Chronic Symptomatic and Microfilaremic Loiasis in a Returned Traveller
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Gnathostoma Spinigerum Was Positive
Department Medicine Diagnostic Centre Swiss TPH Winter Symposium 2017 Helminth Infection – from Transmission to Control Sushi Worms – Diagnostic Challenges Beatrice Nickel Fish-borne helminth infections Consumption of raw or undercooked fish - Anisakis spp. infections - Gnathostoma spp. infections Case 1 • 32 year old man • Admitted to hospital with severe gastric pain • Abdominal pain below ribs since a week, vomiting • Low-grade fever • Physical examination: moderate abdominal tenderness • Laboratory results: mild leucocytosis • Patient revealed to have eaten sushi recently • Upper gastrointestinal endoscopy was performed Carmo J, et al. BMJ Case Rep 2017. doi:10.1136/bcr-2016-218857 Case 1 Endoscopy revealed 2-3 cm long helminth Nematode firmly attached to / Endoscopic removal of larva with penetrating gastric mucosa a Roth net Carmo J, et al. BMJ Case Rep 2017. doi:10.1136/bcr-2016-218857 Anisakiasis Human parasitic infection of gastrointestinal tract by • herring worm, Anisakis spp. (A.simplex, A.physeteris) • cod worm, Pseudoterranova spp. (P. decipiens) Consumption of raw or undercooked seafood containing infectious larvae Highest incidence in countries where consumption of raw or marinated fish dishes are common: • Japan (sashimi, sushi) • Scandinavia (cod liver) • Netherlands (maatjes herrings) • Spain (anchovies) • South America (ceviche) Source: http://parasitewonders.blogspot.ch Life Cycle of Anisakis simplex (L1-L2 larvae) L3 larvae L2 larvae L3 larvae Source: Adapted to Audicana et al, TRENDS in Parasitology Vol.18 No. 1 January 2002 Symptoms Within few hours of ingestion, the larvae try to penetrate the gastric/intestinal wall • acute gastric pain or abdominal pain • low-grade fever • nausea, vomiting • allergic reaction possible, urticaria • local inflammation Invasion of the third-stage larvae into gut wall can lead to eosinophilic granuloma, ulcer or even perforation. -

The Functional Parasitic Worm Secretome: Mapping the Place of Onchocerca Volvulus Excretory Secretory Products
pathogens Review The Functional Parasitic Worm Secretome: Mapping the Place of Onchocerca volvulus Excretory Secretory Products Luc Vanhamme 1,*, Jacob Souopgui 1 , Stephen Ghogomu 2 and Ferdinand Ngale Njume 1,2 1 Department of Molecular Biology, Institute of Biology and Molecular Medicine, IBMM, Université Libre de Bruxelles, Rue des Professeurs Jeener et Brachet 12, 6041 Gosselies, Belgium; [email protected] (J.S.); [email protected] (F.N.N.) 2 Molecular and Cell Biology Laboratory, Biotechnology Unit, University of Buea, Buea P.O Box 63, Cameroon; [email protected] * Correspondence: [email protected] Received: 28 October 2020; Accepted: 18 November 2020; Published: 23 November 2020 Abstract: Nematodes constitute a very successful phylum, especially in terms of parasitism. Inside their mammalian hosts, parasitic nematodes mainly dwell in the digestive tract (geohelminths) or in the vascular system (filariae). One of their main characteristics is their long sojourn inside the body where they are accessible to the immune system. Several strategies are used by parasites in order to counteract the immune attacks. One of them is the expression of molecules interfering with the function of the immune system. Excretory-secretory products (ESPs) pertain to this category. This is, however, not their only biological function, as they seem also involved in other mechanisms such as pathogenicity or parasitic cycle (molting, for example). Wewill mainly focus on filariae ESPs with an emphasis on data available regarding Onchocerca volvulus, but we will also refer to a few relevant/illustrative examples related to other worm categories when necessary (geohelminth nematodes, trematodes or cestodes). -
Trichinosis (Trichinellosis) Case Reporting and Investigation Protocol
Wisconsin Department of Health Services Division of Public Health P-01912 (Rev 08/2017) Communicable Disease Case Reporting and Investigation Protocol TRICHINOSIS (TRICHINELLOSIS) I. IDENTIFICATION AND DEFINITION OF CASES A. Clinical Description: A parasitic disease caused by ingestion of Trichinella species larvae. The disease causes a variety of clinical manifestations. Common signs and symptoms among symptomatic persons include eosinophilia, fever, myalgia, and periorbital edema. B. Laboratory Criteria: Confirmatory laboratory evidence: • Demonstration of Trichinella larvae on muscle biopsy, OR • A positive serology for Trichinella. C. Wisconsin Surveillance Case Definition: A clinically compatible illness that is laboratory confirmed. NOTE: In an outbreak setting, at least one case must be laboratory confirmed. Associated cases are considered confirmed if the patient shared an epidemiologically implicated meal or ate an epidemiologically implicated meat product and has either a positive serology for trichinosis or a clinically compatible illness. II. REPORTING A. Wisconsin Disease Surveillance Category II – Methods for Reporting: This disease shall be reported to the patient’s local health officer or to the local health officer’s designee within 72 hours of recognition of a case or suspected case, per Wis. Admin. Code § DHS 145.04 (3) (b). Report electronically through the Wisconsin Electronic Disease Surveillance System (WEDSS), or mail or fax a completed Acute and Communicable Disease Case Report (F-44151) to the address on the form. B. Responsibility for Reporting: According to Wis. Admin. Code § DHS 145.04(1), persons licensed under Wis. Stat. ch. 441 or 448, laboratories, health care facilities, teachers, principals, or nurses serving a school or day care center, and any person who knows or suspects that a person has a communicable disease identified in Appendix A. -

Toxocariasis: a Rare Cause of Multiple Cerebral Infarction Hyun Hee Kwon Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu, Korea
Case Report Infection & http://dx.doi.org/10.3947/ic.2015.47.2.137 Infect Chemother 2015;47(2):137-141 Chemotherapy ISSN 2093-2340 (Print) · ISSN 2092-6448 (Online) Toxocariasis: A Rare Cause of Multiple Cerebral Infarction Hyun Hee Kwon Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu, Korea Toxocariasis is a parasitic infection caused by the roundworms Toxocara canis or Toxocara cati, mostly due to accidental in- gestion of embryonated eggs. Clinical manifestations vary and are classified as visceral larva migrans or ocular larva migrans according to the organs affected. Central nervous system involvement is an unusual complication. Here, we report a case of multiple cerebral infarction and concurrent multi-organ involvement due to T. canis infestation of a previous healthy 39-year- old male who was admitted for right leg weakness. After treatment with albendazole, the patient’s clinical and laboratory results improved markedly. Key Words: Toxocara canis; Cerebral infarction; Larva migrans, visceral Introduction commonly involved organs [4]. Central nervous system (CNS) involvement is relatively rare in toxocariasis, especially CNS Toxocariasis is a parasitic infection caused by infection with presenting as multiple cerebral infarction. We report a case of the roundworm species Toxocara canis or less frequently multiple cerebral infarction with lung and liver involvement Toxocara cati whose hosts are dogs and cats, respectively [1]. due to T. canis infection in a previously healthy patient who Humans become infected accidentally by ingestion of embry- was admitted for right leg weakness. onated eggs from contaminated soil or dirty hands, or by in- gestion of raw organs containing encapsulated larvae [2]. -

Molecular Identification of the Etiological Agent of Human
Jpn. J. Infect. Dis., 73, 44–50, 2020 Original Article Molecular Identification of the Etiological Agent of Human Gnathostomiasis in an Endemic Area of Mexico Sylvia Paz Díaz-Camacho1, Jesús Ricardo Parra-Unda2, Julián Ríos-Sicairos2, and Francisco Delgado-Vargas2* 1Research Unit in Environment and Health, Autonomous University of Occident, Sinaloa; and 2Public Health Research Unit "Dra. Kaethe Willms", School of Chemical and Biological Sciences, Autonomous University of Sinaloa, University city, Culiacan, Sinaloa, Mexico SUMMARY: Human gnathostomiasis, which is endemic in Mexico, is a worldwide health concern. It is mainly caused by the consumption of raw or insufficiently cooked fish containing the advanced third-stage larvae (AL3A) of Gnathostoma species. The diagnosis of gnathostomiasis is based on epidemiological surveys and immunological diagnostic tests. When a larva is recovered, the species can be identified by molecular techniques. Polymerase chain reaction (PCR) amplification of the second internal transcription spacer (ITS-2) is useful to identify nematode species, including Gnathostoma species. This study aims to develop a duplex-PCR amplification method of the ITS-2 region to differentiate between the Gnathostoma binucleatum and G. turgidum parasites that coexist in the same endemic area, as well as to identify the Gnathostoma larvae recovered from the biopsies of two gnathostomiasis patients from Sinaloa, Mexico. The duplex PCR established based on the ITS- 2 sequence showed that the length of the amplicons was 321 bp for G. binucleatum and 226 bp for G. turgidum. The amplicons from the AL3A of both patients were 321 bp. Furthermore, the length and composition of these amplicons were identical to those deposited in GenBank as G. -

Onchocerciasis
11 ONCHOCERCIASIS ADRIAN HOPKINS AND BOAKYE A. BOATIN 11.1 INTRODUCTION the infection is actually much reduced and elimination of transmission in some areas has been achieved. Differences Onchocerciasis (or river blindness) is a parasitic disease in the vectors in different regions of Africa, and differences in cause by the filarial worm, Onchocerca volvulus. Man is the the parasite between its savannah and forest forms led to only known animal reservoir. The vector is a small black fly different presentations of the disease in different areas. of the Simulium species. The black fly breeds in well- It is probable that the disease in the Americas was brought oxygenated water and is therefore mostly associated with across from Africa by infected people during the slave trade rivers where there is fast-flowing water, broken up by catar- and found different Simulium flies, but ones still able to acts or vegetation. All populations are exposed if they live transmit the disease (3). Around 500,000 people were at risk near the breeding sites and the clinical signs of the disease in the Americas in 13 different foci, although the disease has are related to the amount of exposure and the length of time recently been eliminated from some of these foci, and there is the population is exposed. In areas of high prevalence first an ambitious target of eliminating the transmission of the signs are in the skin, with chronic itching leading to infection disease in the Americas by 2012. and chronic skin changes. Blindness begins slowly with Host factors may also play a major role in the severe skin increasingly impaired vision often leading to total loss of form of the disease called Sowda, which is found mostly in vision in young adults, in their early thirties, when they northern Sudan and in Yemen. -

CDC Overseas Parasite Guidelines
Guidelines for Overseas Presumptive Treatment of Strongyloidiasis, Schistosomiasis, and Soil-Transmitted Helminth Infections for Refugees Resettling to the United States U.S. Department of Health and Human Services Centers for Disease Control and Prevention National Center for Emerging and Zoonotic Infectious Diseases Division of Global Migration and Quarantine February 6, 2019 Accessible version: https://www.cdc.gov/immigrantrefugeehealth/guidelines/overseas/intestinal- parasites-overseas.html 1 Guidelines for Overseas Presumptive Treatment of Strongyloidiasis, Schistosomiasis, and Soil-Transmitted Helminth Infections for Refugees Resettling to the United States UPDATES--the following are content updates from the previous version of the overseas guidance, which was posted in 2008 • Latin American and Caribbean refugees are now included, in addition to Asian, Middle Eastern, and African refugees. • Recommendations for management of Strongyloides in refugees from Loa loa endemic areas emphasize a screen-and-treat approach and de-emphasize a presumptive high-dose albendazole approach. • Presumptive use of albendazole during any trimester of pregnancy is no longer recommended. • Links to a new table for the Treatment Schedules for Presumptive Parasitic Infections for U.S.-Bound Refugees, administered by IOM. Contents • Summary of Recommendations • Background • Recommendations for overseas presumptive treatment of intestinal parasites o Refugees originating from the Middle East, Asia, North Africa, Latin America, and the Caribbean o Refugees -

Gnathostomiasis: an Emerging Imported Disease David A.J
RESEARCH Gnathostomiasis: An Emerging Imported Disease David A.J. Moore,* Janice McCroddan,† Paron Dekumyoy,‡ and Peter L. Chiodini† As the scope of international travel expands, an ous complication of central nervous system involvement increasing number of travelers are coming into contact with (4). This form is manifested by painful radiculopathy, helminthic parasites rarely seen outside the tropics. As a which can lead to paraplegia, sometimes following an result, the occurrence of Gnathostoma spinigerum infection acute (eosinophilic) meningitic illness. leading to the clinical syndrome gnathostomiasis is increas- We describe a series of patients in whom G. spinigerum ing. In areas where Gnathostoma is not endemic, few cli- nicians are familiar with this disease. To highlight this infection was diagnosed at the Hospital for Tropical underdiagnosed parasitic infection, we describe a case Diseases, London; they were treated over a 12-month peri- series of patients with gnathostomiasis who were treated od. Four illustrative case histories are described in detail. during a 12-month period at the Hospital for Tropical This case series represents a small proportion of gnathos- Diseases, London. tomiasis patients receiving medical care in the United Kingdom, in whom this uncommon parasitic infection is mostly undiagnosed. he ease of international travel in the 21st century has resulted in persons from Europe and other western T Methods countries traveling to distant areas of the world and return- The case notes of patients in whom gnathostomiasis ing with an increasing array of parasitic infections rarely was diagnosed at the Hospital for Tropical Diseases were seen in more temperate zones. One example is infection reviewed retrospectively for clinical symptoms and confir- with Gnathostoma spinigerum, which is acquired by eating uncooked food infected with the larval third stage of the helminth; such foods typically include fish, shrimp, crab, crayfish, frog, or chicken. -

Lecture 5: Emerging Parasitic Helminths Part 2: Tissue Nematodes
Readings-Nematodes • Ch. 11 (pp. 290, 291-93, 295 [box 11.1], 304 [box 11.2]) • Lecture 5: Emerging Parasitic Ch.14 (p. 375, 367 [table 14.1]) Helminths part 2: Tissue Nematodes Matt Tucker, M.S., MSPH [email protected] HSC4933 Emerging Infectious Diseases HSC4933. Emerging Infectious Diseases 2 Monsters Inside Me Learning Objectives • Toxocariasis, larva migrans (Toxocara canis, dog hookworm): • Understand how visceral larval migrans, cutaneous larval migrans, and ocular larval migrans can occur Background: • Know basic attributes of tissue nematodes and be able to distinguish http://animal.discovery.com/invertebrates/monsters-inside- these nematodes from each other and also from other types of me/toxocariasis-toxocara-roundworm/ nematodes • Understand life cycles of tissue nematodes, noting similarities and Videos: http://animal.discovery.com/videos/monsters-inside- significant difference me-toxocariasis.html • Know infective stages, various hosts involved in a particular cycle • Be familiar with diagnostic criteria, epidemiology, pathogenicity, http://animal.discovery.com/videos/monsters-inside-me- &treatment toxocara-parasite.html • Identify locations in world where certain parasites exist • Note drugs (always available) that are used to treat parasites • Describe factors of tissue nematodes that can make them emerging infectious diseases • Be familiar with Dracunculiasis and status of eradication HSC4933. Emerging Infectious Diseases 3 HSC4933. Emerging Infectious Diseases 4 Lecture 5: On the Menu Problems with other hookworms • Cutaneous larva migrans or Visceral Tissue Nematodes larva migrans • Hookworms of other animals • Cutaneous Larva Migrans frequently fail to penetrate the human dermis (and beyond). • Visceral Larva Migrans – Ancylostoma braziliense (most common- in Gulf Coast and tropics), • Gnathostoma spp. Ancylostoma caninum, Ancylostoma “creeping eruption” ceylanicum, • Trichinella spiralis • They migrate through the epidermis leaving typical tracks • Dracunculus medinensis • Eosinophilic enteritis-emerging problem in Australia HSC4933. -

STUDY of PARASITIC INFESTATION and ITS EFFECT on the HEALTH STATUS of PRIMARY SCHOOL CHILDREN in TANTA CITY Nour Abd El Azize Mohammed Mealy, Prof
STUDY OF PARASITIC INFESTATION AND ITS EFFECT ON THE HEALTH STATUS OF PRIMARY SCHOOL CHILDREN IN TANTA CITY Nour Abd El Azize Mohammed Mealy, Prof. Dr. Nadia Yahia Ismaiel, Prof. Dr. Hassan Saad Abu Saif, Prof. Dr. Wael Refaat Hablas STUDY OF PARASITIC INFESTATION AND ITS EFFECT ON THE HEALTH STATUS OF PRIMARY SCHOOL CHILDREN IN TANTA CITY By Nour Abd El Azize Mohammed Mealy, Prof. Dr. Nadia Yahia Ismaiel*, Prof. Dr. Hassan Saad Abu Saif*, Prof. Dr. Wael Refaat Hablas** Pediatric*& Clinical Pathology** Depts. Al-Azhar University- Faculty of Medicine ABSTRACT Background: School age children are one of the groups at high-risk for intestinal parasitic infestations. Factors like poor developments of hygienic habits, immune system and over-crowding contributes for infestation. The adverse effects of intestinal parasites among children are diverse and alarming. Intestinal parasitic infestations have detrimental effects on the survival, appetite, growth and physical fitness, school attendance and cognitive performance of school age children (Alemu et al., 2011). Objectives: We aimed to 1. Assess the prevalence of parasitic infestation and its effect on the health status of primary school children in Tanta City (5 schools from 3 areas at Tanta city) 2. Determine the prevalence of intestinal parasitic infestation among primary school children in some urban communities of Tanta City 3. Identify associated risk factors of school children for parasitic infestations in some urban communities of Tanta City. Design: This is descriptive cross sectional study that was carried out on 1000 students (boys &girls) at governmental primary schools at Tanta rural areas. This research was continued until fulfillment of the study from April 2017 to May 2018. -
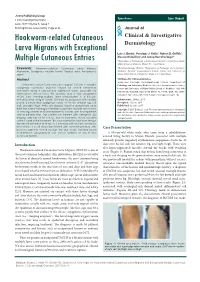
Hookworm-Related Cutaneous Larva Migrans with Exceptional Multiple Cutaneous Entries
Open Access Case Report J Clin Investigat Dermatol June 2017 Volume 5, Issue 1 © All rights are reserved by Vega et al. Journal of Hookworm-related Cutaneous Clinical & Investigative Larva Migrans with Exceptional Dermatology Luis J. Borda1, Penelope J. Kallis1, Robert D. Griffith1, Alessio Giubellino1 and Jeong Hee Cho-Vega2* Multiple Cutaneous Entries 1Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine, Miami, FL, United States Keywords: Hookworm-related Cutaneous Larva Migrans; 2Dermatopathology Division, Department of Pathology and Laboratory Hookworm; Serpiginous multiple tracks; Tropical area; Anti-parasite Medicine, Sylvester Comprehensive Cancer Center and University of agent Miami Miller School of Medicine, Miami, FL, United States Abstract *Address for Correspondence Jeong Hee Cho-Vega, Dermatopathology Division, Department of Hookworm-related Cutaneous Larva Migrans (HrCLM) is a pruritic Pathology and Laboratory Medicine Sylvester Comprehensive Cancer serpiginous cutaneous eruption caused by animal hookworms Center and University of Miami Miller School of Medicine 1120 NW commonly found in tropical and subtropical areas, especially the 14th Street, Holtz ET, Suite 2146 Miami, FL 33136, USA, Tel: (305)- Southeastern United States. We describe here a very exceptional 243-6433; Fax: (305)-243-1624; E-mail: [email protected] HrCLM case showing multiple larva entries/lesions in a 63-year- old white male living in Miami. Clinically he presented with multiple Submission: 25 May, 2017 pruritic erythematous serpiginous tracks on his left anterior leg, left Accepted: 15 June, 2017 calf, and right thigh. While skin biopsies failed to demonstrate larva Published: 22 June, 2017 itself, the overall histological features supported multiple larva tracks Copyright: © 2017 Borda LJ, et al. -

Co-Infection with Onchocerca Volvulus and Loa Loa Microfilariae in Central Cameroon: Are These Two Species Interacting?
843 Co-infection with Onchocerca volvulus and Loa loa microfilariae in central Cameroon: are these two species interacting? S. D. S. PION1,2*, P. CLARKE3, J. A. N. FILIPE2,J.KAMGNO1,J.GARDON1,4, M.-G. BASA´ N˜ EZ2 and M. BOUSSINESQ1,5 1 Laboratoire mixte IRD (Institut de Recherche pour le De´veloppement) – CPC (Centre Pasteur du Cameroun) d’Epide´miologie et de Sante´ publique, Centre Pasteur du Cameroun, BP 1274, Yaounde´, Cameroun 2 Department of Infectious Disease Epidemiology, St Mary’s campus, Norfolk Place, London W2 1PG, UK 3 Infectious Disease Epidemiology Unit London School of Hygiene and Tropical Medicine Keppel Street, London WC1E 7HT, UK 4 Institut de Recherche pour le De´veloppement, UR 24 Epide´miologie et Pre´vention, CP 9214 Obrajes, La Paz, Bolivia 5 Institut de Recherche pour le De´veloppement, De´partement Socie´te´s et Sante´, 213 rue La Fayette, 75480 Paris Cedex 10, France (Received 16 August 2005; revised 3 October; revised 9 December 2005; accepted 9 December 2005; first published online 10 February 2006) SUMMARY Ivermectin treatment may induce severe adverse reactions in some individuals heavily infected with Loa loa. This hampers the implementation of mass ivermectin treatment against onchocerciasis in areas where Onchocerca volvulus and L. loa are co-endemic. In order to identify factors, including co-infections, which may explain the presence of high L. loa micro- filaraemia in some individuals, we analysed data collected in 19 villages of central Cameroon. Two standardized skin snips and 30 ml of blood were obtained from each of 3190 participants and the microfilarial (mf) loads of both O.