Review Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

Molecular Detection of Human Parasitic Pathogens
MOLECULAR DETECTION OF HUMAN PARASITIC PATHOGENS MOLECULAR DETECTION OF HUMAN PARASITIC PATHOGENS EDITED BY DONGYOU LIU Boca Raton London New York CRC Press is an imprint of the Taylor & Francis Group, an informa business CRC Press Taylor & Francis Group 6000 Broken Sound Parkway NW, Suite 300 Boca Raton, FL 33487-2742 © 2013 by Taylor & Francis Group, LLC CRC Press is an imprint of Taylor & Francis Group, an Informa business No claim to original U.S. Government works Version Date: 20120608 International Standard Book Number-13: 978-1-4398-1243-3 (eBook - PDF) This book contains information obtained from authentic and highly regarded sources. Reasonable efforts have been made to publish reliable data and information, but the author and publisher cannot assume responsibility for the validity of all materials or the consequences of their use. The authors and publishers have attempted to trace the copyright holders of all material reproduced in this publication and apologize to copyright holders if permission to publish in this form has not been obtained. If any copyright material has not been acknowledged please write and let us know so we may rectify in any future reprint. Except as permitted under U.S. Copyright Law, no part of this book may be reprinted, reproduced, transmitted, or utilized in any form by any electronic, mechanical, or other means, now known or hereafter invented, including photocopying, microfilming, and recording, or in any information storage or retrieval system, without written permission from the publishers. For permission to photocopy or use material electronically from this work, please access www.copyright.com (http://www.copyright.com/) or contact the Copyright Clearance Center, Inc. -
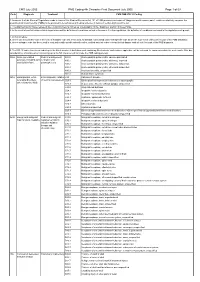
CMS PMB ICD-10 Coding
CMS July 2005 PMB Coding 4th Character Final Dcoument July 2005 Page 1 of 69 Code Diagnosis Treatment CMS PMB ICD-10 Coding 1. Annexure A of the General Regulations made in terms of the Medical Schemes Act, 131 of 1998 provides a schedule of “diagnosis and treatment pairs”, which cumulatively comprise the prescribed minimum benefits (PMBs) to be provided to beneficiaries of medical schemes in terms of section 29(1)(o) of the Act. 2. The attached ICD10 codes represent the Council for Medical Schemes’ interpretation of the “diagnosis” portion of these PMBs. 3. In the event of conflict between this interpretation and the definition of conditions set out in Annexure A to the regulations, the definition of conditions contained in the regulations will prevail. 4. In this schedule: a. where only the primary code in the form of a dagger code has been used, all asterisk codes listed under that specific code as per the ICD-10 set of books form part of the PMB diagnosis; b. where a dagger code has been used in conjunction with specific asterisk codes, omitted asterisk codes relevant to that dagger code do not form part of the PMB diagnosis. 5. The ICD-10 codes have been coded up to the 4th character. A draft document containing 5th character codes where applicable, will be released for comments within the next month. After due consideration, a final document containing up to the 5th character will conclude the PMB coding process. 906A Acute generalised Medical management; A80.0 Acute paralytic poliomyelitis, vaccine-associated paralysis, including -

2011/109440 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date _ . 9 September 2011 (09.09.2011) 2011/109440 Al (51) International Patent Classification: [CH/CH]; Chemin Des Chevreuils 1, 1188 Gimel (CH). C12Q 1/68 (2006.01) G01N 33/53 (2006.01) HOLTERMAN, Daniel [US/US]; 14465 North 14th St., Phoenix, AZ 85022 (US). (21) International Application Number: PCT/US201 1/026750 (74) Agent: AKHAVAN, Ramin; Caris Life Sciences, Inc., 6655 N. MacArthur Blvd., Irving, TX 75039 (US). (22) International Filing Date: 1 March 201 1 (01 .03.201 1) (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, English (25) Filing Language: AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (26) Publication Language: English CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (30) Priority Data: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 61/274,124 1 March 2010 (01 .03.2010) US KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 61/357,5 17 22 June 2010 (22.06.2010) US ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 61/364,785 15 July 2010 (15.07.2010) us NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (71) Applicant (for all designated States except US): CARIS SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, LIFE SCIENCES LUXEMBOURG HOLDINGS [LU/ TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

CNS Infections: LP Is an Important Test in the Diagnosis of Meningitis and Encephalitis
Bacterial meningitis: bacterial infection of the Leptomeninges. • The most common cause of bacterial meningitis in neonates is B group streptococcus and Gram negative bacteria (E.coli and Citrobacter)-ampicillin and gentamycin or third generation cephalosporines. Citrobacter is associated with high incidence of multiple brain abscesses. The most common cause of bacterial meningitis in age group 3 months-5 years are H.influenzae and streptococcus pneumoniae-penecillinnes and third generation cephalosporines. The most common cause in older children and adults are strept. Pneumoniae and Neisseria meningitides-penecillinnes and cephalosporines. The most common cause of viral meningitis is enteroviruses (echo and Cocksakie viruses). • The clinical picture depends on the age: neonates and children present with sepsis. Adults and old children (fever, headaches, vomiting, neck stiffness and decreased level of consciousness. Hemorrhagic rash in case of Neisseria meningitides). Patients should be started on high dose Abs and in the absence of increased ICP , LP should be performed (high protein, decreased glucose, pleocytosis. Neutrophils in thousands. In the presence of raised ICP start Abs and get CT head. Duration of treatment 10-14 days iv Abs. • Individuals exposed to N.meningidites infection should be given Rifampicin for 3-5 days. Vaccines are available. • Talk about TB meningitis (basal meningitis with multiple cranial nerve palsies and sometimes hydrocephalus) and • Discuss the indications and contraindications of LP in CNS infections: LP is an important test in the diagnosis of meningitis and encephalitis. It is contraindicated in the presence signs of increased ICP due to space occupying lesion such as abscess, subdural and epidural empyema (papilloedema, decreased level of consciousness). -

Management of Brain Abscesses
ORIGINAL ARTICLE Management of Brain Abscesses Riaz ur Rehman, Azmatullah khattak, Mian Iftihar Ul Huq, Mewat Shah, Mushtaq ABSTRACT Objective To find the etiology and outcome of treatment of brain abscesses. Study design Descriptive case series. Place & Department of Neurosurgery, Hayatabad Medical complex Peshawar, from October 2008 Duration of to January 2010. study Methodology This study was carried out on patients of brain abscesses of all ages and both genders. Patients having fungal brain abscess, amoebic brain abscess and tuberculous brain abscess were excluded. Brain abscess was diagnosed on contrast CT scan. Cases of early cerebritis were treated using parenteral antibiotics for six to eight weeks. Surgical treatment consisted of either burr hole aspiration with the help of brain cannula, re-aspiration or craniotomy and excision of abscess capsule. Therapeutic outcome was assessed with CT scan on follow up. Procedure related complications and mortality were also recorded. Results A total of 73 patients were managed. The commonest age group was from 11-20 year. The mean age was 26.36 ± 14.1 year (range - 0.16 - 67 year). There were 46 (63.01%) male and 27 (36.99%) female patients. The majority of brain abscesses were supratentorial (n=65 - 89.04%). In 8 (11.96%) cases abscess was in infratentorial region. Contiguous focus of infection was responsible for brain abscess in 29 (39.72%) patients, Majority of patients presented with headache (n=30 - 41.09%) and vomiting (n=25 - 34.24%). Surgical drainage was performed in 70 (95.89%) patients where as 3 (4.11%) patients were treated conservatively. Initially only burr hole aspiration was done in all surgically treated patients. -

Medical Parasitology
Medical Parasitology The main aim of medical Parasitology course is to provide the student with knowledge, comprehension and methods of application of medical Parasitology in practical life. • 1. Describe the morphological characteristics, life cycles, methods of transmission of medically important helminthes. • 2. Mention the morphological characteristics, life cycles, methods of transmission of medically important Protozoa. • 3. Describe the morphological characteristics, life cycles and recognize diseases caused or transmitted by medically important Arthropods. • 4. Discuss clinical picture associated with parasitic infections. • 5. List the different diagnostic techniques for detecting parasites. • 6. Outline the plan of treatment of each parasitic disease. • 7. Interpret different clinical presentations and correlate them to suspected parasites. • 8. Differentiate and compare similar stages of different parasites. • 9. Choose the most suitable diagnostic technique for each parasitic problem • 10. Use the light microscopy . • 1 1.Examine mounted slides and identify different parasites • 12.Examine laboratory specimens . • 13. Interpret the results of examination of parasitic specimens. Introduction to parasitology Objectives • 1- Aims to focus on general parasitological terms that will be discussed later on during the course. • 2-Gives general idea about life cycle, methods of infection and different harmful effects caused by parasitic infection. Introduction • A parasite is an organism which lives on or within another organism called -

List of ICD Codes (V.2009 and V.2012 ICD-10-CA¹)
List of ICD Codes (v.2009 and v.2012 ICD-10-CA¹) ICD Code Short Description Long Description A00 Cholera Cholera A00-A09 Intestinal infectious diseases Intestinal infectious diseases (A00-A09) A000 Cholera dt 01 biovar cholerae Cholera due to Vibrio cholerae 01, biovar cholerae A001 Cholera dt biovar eltor Cholera due to Vibrio cholerae 01, biovar eltor A009 Cholera unspecified Cholera, unspecified A01 Typhoid and paratyphoid fevers Typhoid and paratyphoid fevers A010 Typhoid fever Typhoid fever A011 Paratyphoid fever A Paratyphoid fever A A012 Paratyphoid fever B Paratyphoid fever B A013 Paratyphoid fever C Paratyphoid fever C A014 Paratyphoid fever unspecified Paratyphoid fever, unspecified A02 Other salmonella infections Other salmonella infections A020 Salmonella enteritis Salmonella enteritis A021 Salmonella sepsis Salmonella sepsis A022 Localized salmonella infections Localized salmonella infections A028 Other specified salmonella infections Other specified salmonella infections A029 Salmonella infection unspecified Salmonella infection, unspecified A03 Shigellosis Shigellosis A030 Shigellosis due to Shigella dysenteriae Shigellosis due to Shigella dysenteriae A031 Shigellosis due to Shigella flexneri Shigellosis due to Shigella flexneri A032 Shigellosis due to Shigella boydii Shigellosis due to Shigella boydii A033 Shigellosis due to Shigella sonnei Shigellosis due to Shigella sonnei A038 Other shigellosis Other shigellosis A039 Shigellosis unspecified Shigellosis, unspecified A04 Other bacterial intestinal infections Other bacterial -

Read Code Description 14L.. H/O: Drug Allergy 158.. H/O: Abnormal Uterine Bleeding 16C2
Read Code Description 14L.. H/O: drug allergy 158.. H/O: abnormal uterine bleeding 16C2. Backache 191.. Tooth symptoms 191Z. Tooth symptom NOS 1927. Dry mouth 198.. Nausea 199.. Vomiting 19C.. Constipation 1A23. Incontinence of urine 1A32. Cannot pass urine - retention 1B1G. Headache 1B62. Syncope/vasovagal faint 1B75. Loss of vision 1BA2. Generalised headache 1BA3. Unilateral headache 1BA4. Bilateral headache 1BA5. Frontal headache 1BA6. Occipital headache 1BA7. Parietal headache 1BA8. Temporal headache 1C13. Deafness 1C131 Unilateral deafness 1C132 Partial deafness 1C133 Bilateral deafness 1C14. "Blocked ear" 1C15. Popping sensation in ear 1C1Z. Hearing symptom NOS 22J.. O/E - dead 22J4. O/E - dead - sudden death 22L4. O/E - Wound infected 2542. O/E - dental caries 2554. O/E - gums - blue line 2555. O/E - hypertrophy of gums 2FF.. O/E - skin ulcer 2I14. O/E - a rash 39C0. Pressure sore 39C1. Superficial pressure sore 39C2. Deep pressure sore 62... Patient pregnant 6332. Single stillbirth 66G4. Allergy drug side effect 72001 Enucleation of eyeball 7443. Exteriorisation of trachea 744D. Tracheo-oesophageal puncture 7511. Surgical removal of tooth 75141 Root canal therapy to tooth 7610. Total excision of stomach 7645. Creation of ileostomy 773C. Other operations on bowel 773Cz Other operation on bowel NOS 7826. Incision of bile duct 7840. Total excision of spleen 7B01. Total nephrectomy 7C032 Unilateral total orchidectomy - unspecified 7E117 Left salpingoophorectomy 7E118 Right salpingectomy 7E119 Left salpingectomy 7G321 Avulsion of nail 7H220 Exploratory laparotomy 7J174 Manipulation of mandible 8HG.. Died in hospital 94B.. Cause of death A.... Infectious and parasitic diseases A0... Intestinal infectious diseases A00.. Cholera A000. -
Meddra Version 23.1)
Domenico Scarlattilaan 6 | 1083 HS Amsterdam | The Netherlands Telephone Tel +31(0)88 781 6000 E-mail [email protected] Website www.ema.europa.eu An agency of the European Union 14/09/2020 EMA/484057/2020 Human Medicines Division Important medical event terms list (MedDRA version 23.1) Primary SOC MedDRA Code PT Name SOC Name Comment Added in 23.1 Change This term fits the inclusion for an immune-mediated condition that is 10084828 Immune-mediated cytopenia Blood and lymphatic system disorders usually related to a drug. Similar PT Immune thrombocytopenia is already X included. In v23.0 this term was an LLT under the PT Bone marrow failure, which 10028584 Myelosuppression Blood and lymphatic system disorders X was included in the 23.0 IME list. This term fits the inclusion criteria as a relevant term for cardiac 10084280 Foetal cardiac arrest Cardiac disorders X arrhythmias. Similar PT Cardiac arrest is included in the IME list. In v23.0 this term was an LLT under the PT Cardiac valve replacement 10080073 Prosthetic cardiac valve stenosis Cardiac disorders X complication, which was included in the 23.0 IME list. Perinatal hepatitis C in pediatric patients may range from asymptomatic to fulminant hepatitis. Congenital hepatitis C infection can be associated with 10084252 Congenital hepatitis C infection Congenital, familial and genetic disorders X significant multi-organ damage which meets the criteria for inclusion in the IME list. Congenital viral hepatitis is a viral infection of the baby's liver which occurs when a pregnant woman infected with hepatitis virus passes the virus onto her unborn infant. -

Parasitic Infestations Requiring Surgical Interventions
Seminars in Pediatric Surgery (2012) 21, 142-150 Parasitic infestations requiring surgical interventions Afua A.J. Hesse, MD,a Abdellatif Nouri, MD,b Hussam S. Hassan, MD,c Amel A. Hashish, MD, CT, MHPEc From the aPediatric Surgery Unit, Department of Surgery, University of Ghana Medical School, Accra, Ghana; bDepartment of Pediatric Surgery, Fattouma Bourguiba Hospital, Monastir, Tunisia; and cFaculty of Medicine, Tanta University, Tanta University Hospital, Tanta, Egypt. KEYWORDS Parasitic infestation is common in developing countries especially in Africa. Children are often more Parasites; vulnerable to these infections. Many health problems result from these infestations, including malnu- Surgery; trition, iron-deficiency anemia, surgical morbidities, and even impaired cognitive function and educa- Africa; tional achievement. Surgical intervention may be needed to treat serious complications caused by some Children; of these parasites. Amoebic colitis and liver abscess caused by protozoan infections; intestinal obstruc- Amoebiasis; tion, biliary infestation with cholangitis and liver abscess, and pancreatitis caused by Ascaris lumbri- Ascariasis; coides; biliary obstruction caused by Faschiola; hepatic and pulmonary hydatid cysts caused by Dracontiasis; Echinococcus granulosus and multilocularis are examples. Expenditure of medical care of affected Schistosomiasis; children may cause a great burden on many African governments, which are already suffering from Hydatid; economic instability. The clinical presentation, investigation, and -

Parasitic Infections of the Nervous System, with An
PARASITIC INFECTIONS OF THE NERVOUS SYSTEM, WITH AN UPDATE ON FREE-LIVING AMOEBIC INFECTIONS 'NR de Silva, 2MKdeS Wijesundera Professor of Parasitology, Faculty of Medicine, University of Kelaniya, 2EmeritusProfessor of Parasitology, Faculty of Medicine, University of Peradeniya. the central nervous system, and the disease entities associated with these infections. h the central nervous system (CNS) of humans frequent site of primary infection by parasites, Parasitic infections of the CNS: causative agents tations when the CNS is involved. The second coccidia (Table I),while a range of nematodes, cestodes this article deals at greater length with the and trematodes are also known to cause neurological ae that are known to cause primary infections of disorders (Table 2). Amoebic brain abscess Naegleria fowleri Primary amoebic rneningo-encephalitis Acanthamoeba spp Granulomatous amoebic encephalitis, keratitis Balamufhia mandrilafls Granulomatous amoebic encephalitis Trypanosoma bruceirhodesiense Encephalitis (in Human African Trypanosomiasis or sleeping sickness) and T.b. gambiense Tr~panosomacruzi Encephalitis Msceral larva migrans Eosinophiliimeningo -encephalitis Epilepsy or encephalitis Onchocerca volvulus Encephalopathy a Encephabpathy Neurocysticercosis gives rise to epilepsy, hydrocephalus or organic dementia Echinococcus granulosus Hydatid cyst of the brain or spinal cord Echinococcus rnultilocularis Alveolar echinococcosis Cerebral sparganosis, seizures Schisfosomajaponlcum Schistosoma mansoni Paragonimus westerinani Seizures I 49 (primary or re-activated infection) is well known to cause nwml~imldisease in immunmm~romisedPatients, Among the other trematodes, Paragonimus westerm particularlythosewith organ bns~lanband HIV/AIDS. causing paragonimiasisis a major cause of neurologi Cases of ence~halo~ath~temporally related to mass disease in the Far East, due to cyst formation in ecto tw&nent with i~ermedinfor onchocerciasis have been sits in the brain and presents as intracranial spa reported; most of these cases recovered without serious mupying lesions.