Nobel Laureate for Medicine Prof. Bruce Beutler's Keynote Speech And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Unrestricted Immigration and the Foreign Dominance Of
Unrestricted Immigration and the Foreign Dominance of United States Nobel Prize Winners in Science: Irrefutable Data and Exemplary Family Narratives—Backup Data and Information Andrew A. Beveridge, Queens and Graduate Center CUNY and Social Explorer, Inc. Lynn Caporale, Strategic Scientific Advisor and Author The following slides were presented at the recent meeting of the American Association for the Advancement of Science. This project and paper is an outgrowth of that session, and will combine qualitative data on Nobel Prize Winners family histories along with analyses of the pattern of Nobel Winners. The first set of slides show some of the patterns so far found, and will be augmented for the formal paper. The second set of slides shows some examples of the Nobel families. The authors a developing a systematic data base of Nobel Winners (mainly US), their careers and their family histories. This turned out to be much more challenging than expected, since many winners do not emphasize their family origins in their own biographies or autobiographies or other commentary. Dr. Caporale has reached out to some laureates or their families to elicit that information. We plan to systematically compare the laureates to the population in the US at large, including immigrants and non‐immigrants at various periods. Outline of Presentation • A preliminary examination of the 609 Nobel Prize Winners, 291 of whom were at an American Institution when they received the Nobel in physics, chemistry or physiology and medicine • Will look at patterns of -

書 名 等 発行年 出版社 受賞年 備考 N1 Ueber Das Zustandekommen Der
書 名 等 発行年 出版社 受賞年 備考 Ueber das Zustandekommen der Diphtherie-immunitat und der Tetanus-Immunitat bei thieren / Emil Adolf N1 1890 Georg thieme 1901 von Behring N2 Diphtherie und tetanus immunitaet / Emil Adolf von Behring und Kitasato 19-- [Akitomo Matsuki] 1901 Malarial fever its cause, prevention and treatment containing full details for the use of travellers, University press of N3 1902 1902 sportsmen, soldiers, and residents in malarious places / by Ronald Ross liverpool Ueber die Anwendung von concentrirten chemischen Lichtstrahlen in der Medicin / von Prof. Dr. Niels N4 1899 F.C.W.Vogel 1903 Ryberg Finsen Mit 4 Abbildungen und 2 Tafeln Twenty-five years of objective study of the higher nervous activity (behaviour) of animals / Ivan N5 Petrovitch Pavlov ; translated and edited by W. Horsley Gantt ; with the collaboration of G. Volborth ; and c1928 International Publishing 1904 an introduction by Walter B. Cannon Conditioned reflexes : an investigation of the physiological activity of the cerebral cortex / by Ivan Oxford University N6 1927 1904 Petrovitch Pavlov ; translated and edited by G.V. Anrep Press N7 Die Ätiologie und die Bekämpfung der Tuberkulose / Robert Koch ; eingeleitet von M. Kirchner 1912 J.A.Barth 1905 N8 Neue Darstellung vom histologischen Bau des Centralnervensystems / von Santiago Ramón y Cajal 1893 Veit 1906 Traité des fiévres palustres : avec la description des microbes du paludisme / par Charles Louis Alphonse N9 1884 Octave Doin 1907 Laveran N10 Embryologie des Scorpions / von Ilya Ilyich Mechnikov 1870 Wilhelm Engelmann 1908 Immunität bei Infektionskrankheiten / Ilya Ilyich Mechnikov ; einzig autorisierte übersetzung von Julius N11 1902 Gustav Fischer 1908 Meyer Die experimentelle Chemotherapie der Spirillosen : Syphilis, Rückfallfieber, Hühnerspirillose, Frambösie / N12 1910 J.Springer 1908 von Paul Ehrlich und S. -

Table of Contents (PDF)
June 28, 2016 u vol. 113 u no. 26 From the Cover 7106 Topological defects in liquid crystals E3619 Translation control in Fragile X syndrome E3686 Voltage-sensing phosphatase activities E3782 Aerobic glycolysis and learning 7261 Electric field sensing by bumblebees Contents THIS WEEK IN PNAS Cover image: Pictured is a polarized 7003 In This Issue optical micrograph of a plastic sheet with an array of holes drilled into it and suspended in a nematic-phase liquid LETTERS (ONLINE ONLY) crystal. Lisa Tran et al. found that such a sheet induced arrays of topological E3590 Reduced nitrogen dominated nitrogen deposition in the United States, but its defect lines in a nematic liquid crystal. contribution to nitrogen deposition in China decreased The authors further demonstrated how Xuejun Liu, Wen Xu, Enzai Du, Yuepeng Pan, and Keith Goulding the energy of the liquid crystal and the E3592 Reply to Liu et al.: On the importance of US deposition of nitrogen dioxide, geometry of the holes affect the defect coarse particle nitrate, and organic nitrogen patterns. The findings might have Yi Li, Bret A. Schichtel, John T. Walker, Donna B. Schwede, Xi Chen, Christopher M. B. applications in electronic displays, Lehmann, Melissa A. Puchalski, David A. Gay, and Jeffrey L. Collett Jr. where nematic liquid crystals are widely used. See the article by Tran et al. on E3594 Rise and fall of nitrogen deposition in the United States pages 7106–7111. Image courtesy of Enzai Du Lisa Tran. E3596 Adult pelvic shape change is an evolutionary side effect Philipp Mitteroecker and Barbara Fischer E3597 Reply to Mitteroecker and Fischer: Developmental solutions to the obstetrical dilemma are not Gouldian spandrels Marcia S. -

Die Woche Spezial
In cooperation with DIE WOCHE SPEZIAL >> Autographs>vs.>#NobelSelfie Special >> Big>Data>–>not>a>big>deal,> Edition just>another>tool >> Why>Don’t>Grasshoppers> Catch>Colds? SCIENCE SUMMIT The>64th>Lindau>Nobel>Laureate>Meeting> devoted>to>Physiology>and>Medicine More than 600 young scientists came to Lindau to meet 37 Nobel laureates CAREER WONGSANIT > Women>to>Women: SUPHAKIT > / > Science>and>Family FOTOLIA INFLAMMATION The>Stress>of>Ageing > FLASHPICS > / > MEETINGS > FOTOLIA LAUREATE > CANCER RESEARCH NOBEL > LINDAU > / > J.>Michael>Bishop>and GÄRTNER > FLEMMING > JUAN > / the>Discovery>of>the>first> > CHRISTIAN FOTOLIA Human>Oncogene EDITORIAL IMPRESSUM Chefredakteur: Prof. Dr. Carsten Könneker (v.i.S.d.P.) Dear readers, Redaktionsleiter: Dr. Daniel Lingenhöhl Redaktion: Antje Findeklee, Jan Dönges, Dr. Jan Osterkamp where>else>can>aspiring>young>scientists> Ständige Mitarbeiter: Lars Fischer Art Director Digital: Marc Grove meet>the>best>researchers>of>the>world> Layout: Oliver Gabriel Schlussredaktion: Christina Meyberg (Ltg.), casually,>and>discuss>their>research,>or>their> Sigrid Spies, Katharina Werle Bildredaktion: Alice Krüßmann (Ltg.), Anke Lingg, Gabriela Rabe work>–>or>pressing>global>problems?>Or> Verlag: Spektrum der Wissenschaft Verlagsgesellschaft mbH, Slevogtstraße 3–5, 69126 Heidelberg, Tel. 06221 9126-600, simply>discuss>soccer?>Probably>the>best> Fax 06221 9126-751; Amtsgericht Mannheim, HRB 338114, UStd-Id-Nr. DE147514638 occasion>is>the>annual>Lindau>Nobel>Laure- Geschäftsleitung: Markus Bossle, Thomas Bleck Marketing und Vertrieb: Annette Baumbusch (Ltg.) Leser- und Bestellservice: Helga Emmerich, Sabine Häusser, ate>Meeting>in>the>lovely>Bavarian>town>of> Ute Park, Tel. 06221 9126-743, E-Mail: [email protected] Lindau>on>Lake>Constance. Die Spektrum der Wissenschaft Verlagsgesellschaft mbH ist Kooperati- onspartner des Nationalen Instituts für Wissenschaftskommunikation Daniel>Lingenhöhl> GmbH (NaWik). -

Aaron Ciechanover 2004 Nobel Laureate in Chemistry
TRINITY COLLEGE DUBLIN Medical Research at the Cutting Edge Progress in the fight against Inflammatory Diseases and Cancer Joint Symposium of the Trinity Biomedical Sciences Institute and The Weizmann Institute of Science Tercentenary Hall, Trinity Biomedical Sciences Institute Keynote Speakers July 27-29, 2014 Bruce Beutler 2011 Nobel Laureate in Speakers Physiology and Medicine Opening Address Minister Sean Sherlock TD, University of Texas Minister for Research and Innovation, Irish Government. Aaron Ciechanover Ireland Israel 2004 Nobel Laureate in Chemistry Luke O’Neill Ruth Arnon Technion Israel Institute of TBSI Academic Director The President of the Israel Academy of Technology Diarmuid O’Brien Sciences and Humanities Director of Trinity Research and Mudi Sheves Marc Feldmann Innovation The Weizmann Institute of Science 2003 Albert Lasker Award Andrew Bowie Vice President for Technology Transfer for Clinical Medical Research Trinity Biomedical Sciences Inst. Ido Amit University of Oxford Paul Brown Weizmann Institute of Science England Trinity College Dublin Yinon Ben-Neriah Martin Caffrey Hebrew Univ. of Jerusalem Jules Hoffmann Trinity Biomedical Sciences Inst. 2011 Nobel Laureate in Ashraf Brik Gavin Davey Physiology and Medicine Ben Gurion University Trinity Biomedical Sciences Inst. Institut de Biologie Moleculaire Steffen Jung et Cellulaire, France Aisling Dunne Trinity Biomedical Sciences Inst. Weizmann Institute of Science James Watson Padraic Fallon Eran Elinav 1962 Nobel Laureate in Trinity Biomedical Sciences Inst. Weizmann Institute of Science Physiology and Medicine Alan Irvine Yehuda Kamari Cold Spring Harbor Laboratory Trinity College Dublin Sheba Medical Center New York Vincent Kelly Irit Sagi Trinity Biomedical Sciences Inst. Weizmann Institute of Science Ada Yonath Seamus Martin Idit Shachar 2009 Nobel Laureate in Trinity College Dublin Weizmann Institute of Science Chemistry Kingston Mills David Wallach Weizmann Institute of Science, Trinity Biomedical Sciences Inst. -

Nobel Endeavors in Immunology Introducing Dr
SPRING 2012 A PUBLICATION OF SOUTHWESTERN MEDICAL FOUNDATION Nobel Endeavors in Immunology Introducing Dr. Bruce Beutler, UT Southwestern’s fifth Nobel Laureate, and the new Center for the Genetics of Host Defense Southwestern Medical Foundation Board of Trustees 2011-2012 Edward M. Ackerman Joe M. Haggar, III Richard R. Pollock Sara Melnick Albert Nancy S. Halbreich Caren H. Prothro The Heritage Society Rafael M. Anchia LaQuita C. Hall Carolyn Perot Rathjen OF SOUTHWESTERN MEDICAL FOUNDATION Table of Contents Charlotte Jones Anderson Paul W. Harris* Mike Rawlings table of contents Barry G. Andrews Linda W. Hart Jean W. Roach Joyce T. Alban Mr. and Mrs. Thomas E. McCullough Marilyn H. Augur Joe V. (Jody) Hawn, Jr. Linda Robuck Mr. and Mrs. James R. Alexander Christopher F. McGratty Robert D. Rogers Ralph W. Babb, Jr. Jess T. Hay Anonymous (11) Carmen Crews McCracken McMillan Editor Doris L. Bass Frederick B. Hegi, Jr. Catherine M. Rose George A. Atnip# Ferd C. and Carole W. Meyer Nobel Endeavors in Immunology Peter Beck Jeffrey M. Heller* Billy Rosenthal Marilyn Augur* William R. and Anne E. Montgomery Heidi Harris Cannella The threads of Dr. Bruce Beutler’s scientific 3 # Jill C. Bee Julie K. Hersh Lizzie Horchow Routman* Paul M. Bass* Kay Y. Moran career are inextricably woven into the fabric of W. Robert Beavers, M.D. Barbara and Robert Munford Gil J. Besing Thomas O. Hicks Robert B. Rowling* Creative Director UT Southwestern’s history. From intern to mid-career Drs. Paul R. and Robert H. Munger# Jan Hart Black Sally S. Hoglund Stephen H. -

Winter 2008/2009
WINTER 2008/09 VOLUME ELEVEN / NUMBER THREE NON-PROFIT U.S. POSTAGE PAID PERMIT 751 SAN DIEGO, CA A PUBLICATION OF THE SCRIPPS RESEARCH INSTITUTE Office of Communications—TPC30 10550 North Torrey Pines Road La Jolla, California 92037 www.scripps.edu PUBLISHER: Keith McKeown EDITOR: Mika Ono DESIGN: Studio 32 North PRODUCTION: Studio 32 North Kevin Fung COVER ILLUSTRATION: Brian Rea INTERIOR ILLUSTRATIONS: Meg Mateo Ilasco PORTRAIT PHOTOGRAPHY: Dana Neibert PRINTING: Precision Litho Copyright © 2008. Published by TSRI Press™ “I benefited tremendously from the truly interdisciplinary nature of the Skaggs Institute.” THE SCRIPPS RESEARCH INSTITUTE EXPERTS IN ALMOST JIANMIN GAO, Ph.D. EVERY SUBFIELD JIANMIN GAO, Ph.D. (top) Jianmin Gao, Ph.D., now an assistant professor of chem- exchange ideas, which greatly broadens the horizon of PER HAMMARSTROM, istry at Boston College, served as a postdoctoral fellow scientific problems one dares to tackle.” Ph.D. at the Skaggs Institute under Jeffery Kelly, Ph.D., chair At Boston College, Gao is working on protein folding (bottom) VOLUME ELEVEN / NUMBER THREE WINTER 2008/09 of the Department of Molecular and Experimental Medi- and aggregation, specifically on the folding mechanisms cine and Lita Annenberg Hazen Professor of Chemistry. of beta-structured membrane proteins, which play vital Kelly is also chair of the Board of Trustees of the Skaggs roles in cancer biology. Gao strives to use chemical tools Institute for Research, one of the Skaggs family’s major to bring a fresh look at biological problems. mechanisms for its philanthropy. Understanding the chemistry and biology of mem- 41 “I benefited tremendously from the truly interdisci- brane protein folding is a substantial challenge, and plinary nature of the Skaggs Institute,” said Gao. -

Salk Bulletin, January 28 - February 4, 2019 Date: Friday, January 25, 2019 2:34:00 PM
From: Bulletin To: "[email protected]" Subject: Salk Bulletin, January 28 - February 4, 2019 Date: Friday, January 25, 2019 2:34:00 PM Salk Bulletin Monday, January 28, 2019 Monday, January 28, 2019 4:00 pm – 5:00 pm "Evasion of IL-22-Mediated Antimicrobial Responses by Bacterial Pathogens" Manuela Raffatellu, M.D., Professor, Department of Pediatrics, Division of Host-Microbe Systems and Therapeutics UNIVERSITY OF CALIFORNIA SAN DIEGO Leichtag Room 107 Host: Nissi Varki, M.D. Contact: Andrea Bribiesca, [email protected] Tuesday, January 29, 2019 Tuesday, January 29, 2019 12:00 pm "Circadian Rhythms and Gene Expression Regulation in Different Neurons or Cell Types" Michael Rosbash, Ph.D., Peter Gruber Professor of Neuroscience, Investigator, Howard Hughes Medical Institute; Professor, Department of Biology, Brandeis University President’s Lecture Series SANFORD BURNHAM PREBYS MEDICAL DISCOVERY INSTITUTE Fishman Auditorium Host: Rolf Bodmer Contact: Wendy Lyon, [email protected] Tuesday, January 29, 2019 12:00 pm “GPCR Signaling Pathways as Critical Regulators of Body Weight and Glucose Homeostasis: Clinical Implications” Jürgen Wess, Ph.D., Chief, Molecular Signaling Section, Laboratory of Bioorganic Chemistry, National Institute of Diabetes and Digestive and Kidney Diseases UNIVERSITY OF CALIFORNIA SAN DIEGO Leichtag Building, Room 107 Host: Joan Heller Brown Tuesday, January 29, 2019 3:00 pm “Drugging ‘the Undruggable’. The Augmented Reality of Emerging Therapeutics” Artem Cherkasov, Ph.D., Professor, Faculty of Medicine, University of British Columbia; Head, Therapeutics Development Core Vancouver Prostate Centre SANFORD BURNHAM PREBYS MEDICAL DISCOVERY INSTITUTE Fishman Auditorium Host: Ze’ev Ronai Contact: [email protected] Tuesday, January 29, 2019 4:00 pm “Understanding Sensorimotor Integration During Odor-guided Behaviors” Dinu Florin Albeanu, Cold Spring Harbor Laboratory Neurosciences Seminar Series UNIVERSITY OF CALIFORNIA SAN DIEGO CNCB Marilyn G. -

Guest Editorial 1 Guest Editorial
Indian JJ PhysiolPhysiol PharmacolPharmacol 2012; 2012; 56(1) 56(1) : 1–6 Guest Editorial 1 Guest Editorial IMMUNOLOGY AND NOBEL PRIZE : A LOVE STORY Several breakthroughs revealing the way in which our bodies protect us against microscopic threats of almost any description have been duly acknowledged by the Nobel Prizes in Physiology or Medicine. Interestingly, Nobel Prizes in Physiology or Medicine including the latest one, for the year 2011, has been awarded for twelve times to the field of Immunology. The story began in 1901 with the very first Nobel Prize in Physiology or Medicine - it was awarded to Emil Von Behring for his pioneering work which resulted in the discovery of antitoxins, later termed as antibodies. Working with Shibasaburo Kitasato, Von Behring found that when animals were injected with tiny doses of weakened forms of tetanus or diphtheria bacteria, their blood extracts contained chemicals released in response, which rendered the pathogens’ toxins harmless. Naming these chemical agents ‘antitoxins’, Von Behring and Erich Wernicke showed that transferring antitoxin-containing blood serum into animals infected with the fully virulent versions of diphtheria bacteria cured the recipients of any symptoms, and prevented death. This was found to be true for humans also; and thus Von Behring’s method of treatment – passive serum therapy – became an essential remedy for diphtheria, saving many thousands of lives every year. Shortly after this, the very first explanation about the mechanisms of immune system’s functioning was proposed which paved way for extensive research in immunology till today. Paul Ehrlich had hit upon the key concept of how antibodies seek and neutralize the toxic actions of bacteria, while Ilya Mechnikov had discovered that certain body cells could destroy pathogens by simply engulfing or “eating” them. -

CV Bruce Beutler
Curriculum Vitae Prof. Dr. Bruce Beutler Name: Bruce Alan Beutler Born: 29 December 1957 Research focuses: Immune system, innate immunity, receptor proteins, toll gene, toll‐like receptors (TLR), tumour necrosis factor (TNF), TNF blockers Bruce Alan Beutler is an American immunologist and geneticist. In 2011 he was awarded the Nobel Prize in Physiology or Medicine along with Jules Hoffmann and Ralph M. Steinmann. The three scientists researched the human immune system and, as the Nobel committee put it, “revolutionised our understanding of the immune system”. Bruce Beutler and his colleague Jules Hoffmann discovered activation mechanisms of innate immunity. Academic and Professional Career since 2011 Director of the Center for the Genetics of Host Defense and holder of the “Raymond and Ellen Willie Distinguished Chair in Cancer Research”, University of Texas Southwestern Medical Center, USA 2007 ‐ 2011 Chief of the Department of Genetics, The Scripps Research Institute, La Jolla, USA 2000 ‐ 2007 Professor of Immunology and Microbial Science (IMS), The Scripps Research Institute, La Jolla, USA 2000 ‐ 2011 Lecturer, Kellogg School of Science and Technology, The Scripps Research Institute, La Jolla, USA 1996 ‐ 2000 Professor at the University of Texas Southwestern Medical Center, USA 1991 ‐ 2000 Associate Scientist at the University of Texas Southwestern Medical Center, USA 1990 ‐ 1996 Associate Professor, Department of Internal Medicine, University of Texas Southwestern Medical Center, USA Nationale Akademie der Wissenschaften Leopoldina www.leopoldina.org 1 1986 ‐ 1991 Assistant Investigator, Howard Hughes Medical Institute, USA 1986 ‐ 1990 Assistant Professor, Department of Internal Medicine, The University of Texas Southwestern Medical Center, USA 1985 ‐ 1986 Assistant Professor, Rockefeller University, USA 1983 ‐ 1985 Postdoctoral Fellow, Rockefeller University, USA 1981 ‐ 1983 Assistant, University of Texas Southwestern Medical Center, USA 1981 M.D., Pritzker School of Medicine, University of Chicago, USA 1976 B.A. -

BIOVISION 2013 Speakers Oct 24 GB
BRINGING TOGETHER MULTI-STAKEHOLDER PARTNERS TO TRANSLATE SCIENTIFIC ADVANCES INTO ACTIONABLE SOLUTIONS FOR THE BENEFIT OF CITIZENS BIOVISION SPEAKERS BIOVISION, the World Life Sciences Forum , brings together international decision makers from the academic, private sector, policy-making and civil society sectors to debate over the impact of the latest scientific advances on society. 2013 SPEAKERS* • Geneviève Fioraso (Minister for Higher Education and Research, France) • Marisol Touraine (Minister of Health and Social Affairs, France) • Awa-Marie Coll-Seck ( Health Minister, Senegal) • Carlos Gadelha (Secretary of State, Ministry of Health, Brazil) • Grace Naledi Mandisa Pandor (Minister of Science and Technology, Republic of South Africa) • Michele Bachelet (Former President, Republic of Chile; Executive Director, UN WOMEN) • Anne Glover (Chief Scientific Adviser to the President, European Commission) – Confirmed • Paul Rübig (President STOA, member of European Parliament) • Antonio Fernando Correia de Campos (Vice President, STOA, European Parliament) • John Beddington (Scientific Adviser, United Kingdom Government) • Oleg Chestnov (Assistant Director General, Non Communicable Diseases and Mental Health, WHO, Switzerland) • Kris Christen (Editor and writer, Artificial Retina Project, U.S. Department of Energy) • Gerald Dziekan (Head Safe Surgery, Pulse Oximetry, Care Checklists & AMR Programmes, HO Patient Safety, Switzerland) – Confirmed • Carissa F. Etienne (Assistant Director General, Health Systems and Services, WHO, Switzerland) -
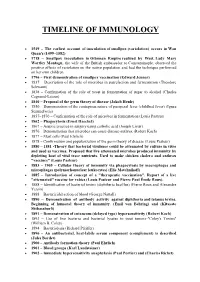
Timeline of Immunology
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins.