Parasitic Infestations Requiring Surgical Interventions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
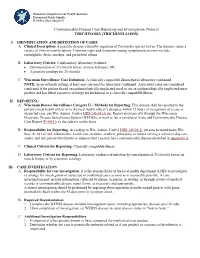
Trichinosis (Trichinellosis) Case Reporting and Investigation Protocol
Wisconsin Department of Health Services Division of Public Health P-01912 (Rev 08/2017) Communicable Disease Case Reporting and Investigation Protocol TRICHINOSIS (TRICHINELLOSIS) I. IDENTIFICATION AND DEFINITION OF CASES A. Clinical Description: A parasitic disease caused by ingestion of Trichinella species larvae. The disease causes a variety of clinical manifestations. Common signs and symptoms among symptomatic persons include eosinophilia, fever, myalgia, and periorbital edema. B. Laboratory Criteria: Confirmatory laboratory evidence: • Demonstration of Trichinella larvae on muscle biopsy, OR • A positive serology for Trichinella. C. Wisconsin Surveillance Case Definition: A clinically compatible illness that is laboratory confirmed. NOTE: In an outbreak setting, at least one case must be laboratory confirmed. Associated cases are considered confirmed if the patient shared an epidemiologically implicated meal or ate an epidemiologically implicated meat product and has either a positive serology for trichinosis or a clinically compatible illness. II. REPORTING A. Wisconsin Disease Surveillance Category II – Methods for Reporting: This disease shall be reported to the patient’s local health officer or to the local health officer’s designee within 72 hours of recognition of a case or suspected case, per Wis. Admin. Code § DHS 145.04 (3) (b). Report electronically through the Wisconsin Electronic Disease Surveillance System (WEDSS), or mail or fax a completed Acute and Communicable Disease Case Report (F-44151) to the address on the form. B. Responsibility for Reporting: According to Wis. Admin. Code § DHS 145.04(1), persons licensed under Wis. Stat. ch. 441 or 448, laboratories, health care facilities, teachers, principals, or nurses serving a school or day care center, and any person who knows or suspects that a person has a communicable disease identified in Appendix A. -

Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

Onchocerciasis
11 ONCHOCERCIASIS ADRIAN HOPKINS AND BOAKYE A. BOATIN 11.1 INTRODUCTION the infection is actually much reduced and elimination of transmission in some areas has been achieved. Differences Onchocerciasis (or river blindness) is a parasitic disease in the vectors in different regions of Africa, and differences in cause by the filarial worm, Onchocerca volvulus. Man is the the parasite between its savannah and forest forms led to only known animal reservoir. The vector is a small black fly different presentations of the disease in different areas. of the Simulium species. The black fly breeds in well- It is probable that the disease in the Americas was brought oxygenated water and is therefore mostly associated with across from Africa by infected people during the slave trade rivers where there is fast-flowing water, broken up by catar- and found different Simulium flies, but ones still able to acts or vegetation. All populations are exposed if they live transmit the disease (3). Around 500,000 people were at risk near the breeding sites and the clinical signs of the disease in the Americas in 13 different foci, although the disease has are related to the amount of exposure and the length of time recently been eliminated from some of these foci, and there is the population is exposed. In areas of high prevalence first an ambitious target of eliminating the transmission of the signs are in the skin, with chronic itching leading to infection disease in the Americas by 2012. and chronic skin changes. Blindness begins slowly with Host factors may also play a major role in the severe skin increasingly impaired vision often leading to total loss of form of the disease called Sowda, which is found mostly in vision in young adults, in their early thirties, when they northern Sudan and in Yemen. -

Taenia Solium Transmission in a Rural Community in ·Honduras: an Examination of Risk Factors and Knowledge
Taenia solium Transmission in a Rural Community in ·Honduras: An Examination of Risk Factors and Knowledge by Haiyan Pang Faculty of Applied Health Sciences Brock University A thesis submitted for completion of the Master of Science Degree Haiyan Pang © 2004 lAMES A GIBSON LIBRARY . BROCK UNIVERSITY sr. CAtHARINES· ON Abstract Taenia soliurn taeniasis and cysticercosis are recognized as a major public health problem in Latin America. T. soliurn transmission not only affects the health of the individual, but also social and economic development, perpetuating the cycle of poverty. To determine prevalence rates, population knowledge and risk factors associated with transmission, anepidemiological study was undertaken in the rural community of Jalaca. Two standardized questionnaires were used to collect epidemiological and T. soli urn general knowledge data. Kato-Katz technique and an immunoblot assay (EITB) were used to determine taeniasis and seroprevalence, respectively. In total, 139 individuals belonging to 56 households participated in the study. Household characteristics were consistent with conditions of poverty of rural Honduras: 21.4% had no toilet or latrines, 19.6% had earthen floor, and 51.8% lacked indoor tap water. Pigs were raised in 46.4% of households, of which 70% allowed their pigs roaming freely. A human seroprevalence rate of 18.7% and a taeniasis prevalence rate of 2.4% were found. Only four persons answered correctly 2: 6 out of ten T. soliurn knowledge questions, for an average passing score of 2.9%. In general, a serious gap exists in knowledge regarding how humans acquire the infections, especially neurocysticercosis was identified. After regression analysis, the ability to recognize adult tapeworms and awareness of the clinical importance of taeniasis, were found to be significant risk factors for T. -

Lecture 5: Emerging Parasitic Helminths Part 2: Tissue Nematodes
Readings-Nematodes • Ch. 11 (pp. 290, 291-93, 295 [box 11.1], 304 [box 11.2]) • Lecture 5: Emerging Parasitic Ch.14 (p. 375, 367 [table 14.1]) Helminths part 2: Tissue Nematodes Matt Tucker, M.S., MSPH [email protected] HSC4933 Emerging Infectious Diseases HSC4933. Emerging Infectious Diseases 2 Monsters Inside Me Learning Objectives • Toxocariasis, larva migrans (Toxocara canis, dog hookworm): • Understand how visceral larval migrans, cutaneous larval migrans, and ocular larval migrans can occur Background: • Know basic attributes of tissue nematodes and be able to distinguish http://animal.discovery.com/invertebrates/monsters-inside- these nematodes from each other and also from other types of me/toxocariasis-toxocara-roundworm/ nematodes • Understand life cycles of tissue nematodes, noting similarities and Videos: http://animal.discovery.com/videos/monsters-inside- significant difference me-toxocariasis.html • Know infective stages, various hosts involved in a particular cycle • Be familiar with diagnostic criteria, epidemiology, pathogenicity, http://animal.discovery.com/videos/monsters-inside-me- &treatment toxocara-parasite.html • Identify locations in world where certain parasites exist • Note drugs (always available) that are used to treat parasites • Describe factors of tissue nematodes that can make them emerging infectious diseases • Be familiar with Dracunculiasis and status of eradication HSC4933. Emerging Infectious Diseases 3 HSC4933. Emerging Infectious Diseases 4 Lecture 5: On the Menu Problems with other hookworms • Cutaneous larva migrans or Visceral Tissue Nematodes larva migrans • Hookworms of other animals • Cutaneous Larva Migrans frequently fail to penetrate the human dermis (and beyond). • Visceral Larva Migrans – Ancylostoma braziliense (most common- in Gulf Coast and tropics), • Gnathostoma spp. Ancylostoma caninum, Ancylostoma “creeping eruption” ceylanicum, • Trichinella spiralis • They migrate through the epidermis leaving typical tracks • Dracunculus medinensis • Eosinophilic enteritis-emerging problem in Australia HSC4933. -

STUDY of PARASITIC INFESTATION and ITS EFFECT on the HEALTH STATUS of PRIMARY SCHOOL CHILDREN in TANTA CITY Nour Abd El Azize Mohammed Mealy, Prof
STUDY OF PARASITIC INFESTATION AND ITS EFFECT ON THE HEALTH STATUS OF PRIMARY SCHOOL CHILDREN IN TANTA CITY Nour Abd El Azize Mohammed Mealy, Prof. Dr. Nadia Yahia Ismaiel, Prof. Dr. Hassan Saad Abu Saif, Prof. Dr. Wael Refaat Hablas STUDY OF PARASITIC INFESTATION AND ITS EFFECT ON THE HEALTH STATUS OF PRIMARY SCHOOL CHILDREN IN TANTA CITY By Nour Abd El Azize Mohammed Mealy, Prof. Dr. Nadia Yahia Ismaiel*, Prof. Dr. Hassan Saad Abu Saif*, Prof. Dr. Wael Refaat Hablas** Pediatric*& Clinical Pathology** Depts. Al-Azhar University- Faculty of Medicine ABSTRACT Background: School age children are one of the groups at high-risk for intestinal parasitic infestations. Factors like poor developments of hygienic habits, immune system and over-crowding contributes for infestation. The adverse effects of intestinal parasites among children are diverse and alarming. Intestinal parasitic infestations have detrimental effects on the survival, appetite, growth and physical fitness, school attendance and cognitive performance of school age children (Alemu et al., 2011). Objectives: We aimed to 1. Assess the prevalence of parasitic infestation and its effect on the health status of primary school children in Tanta City (5 schools from 3 areas at Tanta city) 2. Determine the prevalence of intestinal parasitic infestation among primary school children in some urban communities of Tanta City 3. Identify associated risk factors of school children for parasitic infestations in some urban communities of Tanta City. Design: This is descriptive cross sectional study that was carried out on 1000 students (boys &girls) at governmental primary schools at Tanta rural areas. This research was continued until fulfillment of the study from April 2017 to May 2018. -

Molecular Detection of Human Parasitic Pathogens
MOLECULAR DETECTION OF HUMAN PARASITIC PATHOGENS MOLECULAR DETECTION OF HUMAN PARASITIC PATHOGENS EDITED BY DONGYOU LIU Boca Raton London New York CRC Press is an imprint of the Taylor & Francis Group, an informa business CRC Press Taylor & Francis Group 6000 Broken Sound Parkway NW, Suite 300 Boca Raton, FL 33487-2742 © 2013 by Taylor & Francis Group, LLC CRC Press is an imprint of Taylor & Francis Group, an Informa business No claim to original U.S. Government works Version Date: 20120608 International Standard Book Number-13: 978-1-4398-1243-3 (eBook - PDF) This book contains information obtained from authentic and highly regarded sources. Reasonable efforts have been made to publish reliable data and information, but the author and publisher cannot assume responsibility for the validity of all materials or the consequences of their use. The authors and publishers have attempted to trace the copyright holders of all material reproduced in this publication and apologize to copyright holders if permission to publish in this form has not been obtained. If any copyright material has not been acknowledged please write and let us know so we may rectify in any future reprint. Except as permitted under U.S. Copyright Law, no part of this book may be reprinted, reproduced, transmitted, or utilized in any form by any electronic, mechanical, or other means, now known or hereafter invented, including photocopying, microfilming, and recording, or in any information storage or retrieval system, without written permission from the publishers. For permission to photocopy or use material electronically from this work, please access www.copyright.com (http://www.copyright.com/) or contact the Copyright Clearance Center, Inc. -

Infestation in a Central Nigerian Rural Community * ANOSIKE, JC
J. Appl. Sci. Environ. Mgt. June, 2006 JASEM ISSN 1119-8362 Full-text Available Online at All rights reserved www.bioline.org.br/ja Vol. 10 (2) 61 - 66 Studies on the Intestinal Worm (Helminthiasis) infestation in a Central Nigerian Rural Community *1ANOSIKE, JC; 1ZACCHEAUS, VO; 1ADEIYONGO, CM; 2ABANOBI, OC; 1DADA, EO; 3OKU, EE; 1KEKE, IR; 4UWAEZUOKE, JC; 4AMAJUOYI, OU; 5OBIUKWU, CE; 4NWOSU, DC; 4OGBUSU, FI 1Department of Zoology, University of Jos P.M.B. 2084, Jos, Plateau State, Nigeria 2Department of Community Medicine, College of Medicine and Health Sciences, Abia State, University, Uturu, Nigeria 3Department of Biological Sciences, University of Calabar, Nigeria 4Department of Animal & Environmental Biology, Imo State University, Owerri, Nigeria. 5Department of Industrial Microbiology, Imo State University, Owerri, Nigeria. E-mail: [email protected] ABSTRACT: The prevalence of intestinal helminth of residents of Naraguta rural community in Central Nigeria is presented. Out of 700 stool specimens examined between January and July 1999, 261 (37.3%) were positive for helminthic infections. Helminths encountered include Hookworm, Schistosoma mansoni, Trichuris trichiura, Strongyloides stercoralis, Ascaris lumbricoides, and Hymenolepis nana. Hookworm was the most predominant, followed by S. stercoralis, S. mansoni and A. lumbricoides with T. trichiura as the least. Intestinal helminthiasis was equally prevalent for males and females. However, infection rates were high among persons below ten years of age, in toddlers, housewives and farmers than others. Persons defecating in the bush harbored more worms (56.7%) than pit latrine users (43.3%). Free medical diagnosis in most rural communities in Nigeria are probably justifiable and should be promoted and/or sustained by government. -

Public Health Significance of Intestinal Parasitic Infections*
Articles in the Update series Les articles de la rubrique give a concise, authoritative, Le pointfournissent un bilan and up-to-date survey of concis et fiable de la situa- the present position in the tion actuelle dans les do- Update selectedfields, coveringmany maines consideres, couvrant different aspects of the de nombreux aspects des biomedical sciences and sciences biomedicales et de la , po n t , , public health. Most of santepublique. Laplupartde the articles are written by ces articles auront donc ete acknowledged experts on the redigeis par les specialistes subject. les plus autorises. Bulletin of the World Health Organization, 65 (5): 575-588 (1987) © World Health Organization 1987 Public health significance of intestinal parasitic infections* WHO EXPERT COMMITTEE' Intestinal parasitic infections are distributed virtually throughout the world, with high prevalence rates in many regions. Amoebiasis, ascariasis, hookworm infection and trichuriasis are among the ten most common infections in the world. Other parasitic infections such as abdominal angiostrongyliasis, intestinal capil- lariasis, and strongyloidiasis are of local or regional public health concern. The prevention and control of these infections are now more feasible than ever before owing to the discovery of safe and efficacious drugs, the improvement and sim- plification of some diagnostic procedures, and advances in parasite population biology. METHODS OF ASSESSMENT The amount of harm caused by intestinal parasitic infections to the health and welfare of individuals and communities depends on: (a) the parasite species; (b) the intensity and course of the infection; (c) the nature of the interactions between the parasite species and concurrent infections; (d) the nutritional and immunological status of the population; and (e) numerous socioeconomic factors. -
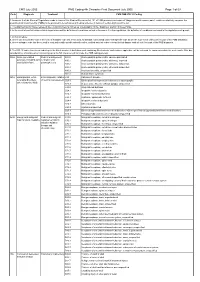
CMS PMB ICD-10 Coding
CMS July 2005 PMB Coding 4th Character Final Dcoument July 2005 Page 1 of 69 Code Diagnosis Treatment CMS PMB ICD-10 Coding 1. Annexure A of the General Regulations made in terms of the Medical Schemes Act, 131 of 1998 provides a schedule of “diagnosis and treatment pairs”, which cumulatively comprise the prescribed minimum benefits (PMBs) to be provided to beneficiaries of medical schemes in terms of section 29(1)(o) of the Act. 2. The attached ICD10 codes represent the Council for Medical Schemes’ interpretation of the “diagnosis” portion of these PMBs. 3. In the event of conflict between this interpretation and the definition of conditions set out in Annexure A to the regulations, the definition of conditions contained in the regulations will prevail. 4. In this schedule: a. where only the primary code in the form of a dagger code has been used, all asterisk codes listed under that specific code as per the ICD-10 set of books form part of the PMB diagnosis; b. where a dagger code has been used in conjunction with specific asterisk codes, omitted asterisk codes relevant to that dagger code do not form part of the PMB diagnosis. 5. The ICD-10 codes have been coded up to the 4th character. A draft document containing 5th character codes where applicable, will be released for comments within the next month. After due consideration, a final document containing up to the 5th character will conclude the PMB coding process. 906A Acute generalised Medical management; A80.0 Acute paralytic poliomyelitis, vaccine-associated paralysis, including -

Hymenolepiasis in a Pregnant Woman: a Case Report of Hymenolepis Nana Infection
Open Access Case Report DOI: 10.7759/cureus.3810 Hymenolepiasis in a Pregnant Woman: A Case Report of Hymenolepis nana Infection Venkataramana Kandi 1 , Sri Sandhya Koka 1 , Mohan Rao Bhoomigari 1 1. Microbiology, Prathima Institute of Medical Sciences, Karimnagar, IND Corresponding author: Venkataramana Kandi, [email protected] Abstract Hymenolepiasis is an infection caused by Hymenolepis nana (H. nana) and H. diminuta (H. diminuta). Hymenolepiasis is prevalent throughout the world with human infections with H. nana being frequently reported in the literature as compared to H. diminuta. Hymenolepiasis is more frequent among children, and most human infections remain asymptomatic and self-limited. Symptoms including abdominal pain, diarrhea, and vomiting are frequently noted in the cases of heavy infections. We report a case of hymenolepiasis caused by H. nana in a pregnant woman. Categories: Obstetrics/Gynecology, Infectious Disease, Public Health Keywords: hymenolepiasis, hymenolepis nana, h. nana, h. diminuta, children, adults, asymptomatic, pregnant woman Introduction Human infection caused by the cestodes belonging to the genus Hymenolepis is called as hymenolepiasis. The cestodes are broadly classified as pseudophyllidean and cyclophyllidean cestodes. Hymenolepis species (spp.) fall into the cyclophyllidean group, which is characterized by the presence of four cup-like structures in the scolex/head called as suckers. The suckers are either armed (presence of hook-like structures) or unarmed (no hooks). Hymenolepis spp. are armed with the presence of a single round of hooks around the suckers. Among the Hymenolepis spp., H. nana is commonly called as a dwarf tapeworm and H. diminuta is referred to as a rat tapeworm. H. nana frequently causes human infections and may also cause infections in rats, whereas H. -

2011/109440 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date _ . 9 September 2011 (09.09.2011) 2011/109440 Al (51) International Patent Classification: [CH/CH]; Chemin Des Chevreuils 1, 1188 Gimel (CH). C12Q 1/68 (2006.01) G01N 33/53 (2006.01) HOLTERMAN, Daniel [US/US]; 14465 North 14th St., Phoenix, AZ 85022 (US). (21) International Application Number: PCT/US201 1/026750 (74) Agent: AKHAVAN, Ramin; Caris Life Sciences, Inc., 6655 N. MacArthur Blvd., Irving, TX 75039 (US). (22) International Filing Date: 1 March 201 1 (01 .03.201 1) (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, English (25) Filing Language: AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (26) Publication Language: English CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (30) Priority Data: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 61/274,124 1 March 2010 (01 .03.2010) US KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 61/357,5 17 22 June 2010 (22.06.2010) US ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 61/364,785 15 July 2010 (15.07.2010) us NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (71) Applicant (for all designated States except US): CARIS SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, LIFE SCIENCES LUXEMBOURG HOLDINGS [LU/ TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW.