaifar MR, Jamallivani P, Rasoli K, Naderisorki M. Pancytopenia: A Rare Presentation of Late Onset Isovaleric Acidemia. IJBC 2020; 12(1): 38-40. Dear Editor, thrombocytopenia and compensated metabolic acidosis. Isovaleric academia was first recognized by Tanaka Biochemical analysis including blood glucose and and colleagues as a new genetic disorder of leucine coagulation profile were within normal limits. Serum metabolism in two siblings in early infancy. There is C-reactive protein, erythrocyte sedimentation rate and Downloaded from ijbc.ir at 19:37 +0330 on Thursday September 30th 2021 a defect in the catabolism of leucine resulting in the lactate dehydrogenase were normal.