Download ( 947KB )
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Downloaded from GEO
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Oxylipin metabolism is controlled by mitochondrial b-oxidation during bacterial inflammation. Mariya Misheva1, Konstantinos Kotzamanis1*, Luke C Davies1*, Victoria J Tyrrell1, Patricia R S Rodrigues1, Gloria A Benavides2, Christine Hinz1, Robert C Murphy3, Paul Kennedy4, Philip R Taylor1,5, Marcela Rosas1, Simon A Jones1, Sumukh Deshpande1, Robert Andrews1, Magdalena A Czubala1, Mark Gurney1, Maceler Aldrovandi1, Sven W Meckelmann1, Peter Ghazal1, Victor Darley-Usmar2, Daniel White1, and Valerie B O’Donnell1 1Systems Immunity Research Institute and Division of Infection and Immunity, and School of Medicine, Cardiff University, UK, 2Department of Pathology, University of Alabama at Birmingham, Birmingham, AL 35294, USA, 3Department of Pharmacology, University of Colorado Denver, Aurora, CO 80045, USA, 4Cayman Chemical 1180 E Ellsworth Rd, Ann Arbor, MI 48108, United States, 5UK Dementia Research Institute at Cardiff, Cardiff University, UK Address correspondence: Valerie O’Donnell, [email protected] or Daniel White, [email protected], Systems Immunity Research Institute, Cardiff University *Both authors contributed equally to the study 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -
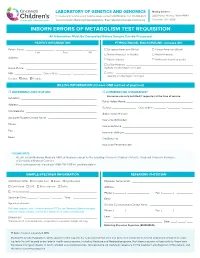
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

Activation of Pparα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis
Tohoku J. Exp. Med., 2016, 240, 113-122PPARα Activation in Cells due to VLCAD Deficiency 113 Activation of PPARα by Fatty Acid Accumulation Enhances Fatty Acid Degradation and Sulfatide Synthesis * * Yang Yang,1, Yuyao Feng,1, Xiaowei Zhang,2 Takero Nakajima,1 Naoki Tanaka,1 Eiko Sugiyama,3 Yuji Kamijo4 and Toshifumi Aoyama1 1Department of Metabolic Regulation, Shinshu University Graduate School of Medicine, Matsumoto, Nagano, Japan 2Department of Neurosurgery, The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, China 3Department of Nutritional Science, Nagano Prefectural College, Nagano, Nagano, Japan 4Department of Nephrology, Shinshu University School of Medicine, Matsumoto, Nagano, Japan Very-long-chain acyl-CoA dehydrogenase (VLCAD) catalyzes the first reaction in the mitochondrial fatty acid β-oxidation pathway. VLCAD deficiency is associated with the accumulation of fat in multiple organs and tissues, which results in specific clinical features including cardiomyopathy, cardiomegaly, muscle weakness, and hepatic dysfunction in infants. We speculated that the abnormal fatty acid metabolism in VLCAD-deficient individuals might cause cell necrosis by fatty acid toxicity. The accumulation of fatty acids may activate peroxisome proliferator-activated receptor (PPAR), a master regulator of fatty acid metabolism and a potent nuclear receptor for free fatty acids. We examined six skin fibroblast lines, derived from VLCAD-deficient patients and identified fatty acid accumulation and PPARα activation in these cell lines. We then found that the expression levels of three enzymes involved in fatty acid degradation, including long-chain acyl-CoA synthetase (LACS), were increased in a PPARα-dependent manner. This increased expression of LACS might enhance the fatty acyl-CoA supply to fatty acid degradation and sulfatide synthesis pathways. -

Suppression of Fatty Acid Oxidation by Thioesterase Superfamily Member
bioRxiv preprint doi: https://doi.org/10.1101/2021.04.21.440732; this version posted April 21, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Suppression of Fatty Acid Oxidation by Thioesterase Superfamily Member 2 in Skeletal Muscle Promotes Hepatic Steatosis and Insulin Resistance Norihiro Imai1, Hayley T. Nicholls1, Michele Alves-Bezerra1, Yingxia Li1, Anna A. Ivanova2, Eric A. Ortlund2, and David E. Cohen1 1Division of Gastroenterology and Hepatology, Joan & Sanford I. Weill Department of Medicine, Weill Cornell Medical College, NY 10021 USA 2Department of Biochemistry, Emory University, Atlanta, GA 30322 USA Current addresses: Norihiro Imai - Department of Gastroenterology and Hepatology, Nagoya University School of Medicine, Aichi 4668560 Japan Michele Alves-Bezerra - Department of Molecular Physiology and Biophysics, Baylor College of Medicine, Houston, TX 77030 USA bioRxiv preprint doi: https://doi.org/10.1101/2021.04.21.440732; this version posted April 21, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Figure number: 8 Supplemental figure number: 10 Supplemental table number: 2 References: 48 Keywords: Hepatic steatosis, obesity, acyl-CoA thioesterase, fatty acid oxidation, insulin resistance Conflict of interest: The authors have declared that no conflict of interest exists. Author contributions: N.I.: designed research studies, conducted experiments, acquired data, analyzed data and wrote manuscript. H.T.N.: conducted experiments and analyzed data, M.A.B.: designed research studies and conducted experiments, Y.L.: acquired data, A.A.I.: conducted experiments and analyzed data, E.A.O.: analyzed data, D.E.C.: designed research studies, analyzed data and wrote manuscript. -

Free PDF Download
European Review for Medical and Pharmacological Sciences 2019; 23: 1710-1721 Next-generation sequencing identifies a homozygous mutation in ACADVL associated with pediatric familial dilated cardiomyopathy S.J. CARLUS1, I.S. ALMUZAINI2, M. KARTHIKEYAN3, L. LOGANATHAN3, G.S. AL-HARBI1, A.M. ABDALLAH4, K.M. AL-HARBI1 1Pediatrics Department, Cardiogenetics Unit, College of Medicine, Taibah University, Al-Madinah, Kingdom of Saudi Arabia 2Department of Pediatric Cardiology, Al-Madinah Maternity and Children Hospital (MMCH), Al-Madinah, Kingdom of Saudi Arabia 3Department of Bioinformatics, Alagappa University, Karaikudi, Tamil Nadu, India 4West Midlands Regional Genetics Laboratory, Birmingham Women’s NHS Foundation Trust, Birmingham, United Kingdom Abstract. – OBJECTIVE: Pediatric familial di- Key Words lated cardiomyopathy (DCM) is a rare and se- Pediatric familial dilated cardiomyopathy, Targeted vere heart disease. The genetics of familial DCM gene sequencing, ACADVL, Saudi Arabia, Consanguinity, are complex and include over 100 known dis- Molecular docking, Molecular dynamics. ease-causing genes, but many causative genes are unknown. We aimed to identify the causative gene for DCM in a consanguineous Saudi Ara- bian family with affected family members and a history of sudden death. Introduction PATIENTS AND METHODS: Affected (two chil- dren) and unaffected (one sibling and the mother) Dilated cardiomyopathy (DCM) is a heart family members were screened by next-gener- ation sequencing (NGS) for 181 candidate DCM disease characterized by ventricular dilation and genes and underwent metabolic screening. Fif- impaired myocardial contractility. DCM affects ty-seven clinically annotated controls and 46 DCM 1 in 2500 of the general population and is one of cases were then tested for the identified mutation. -

Role of Metabolism in Bone Development and Homeostasis
International Journal of Molecular Sciences Review Role of Metabolism in Bone Development and Homeostasis Akiko Suzuki 1,2 , Mina Minamide 1,2, Chihiro Iwaya 1,2, Kenichi Ogata 1,2 and Junichi Iwata 1,2,3,* 1 Department of Diagnostic & Biomedical Sciences, School of Dentistry, The University of Texas Health Science Center at Houston, Houston, TX 77054, USA; [email protected] (A.S.); [email protected] (M.M.); [email protected] (C.I.); [email protected] (K.O.) 2 Center for Craniofacial Research, The University of Texas Health Science Center at Houston, Houston, TX 77054, USA 3 MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences, Houston, TX 77030, USA * Correspondence: [email protected] Received: 16 October 2020; Accepted: 25 November 2020; Published: 26 November 2020 Abstract: Carbohydrates, fats, and proteins are the underlying energy sources for animals and are catabolized through specific biochemical cascades involving numerous enzymes. The catabolites and metabolites in these metabolic pathways are crucial for many cellular functions; therefore, an imbalance and/or dysregulation of these pathways causes cellular dysfunction, resulting in various metabolic diseases. Bone, a highly mineralized organ that serves as a skeleton of the body, undergoes continuous active turnover, which is required for the maintenance of healthy bony components through the deposition and resorption of bone matrix and minerals. This highly coordinated event is regulated throughout life by bone cells such as osteoblasts, osteoclasts, and osteocytes, and requires synchronized activities from different metabolic pathways. Here, we aim to provide a comprehensive review of the cellular metabolism involved in bone development and homeostasis, as revealed by mouse genetic studies. -

Tissue Specific Roles of Fatty Acid Oxidation
TISSUE SPECIFIC ROLES OF FATTY ACID OXIDATION by Jieun Lee A dissertation submitted to Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland September, 2016 © 2016 Jieun Lee All Rights Reserved ABSTRACT The oxidation of long chain fatty acids facilitates mitochondrial respiration in diverse cell types. In this thesis, the role of fatty acid oxidation primarily in the adipose tissue and liver are discussed. To address this question, we generated mice with an adipose- or liver-specific knockout of carnitine palmitoyltransferase 2 (Cpt2), an obligate step in long chain mitochondrial fatty acid oxidation. In adipocyte-specific KO mice (Cpt2A-/-), the brown adipose tissue (BAT) of Cpt2A-/- mice was unable to utilize fatty acids and therefore caused hypothermia after an acute cold challenge. Surprisingly, Cpt2A-/- BAT was also unable to up-regulate thermogenic genes such as Ucp1 and Pgc1a in response to agonist-induced stimulation in vivo or ex vivo. The adipose specific loss of CPT2 did not result in changes in body weight on low or high fat diets, although paradoxically, low fat diets promoted and high fat diets suppressed adiposity. Additionally, a high fat diet increased oxidative stress and inflammation in gonadal white adipose tissue (WAT) of control mice but this effect was greatly suppressed in Cpt2A-/- mice. However, this suppression did not improve high fat diet induced glucose intolerance. In hepatocyte-specific KO (Cpt2L-/-) mice, fasting induced hepatic steatosis and serum dyslipidemia with an absence of circulating ketones while blood glucose remained normal. Systemic energy homeostasis was largely maintained in fasting Cpt2L-/- mice by adaptations in hepatic and systemic oxidative gene expression mediated in part by Pparα target genes including procatabolic hepatokines Fgf21, Gdf15 and Igfbp1. -

Construction and Validation of a Prognostic Gene-Based Model For
Article Construction and Validation of a Prognostic Gene-Based Model for Overall Survival Prediction in Hepatocellular Carcinoma Using an Integrated Statistical and Bioinformatic Approach Eskezeia Y. Dessie 1, Siang-Jyun Tu2, Hui-Shan Chiang2, Jeffrey J.P. Tsai1, Ya-Sian Chang2,*, Jan-Gowth Chang2,* and Ka-Lok Ng 1, 3, 4,* 1 Department of Bioinformatics and Medical Engineering, Asia University, Taichung, Taiwan; No. 500, Li- oufeng Rd., Wufeng, Taichung 41354, Taiwan; [email protected] (E.Y.D.); [email protected] (J.-P.T.); [email protected] (K.-L.N.) 2 Department of Laboratory Medicine, and Center for Precision Medicine, China Medical University and Hospital, Taichung, Taiwan; No. 2, Yude Rd., North Dist., Taichung City 404332, Taiwan; [email protected] (S.-J.T.); [email protected] (H.-S.C.); [email protected] (Y.-S.C.); [email protected] (J.-G.C.) 3 Department of Medical Research, China Medical University Hospital, China Medical University, Taichung, Taiwan; No. 2, Yude Rd., North Dist., Taichung City 404332, Taiwan; [email protected] (K.-L.N.) 4 Center for Artificial Intelligence and Precision Medicine Research, Asia University, Taichung, Taiwan; No. 500, Lioufeng Rd., Wufeng, Taichung 41354, Taiwan; [email protected] (K.-L.N.) * Correspondence: [email protected] (Y.-S.C.); [email protected] (K.-L.N.); [email protected] (J.-G.C.) Int. J. Mol. Sci. 2021, 22, 1632. https://doi.org/10.3390/ijms22041632 www.mdpi.com/journal/ijms Int. J. Mol. Sci. 2021, 22, 1632 2 of 7 Int. J. Mol. Sci. -

Ab118182 – Fatty Acid Oxidation Human In-Cell ELISA
ab118182 – Fatty Acid Oxidation Human In-Cell ELISA Kit (ACADVL, ACADM, HADHA) Instructions for Use For measuring in high throughput very long chain specific acyl-CoA dehydrogenase, medium-chain specific acyl-CoA dehydrogenase and long-chain 3-hydroxyl-CoA dehydrogenase This product is for research use only and is not intended for diagnostic use. 1 Table of Contents 1. Introduction 3 2. Assay Summary 6 3. Kit Contents 7 4. Storage and Handling 7 5. Additional Materials Required 8 6. Preparation of Reagents 8 7. Sample Preparation 9 8. Assay Procedure 11 9. Data Analysis 14 10. Assay Performance and Specificity 14 11. Frequently Asked Questions 18 12. Troubleshooting 21 2 1. Introduction Principle: ab118182 uses quantitative immunocytochemistry to measure protein levels or post-translational modifications in cultured cells. Cells are fixed in a microplate and targets of interest are detected with highly specific, well-characterized monoclonal antibodies, and levels are quantified with IRDye®-labeled Secondary Antibodies. IR imaging and quantitation is performed using a LI- COR® Odyssey® or Aerius® system. Background: The Fatty acid B-oxidation (FAO) pathway is a key metabolic pathway that plays an important role in energy homeostasis particularly in organs such as the liver, heart and skeletal muscle. Oxidation of fatty acids occurs inside the mitochondria where acyl-CoA esters (activated fatty acids) of various lengths are shortened into units of acetyl-CoA each time a cycle is fully completed. Each unit of acetyl-CoA is then oxidized by the mitochondria into CO 2 and H 2O via the citric acid cycle and the mitochondria respiratory chain. -

Very Long-Chain Acyl-Coa Dehydrogenase (VLCAD) Deficiency
Very long-chain acyl-CoA dehydrogenase (VLCAD) deficiency What is VLCAD deficiency? VLCAD deficiency is an inherited metabolic disease characterized by lethargy, weakness, and low blood sugar. Individuals with VLCAD deficiency have deficiencies of the very long-chain acyl-CoA dehydrogenase enzyme, which helps to break down very long-chain fatty acids (a type of fat) that are used for energy in cells.1 Symptoms associated with VLCAD deficiency are due to low levels of energy and the toxic build-up of fatty acids in cells, especially in the heart, liver, and muscles.2 What are the symptoms of VLCAD deficiency and what treatment is available? Symptoms of VLCAD deficiency are variable in severity and age at onset, but are typically seen in infancy or early childhood.1 Children with the most severe, early-onset form of VLCAD deficiency are at risk for serious complications such as liver problems and life-threatening heart problems.2 Children or adults with a later-onset form may have intermittent muscle-related or no symptoms.3 Signs and symptoms are often triggered by fasting, illness, or exercise and may include:2,3 • Episodic hypoglycemia (low blood sugar) • Irritability • Lethargy (lack of energy) • Muscle weakness • Cardiomyopathy (abnormal heart muscle) • Abnormal heart rhythms • Hepatomegaly (enlarged liver) • Intermittant rhabdomyolysis (breakdown of muscle tissue) Treatment focuses on prevention of complications and management of symptoms through dietary modifications and avoidance of dehydration and fasting. Acute episodes may be treated with intravenous glucose.2,3 VLCAD deficiency is included in all state newborn screening profiles in the United States.4 How is VLCAD deficiency inherited? VLCAD deficiency is an autosomal recessive disease caused by mutations in the ACADVL gene.1 An individual who inherits one copy of an ACADVL gene mutation is a carrier and is not expected to have related health problems. -

Identification of Very-Long-Chain Acyl-Coa Dehydrogenase Deficiency in Three Patients ~Reviousl~Diagnosed with Long-Chain Acyl-Coa Dehydrogenase Deficiency
003 I-3998/93/340 1-0 I1 1$03.00/0 PEDIATRIC RESEARCH Vol. 34, No. 1, 1993 Copyright O 1993 International Pediatric Research Foundation. Inc. Prinred in U.S.A. Identification of Very-Long-Chain Acyl-CoA Dehydrogenase Deficiency in Three Patients ~reviousl~Diagnosed with Long-chain Acyl-CoA Dehydrogenase Deficiency SEIJI YAMAGUCHI,' YASUHIRO INDO: PAUL M. COATES, TAKASHI HASHIMOTO, AND KAY TANAKA Department of Genetics. Yale University School ofMedicine, New IIaven, Connecticlrt 06510 [S. Y., Y.I., K.T.]; Division of Gastroenterology and Ntrtrition, Cl~ildren'sHospital of Philadelphia, Philadelphia. Pennsylvania 19104 [P.IZf.C.]; and Department of Biocl~emistry,Sl~inshu University School of Medicine, hfatslrmoto, Nagano 390. Japan [T.H.] ABSTRACT. Long-chain acyl-CoA dehydrogenase Hale ul. in 1985 (I), at least 13 patients have been reported (LCAD) deficiency is a disorder of fatty acid 8-oxidation. (2.3). The main clinical symptoms of this disease include muscle Its diagnosis has been made based on the reduced activity weakness. hepatomegaly. cardiomegaly, and episodes of hypo- of palmitoyl-CoA dehydrogenation, i.e., in fibroblasts. We ketotic hypoglycemia. Some of the patients died with an acute previously showed that in immunoblot analysis, an LCAD episode without noticeable prodromal symptoms, mimicking band of normal size and intensity was detected in fibro- sudden infant death syndrome (3). LCAD deficiency is one of a blasts from all LCAD-deficient patients tested. In the group of diseases caused by defects in fatty acid oxidation (4) present study, we amplified via polymerase chain reaction that includes, among others, MCAD deficiency (5) and long- and sequenced LCAD cDNA from three of these LCAD- chain 3-hydroxyacyl-CoA dehydrogenase deficiency (6). -
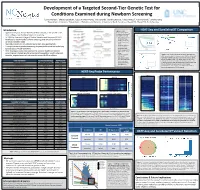
Development of a Targeted Second-Tier Genetic Test For
Development of a Targeted Second-Tier Genetic Test for Conditions Examined during Newborn Screening 1Lonna Mollison, 1Chelsea Gustafson, 1Edgar A Rivera-Munoz, 1Alicia Brandt, 1Daniela DeCristo, 1Falecia Metcalf, 2Cynthia Powell, 1Jonathan Berg 1Department of Genetics, 2Department of Pediatrics and Genetics, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina Introduction Figure 1. Library HEAT-Seq and SureSelectXT Comparison • Approximately four million children are born annually in the United States, preparation workflows for Agilent’s SureSelectXT most undergo state mandated newborn screening and Roche’s HEAT-Seq. A. B. C. • In 2006 the American College of Medical Genetics and Genomics (ACMG) • Time requirement for developed a recommended uniform screening panel (RUSP) to minimize SureSelectXT was about 32 hours, and variability between states for HEAT-Seq about 8 • Most RUSP conditions are detected by tandem mass spectrometry hours. • Recommended DNA • Through the use of genetic sequencing it is possible to detect the underlying input amount for genetic cause of RUSP conditions SureSelectXT was • Here we propose a step-wise approach to enhance traditional newborn about 3000ng, and for HEAT-Seq was about D. screening and integrate genetic screening into population health using cost- 250ng. effective, targeted sequencing to examine current RUSP conditions • Cost per sample for Figure 4. (A-C) The percent of bases at varying read depths for SureSelectXT HEAT-Seq and SureSelect when normalized to 5M reads (A), 50M (including all human reads (B) and 200M reads (C) for each of the 8 samples. (D) The exon baits) was about percent of targeted bases in all samples sequenced at 30 fold Core Condition Associated Gene(s) ACMG Code $333, and for HEAT- coverage were estimated normalizing the data to various values Maple Syrup Urine Disease BCKDHA, BCKDHB, DBT MSUD Seq (including MIPs) of sequenced reads.