Genetic Mapping and Mutation Analysis of Genes Causing Human Hereditary Skeletal Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MECHANISMS in ENDOCRINOLOGY: Novel Genetic Causes of Short Stature
J M Wit and others Genetics of short stature 174:4 R145–R173 Review MECHANISMS IN ENDOCRINOLOGY Novel genetic causes of short stature 1 1 2 2 Jan M Wit , Wilma Oostdijk , Monique Losekoot , Hermine A van Duyvenvoorde , Correspondence Claudia A L Ruivenkamp2 and Sarina G Kant2 should be addressed to J M Wit Departments of 1Paediatrics and 2Clinical Genetics, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, Email The Netherlands [email protected] Abstract The fast technological development, particularly single nucleotide polymorphism array, array-comparative genomic hybridization, and whole exome sequencing, has led to the discovery of many novel genetic causes of growth failure. In this review we discuss a selection of these, according to a diagnostic classification centred on the epiphyseal growth plate. We successively discuss disorders in hormone signalling, paracrine factors, matrix molecules, intracellular pathways, and fundamental cellular processes, followed by chromosomal aberrations including copy number variants (CNVs) and imprinting disorders associated with short stature. Many novel causes of GH deficiency (GHD) as part of combined pituitary hormone deficiency have been uncovered. The most frequent genetic causes of isolated GHD are GH1 and GHRHR defects, but several novel causes have recently been found, such as GHSR, RNPC3, and IFT172 mutations. Besides well-defined causes of GH insensitivity (GHR, STAT5B, IGFALS, IGF1 defects), disorders of NFkB signalling, STAT3 and IGF2 have recently been discovered. Heterozygous IGF1R defects are a relatively frequent cause of prenatal and postnatal growth retardation. TRHA mutations cause a syndromic form of short stature with elevated T3/T4 ratio. Disorders of signalling of various paracrine factors (FGFs, BMPs, WNTs, PTHrP/IHH, and CNP/NPR2) or genetic defects affecting cartilage extracellular matrix usually cause disproportionate short stature. -

Fetal Megacystis: a Lot More Than LUTO
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Erasmus University Digital Repository Ultrasound Obstet Gynecol 2019; 53: 779–787 Published online in Wiley Online Library (wileyonlinelibrary.com). DOI: 10.1002/uog.19182. This is an open access article under the terms of the Creative Commons Attribution-NonCommercial License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited and is not used for commercial purposes. Fetal megacystis: a lot more than LUTO F. FONTANELLA1 ,L.MAGGIO1,J.B.G.M.VERHEIJ2,L.K.DUIN1 , P. N. ADAMA VAN SCHELTEMA3, T. E. COHEN-OVERBEEK4,E.PAJKRT5, M. BEKKER6,7, C. WILLEKES8,C.J.BAX9, V. GRACCHI10, D. OEPKES3 andC.M.BILARDO1 1Department of Obstetrics, Gynaecology and Prenatal Diagnosis, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands; 2Department of Genetics, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands; 3Department of Obstetrics, Gynaecology and Prenatal Diagnosis, Leiden University Medical Center, Leiden, The Netherlands; 4Division of Obstetrics and Prenatal Medicine, Department of Obstetrics and Gynecology, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands; 5Department of Obstetrics, Academic Medical Center Amsterdam, Amsterdam, The Netherlands; 6Department of Obstetrics, Gynaecology and Prenatal Diagnosis, Radboud University Medical Center, Nijmegen, The Netherlands; 7Department of Obstetrics, Gynaecology -

Orphanet Report Series Rare Diseases Collection
Orphanet Report Series Rare Diseases collection January 2013 Disease Registries in Europe www.orpha.net 20102206 Table of contents Methodology 3 List of rare diseases that are covered by the listed registries 4 Summary 13 1- Distribution of registries by country 13 2- Distribution of registries by coverage 14 3- Distribution of registries by affiliation 14 Distribution of registries by country 15 European registries 38 International registries 41 Orphanet Report Series - Disease Registries in Europe - January 2013 2 http://www.orpha.net/orphacom/cahiers/docs/GB/Registries.pdf Methodology Patient registries and databases constitute key instruments to develop clinical research in the field of rare diseases (RD), to improve patient care and healthcare planning. They are the only way to pool data in order to achieve a sufficient sample size for epidemiological and/or clinical research. They are vital to assess the feasibility of clinical trials, to facilitate the planning of appropriate clinical trials and to support the enrolment of patients. Registries of patients treated with orphan drugs are particularly relevant as they allow the gathering of evidence on the effectiveness of the treatment and on its possible side effects, keeping in mind that marketing authorisation is usually granted at a time when evidence is still limited although already somewhat convincing. This report gather the information collected by Orphanet so far, regarding systematic collections of data for a specific disease or a group of diseases. Cancer registries are listed only if they belong to the network RARECARE or focus on a rare form of cancer. The report includes data about EU countries and surrounding countries participating to the Orphanet consortium. -

Blueprint Genetics Comprehensive Skeletal Dysplasias and Disorders
Comprehensive Skeletal Dysplasias and Disorders Panel Test code: MA3301 Is a 251 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of disorders involving the skeletal system. About Comprehensive Skeletal Dysplasias and Disorders This panel covers a broad spectrum of skeletal disorders including common and rare skeletal dysplasias (eg. achondroplasia, COL2A1 related dysplasias, diastrophic dysplasia, various types of spondylo-metaphyseal dysplasias), various ciliopathies with skeletal involvement (eg. short rib-polydactylies, asphyxiating thoracic dysplasia dysplasias and Ellis-van Creveld syndrome), various subtypes of osteogenesis imperfecta, campomelic dysplasia, slender bone dysplasias, dysplasias with multiple joint dislocations, chondrodysplasia punctata group of disorders, neonatal osteosclerotic dysplasias, osteopetrosis and related disorders, abnormal mineralization group of disorders (eg hypopohosphatasia), osteolysis group of disorders, disorders with disorganized development of skeletal components, overgrowth syndromes with skeletal involvement, craniosynostosis syndromes, dysostoses with predominant craniofacial involvement, dysostoses with predominant vertebral involvement, patellar dysostoses, brachydactylies, some disorders with limb hypoplasia-reduction defects, ectrodactyly with and without other manifestations, polydactyly-syndactyly-triphalangism group of disorders, and disorders with defects in joint formation and synostoses. Availability 4 weeks Gene Set Description -
With a Learning Disability; Guidance for General Practice
Improving identification of people with a learning disability: guidance for general practice NHS England and Improvement Publishing Approval Reference: 001030 Version 1 NHS England and NHS Improvement Contents Introduction .................................................................................... 2 Actions for practices ....................................................................... 4 Appendix 1: List of codes that indicate a learning disability ........... 7 Appendix 2: List of codes that may indicate a learning disability . 14 Appendix 3: List of outdated codes .............................................. 20 Appendix 4: Learning disability identification check-list ............... 22 1 | Contents Introduction 1. The NHS Long Term Plan1 commits to improve uptake of the existing annual health check in primary care for people aged over 14 years with a learning disability, so that at least 75% of those eligible have a learning disability health check each year. 2. There is also a need to increase the number of people receiving the annual seasonal flu vaccination, given the level of avoidable mortality associated with respiratory problems. 3. In 2017/18, only 44.6% of patients with a learning disability received a flu vaccination and only 55.1% of patients with a learning disability received an annual learning disability health check.2 4. In June 2019, NHS England and NHS Improvement announced a series of measures to improve coverage of annual health checks and flu vaccination for people with a learning disability. One of the commitments was to improve the quality of registers for people with a learning disability3. Clinical coding review 5. Most GP practices have developed a register of their patients known to have a learning disability. This has been developed from clinical diagnoses, from information gathered from learning disabilities teams and social services and has formed the basis of registers for people with learning disability developed for the Quality and Outcomes Framework (QOF). -

Craniosynostosis Precision Panel Overview Indications Clinical Utility
Craniosynostosis Precision Panel Overview Craniosynostosis is defined as the premature fusion of one or more cranial sutures, often resulting in abnormal head shape. It is a developmental craniofacial anomaly resulting from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). As well, craniosynostosis can be simple when only one suture fuses prematurely or complex/compound when there is a premature fusion of multiple sutures. Complex craniosynostosis are usually associated with other body deformities. The main morbidity risk is the elevated intracranial pressure and subsequent brain damage. When left untreated, craniosynostosis can cause serious complications such as developmental delay, facial abnormality, sensory, respiratory and neurological dysfunction, eye anomalies and psychosocial disturbances. In approximately 85% of the cases, this disease is isolated and nonsyndromic. Syndromic craniosynostosis usually present with multiorgan complications. The Igenomix Craniosynostosis Precision Panel can be used to make a directed and accurate diagnosis ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Craniosynostosis Precision Panel is indicated for those patients with a clinical diagnosis or suspicion with or without the following manifestations: ‐ Microcephaly ‐ Scaphocephaly (elongated head) ‐ Anterior plagiocephaly ‐ Brachycephaly ‐ Torticollis ‐ Frontal bossing Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. - Early initiation of treatment in the form surgical procedures to relieve fused sutures, midface advancement, limited phase of orthodontic treatment and combined 1 orthodontics/orthognathic surgery treatment. -

Chromosomal Microarray Analysis in Turkish Patients with Unexplained Developmental Delay and Intellectual Developmental Disorders
177 Arch Neuropsychitry 2020;57:177−191 RESEARCH ARTICLE https://doi.org/10.29399/npa.24890 Chromosomal Microarray Analysis in Turkish Patients with Unexplained Developmental Delay and Intellectual Developmental Disorders Hakan GÜRKAN1 , Emine İkbal ATLI1 , Engin ATLI1 , Leyla BOZATLI2 , Mengühan ARAZ ALTAY2 , Sinem YALÇINTEPE1 , Yasemin ÖZEN1 , Damla EKER1 , Çisem AKURUT1 , Selma DEMİR1 , Işık GÖRKER2 1Faculty of Medicine, Department of Medical Genetics, Edirne, Trakya University, Edirne, Turkey 2Faculty of Medicine, Department of Child and Adolescent Psychiatry, Trakya University, Edirne, Turkey ABSTRACT Introduction: Aneuploids, copy number variations (CNVs), and single in 39 (39/123=31.7%) patients. Twelve CNV variant of unknown nucleotide variants in specific genes are the main genetic causes of significance (VUS) (9.75%) patients and 7 CNV benign (5.69%) patients developmental delay (DD) and intellectual disability disorder (IDD). were reported. In 6 patients, one or more pathogenic CNVs were These genetic changes can be detected using chromosome analysis, determined. Therefore, the diagnostic efficiency of CMA was found to chromosomal microarray (CMA), and next-generation DNA sequencing be 31.7% (39/123). techniques. Therefore; In this study, we aimed to investigate the Conclusion: Today, genetic analysis is still not part of the routine in the importance of CMA in determining the genomic etiology of unexplained evaluation of IDD patients who present to psychiatry clinics. A genetic DD and IDD in 123 patients. diagnosis from CMA can eliminate genetic question marks and thus Method: For 123 patients, chromosome analysis, DNA fragment analysis alter the clinical management of patients. Approximately one-third and microarray were performed. Conventional G-band karyotype of the positive CMA findings are clinically intervenable. -

Primordial Dwarfism: a Case Series from North East of Iran and Literature Review
April 2019, Volume 7, Issue 2, Number 14 A Case Report and Literature Review: Primordial Dwarfism: A Case Series From North East of Iran and Literature Review Rahim Vakili1, 2 , Somayyeh Hashemian1* 1. Department of Pediatrics, Faculty of Medicine, Imam Reza Hospital, Mashhad University of Medical Sciences, Mashhad, Iran. 2. Medical Genetic Research Center, Mashhad University of Medical Sciences, Mashhad, Iran. Use your device to scan and read the article online Citation: Vakili R, Hashemian S. Primordial Dwarfism: A Case Series From North East of Iran and Literature Review. Journal of Pediatrics Review. 2019; 7(2):113-120. http://dx.doi.org/10.32598/jpr.7.2.113 : http://dx.doi.org/10.32598/jpr.7.2.113 A B S T R A C T Introduction: Primordial dwarfism is a rare class of genetic disorders, characterized by intrauterine See Page 119 Funding: growth retardation, short stature at birth and growth deficiency that persist throughout life. This disorder is caused by various mechanisms such as chromosomal abnormalities, molecular Article info: changes and mutation of genes that result in developmental defects, facial dysmorphism and Received: 15 February 2018 skeletal abnormalities in fetus. Primordial dwarfism includes 5 specific subtypes that their First Revision: 10 March 2018 descriptions vary from one type to another. This study aimed to report 7 cases of primordial Accepted: 30 May 2018 dwarfism as the first case series study and literature review of this disorder in Iran. Published: 01 April 2019 Case Presentations: This study presented primordial dwarfism patients and summarized clinical findings of 7 cases who referred to Pediatric endocrine wards in Imam Reza Hospital, from June 2016 to September 2017. -
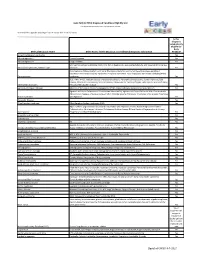
Early ACCESS Diagnosed Conditions List
Iowa Early ACCESS Diagnosed Conditions Eligibility List List adapted with permission from Early Intervention Colorado To search for a specific word type "Ctrl F" to use the "Find" function. Is this diagnosis automatically eligible for Early Medical Diagnosis Name Other Names for the Diagnosis and Additional Diagnosis Information ACCESS? 6q terminal deletion syndrome Yes Achondrogenesis I Parenti-Fraccaro Yes Achondrogenesis II Langer-Saldino Yes Schinzel Acrocallosal syndrome; ACLS; ACS; Hallux duplication, postaxial polydactyly, and absence of the corpus Acrocallosal syndrome, Schinzel Type callosum Yes Acrodysplasia; Arkless-Graham syndrome; Maroteaux-Malamut syndrome; Nasal hypoplasia-peripheral dysostosis-intellectual disability syndrome; Peripheral dysostosis-nasal hypoplasia-intellectual disability (PNM) Acrodysostosis syndrome Yes ALD; AMN; X-ALD; Addison disease and cerebral sclerosis; Adrenomyeloneuropathy; Siemerling-creutzfeldt disease; Bronze schilder disease; Schilder disease; Melanodermic Leukodystrophy; sudanophilic leukodystrophy; Adrenoleukodystrophy Pelizaeus-Merzbacher disease Yes Agenesis of Corpus Callosum Absence of the corpus callosum; Hypogenesis of the corpus callosum; Dysplastic corpus callosum Yes Agenesis of Corpus Callosum and Chorioretinal Abnormality; Agenesis of Corpus Callosum With Chorioretinitis Abnormality; Agenesis of Corpus Callosum With Infantile Spasms And Ocular Anomalies; Chorioretinal Anomalies Aicardi syndrome with Agenesis Yes Alexander Disease Yes Allan Herndon syndrome Allan-Herndon-Dudley -

Statistical Analysis Plan
Cover Page for Statistical Analysis Plan Sponsor name: Novo Nordisk A/S NCT number NCT03061214 Sponsor trial ID: NN9535-4114 Official title of study: SUSTAINTM CHINA - Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Document date: 22 August 2019 Semaglutide s.c (Ozempic®) Date: 22 August 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL Clinical Trial Report Status: Final Appendix 16.1.9 16.1.9 Documentation of statistical methods List of contents Statistical analysis plan...................................................................................................................... /LQN Statistical documentation................................................................................................................... /LQN Redacted VWDWLVWLFDODQDO\VLVSODQ Includes redaction of personal identifiable information only. Statistical Analysis Plan Date: 28 May 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL UTN:U1111-1149-0432 Status: Final EudraCT No.:NA Page: 1 of 30 Statistical Analysis Plan Trial ID: NN9535-4114 Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Author Biostatistics Semaglutide s.c. This confidential document is the property of Novo Nordisk. No unpublished information contained herein may be disclosed without prior written approval from Novo Nordisk. Access to this document must be restricted to relevant parties.This -

A Unifying Hypothesis on the Pathogenesis of Moyamoya Disease Based on a Systematic Review
NEUROSURGICAL FOCUS Neurosurg Focus 51 (3):E6, 2021 The mechanobiological theory: a unifying hypothesis on the pathogenesis of moyamoya disease based on a systematic review Bhanu Jayanand Sudhir, MCh,1 Arun Gowda Keelara, MS,1 Easwer Harihara Venkat, MCh,1 Ken Kazumata, MD, PhD,2 and Ananthalakshmy Sundararaman, PhD3 1Department of Neurosurgery, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, Kerala State, India; 2Department of Neurosurgery, Hokkaido University Graduate School of Medicine, Sapporo, Japan; and 3Department of Cardiovascular Diseases and Diabetes Biology, Rajiv Gandhi Centre for Biotechnology, Trivandrum, Kerala State, India OBJECTIVE Moyamoya angiopathy (MMA) affects the distal internal carotid artery and is designated as moyamoya disease (MMD) when predisposing conditions are absent, or moyamoya syndrome (MMS) when it occurs secondary to other causes. The authors aimed to investigate the reason for this anatomical site predilection of MMA. There is compel- ling evidence to suggest that MMA is a phenomenon that occurs due to stereotyped mechanobiological processes. Literature regarding MMD and MMS was systematically reviewed to decipher a common pattern relating to the develop- ment of MMA. METHODS A systematic review was conducted to understand the pathogenesis of MMA in accordance with PRISMA guidelines. PubMed MEDLINE and Scopus were searched using “moyamoya” and “pathogenesis” as common keywords and specific keywords related to six identified key factors. Additionally, a literature search was performed for MMS using “moyamoya” and “pathogenesis” combined with reported associations. A progressive search of the literature was also performed using the keywords “matrix metalloprotease,” “tissue inhibitor of matrix metalloprotease,” “endothelial cell,” “smooth muscle cell,” “cytokines,” “endothelin,” and “transforming growth factor” to infer the missing links in molecular pathogenesis of MMA. -

Omphalocele and Gastroschisis Precision Panel Overview Indications Clinical Utility
Omphalocele and Gastroschisis Precision Panel Overview Omphalocele, also known as exomphalos, is a midline abdominal wall defect at the base of the umbilical cord where herniation of abdominal contents takes place. The herniated organs are covered by the parietal peritoneum. The cause of omphalocele postulated to be a failure of the bowel to return into the abdomen by 10-12 weeks. Omphaloceles are associated with other anomalies in more than 70% of the cases, generally chromosomal, and the severity is dictated by the anomalies that are present. The main difficulty of this condition is the exclusion of associated conditions, not all diagnosed prenatally. Gastroschisis represents a herniation of abdominal contents through a paramedian full-thickness abdominal fusion defect. The abdominal herniation, in contrast with omphalocele, is usually to the right of the umbilical cord. It usually contains small bowel and has no surrounding membrane. Challenges in management of gastroschisis are related to the prevention of late intrauterine death, and the prediction and treatment of complex forms. The Igenomix Omphalocele and Gastroschisis Gene Panel can be used to as a screening tool for underlying genetic alterations associated to these conditions. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Omphalocele and Gastroschisis Gene Panel is indicated for those patients with a clinical suspicion of omphalocele and/or gastroschisis which manifest as: - Herniation of intestines through abdominal wall - Polyhydramnios in utero - Elevated levels of maternal serum a-fetoprotein (MSAFP) Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient.