Estimation of the Collective Effective Dose to the Population from Medical X-Ray Examinations in Finland
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RADIOGRAPHY to Prepare Individuals to Become Registered Radiologic Technologists
RADIOGRAPHY To prepare individuals to become Registered Radiologic Technologists. THE WORKFORCE CAPITAL This two-year, advanced medical program trains students in radiography. Radiography uses radiation to produce images of tissues, organs, bones and vessels of the body. The radiographer is an essential member of the health care team who works in a variety of settings. Responsibili- ties include accurately positioning the patient, producing quality diagnostic images, maintaining equipment and keeping computerized records. This certificate program of specialized training focuses on each of these responsibilities. Graduates are eligible to apply for the national credential examination to become a registered technologist in radiography, RT(R). Contact Student Services for current tuition rates and enrollment information. 580.242.2750 Mission, Goals, and Student Learning Outcomes Program Effectiveness Data Radiography Program Guidelines (Policies and Procedures) “The programs at Autry prepare you for the workforce with no extra training needed after graduation.” – Kenedy S. autrytech.edu ENDLESS POSSIBILITIES 1201 West Willow | Enid, Oklahoma, 73703 | 580.242.2750 | autrytech.edu COURSE LENGTH Twenty-four-month daytime program î August-July î Monday-Friday Academic hours: 8:15am-3:45pm Clinical hours: Eight-hour shifts between 7am-5pm with some ADMISSION PROCEDURES evening assignments required Applicants should contact Student Services at Autry Technology Center to request an information/application packet. Applicants who have a completed application on file and who have met entrance requirements will be considered for the program. Meeting ADULT IN-DISTRICT COSTS the requirements does not guarantee admission to the program. Qualified applicants will be contacted for an interview, and class Year One: $2732 (Additional cost of books and supplies approx: $1820) selection will be determined by the admissions committee. -

ACR–SPR-STR Practice Parameter for the Performance of Chest Radiography
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2017 (Resolution 2)* ACR–SPR–STR PRACTICE PARAMETER FOR THE PERFORMANCE OF CHEST RADIOGRAPHY PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -
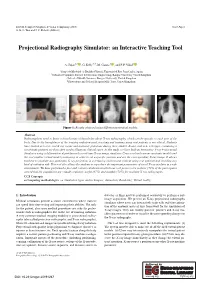
Projectional Radiography Simulator: an Interactive Teaching Tool
EG UK Computer Graphics & Visual Computing (2019) Short Paper G. K. L. Tam and J. C. Roberts (Editors) Projectional Radiography Simulator: an Interactive Teaching Tool A. Sujar1,2 , G. Kelly3,4, M. García1 , and F. P. Vidal2 1Grupo de Modelado y Realidad Virtual, Universidad Rey Juan Carlos, Spain 2School of Computer Science & Electronic Engineering, Bangor University United Kingdom 3School of Health Sciences, Bangor University, United Kingdom 4Shrewsbury and Telford Hospital NHS Trust, United Kingdom Figure 1: Results obtained using different anatomical models. Abstract Radiographers need to know a broad range of knowledge about X-ray radiography, which can be specific to each part of the body. Due to the harmfulness of the ionising radiation used, teaching and training using real patients is not ethical. Students have limited access to real X-ray rooms and anatomic phantoms during their studies. Books, and now web apps, containing a set of static pictures are then often used to illustrate clinical cases. In this study, we have built an Interactive X-ray Projectional Simulator using a deformation algorithm with a real-time X-ray image simulator. Users can load various anatomic models and the tool enables virtual model positioning in order to set a specific position and see the corresponding X-ray image. It allows teachers to simulate any particular X-ray projection in a lecturing environment without using real patients and avoiding any kind of radiation risk. This tool also allows the students to reproduce the important parameters of a real X-ray machine in a safe environment. We have performed a face and content validation in which our tool proves to be realistic (72% of the participants agreed that the simulations are visually realistic), useful (67%) and suitable (78%) for teaching X-ray radiography. -

THE COLLECTIVE EFFECTIVE DOSE RESULTING from RADIATION EMITTED DURING the FIRST WEEKS of the FUKUSHIMA DAIICHI NUCLEAR ACCIDENT Matthew Mckinzie, Ph.D
THE COLLECTIVE EFFECTIVE DOSE RESULTING FROM RADIATION EMITTED DURING THE FIRST WEEKS OF THE FUKUSHIMA DAIICHI NUCLEAR ACCIDENT Matthew McKinzie, Ph.D. and Thomas B. Cochran, Ph.D., Natural Resources Defense Council April 10, 2011 The Magnitude 9.0 earthquake off Japan’s Pacific Coast, which was the initiating event for accidents at four of the six reactors at the Fukushima Daiichi nuclear power plant, occurred at 14:46 local time on March 11th. At 15:41 a tsunami hit the plant and a station blackout ensued. A reconstruction of the accident progression by Areva1 posited that the final option for cooling the reactors – the reactor core isolation pumps – failed just hours later in Unit 1 (at 16:36), failed in the early morning of March 13th in Unit 3 (at 02:44), and failed early in the afternoon of March 14th in Unit 2 (at 13:25). Radiological releases spiked beginning on March 15th and in the Areva analysis are attributed to the venting of the reactor pressure vessels, explosion in Unit 2, and – significantly – explosion and fire in Unit 4. Fuel had been discharged from the Unit 4 reactor core to the adjacent spent fuel pool on November 30, 2010, raising the possibility of a core melt “on fresh air.” The Japanese Ministry of Education, Culture, Sports, Science and Technology (MEXT) has posted hourly dose rates by prefecture2 on its website. We do not currently know the geographic coordinates of these radiation monitoring sites. The English language versions of the hourly dose rate measurements by prefecture begin in table form at 17:00 on March 16th, and hourly dose rates are provided as charts3 beginning at 00:00 on March 14th. -

Download Article (PDF)
Current Directions in Biomedical Engineering 2015; 1:257–260 Thomas Homann*, Axel Boese, Sylvia Glaßer, Martin Skalej, and Oliver Beuing Intravascular optical coherence tomography (OCT) as an additional tool for the assessment of stent structures Abstract: Evaluation of the vascular stent position, shape cases an additional imaging of the implants by OCT would and correct expansion has a high relevance in therapy be benecial. In our study, we determined the ability of and diagnosis. Hence, the wall apposition in vessel areas OCT to image structural information of dierent vascular with diering diameters and the appearance of torsions or stents in a phantom study. structural defects of the implant body caused by catheter based device dropping are of special interest. Neurovascu- lar implants like braided ow diverter and laser cut stents 2 Materials and methods consist of metal struts and wires with diameters of about 40 µm. Depending on the implants material composition, A plastic model with bores of dierent diameters for the in- visibility is poor with conventional 2D X-ray uoroscopic take of 3 vascular implants was manufactured (see Figure and radiographic imaging. The metal structures of the im- 1). The model has a geometrical extend of 80 mm×50 mm× plants also lead to artifacts in 3D X-ray images and can 15 mm and a straight course of the bores. A translucent hamper the assessment of the device position. We inves- plastic material was selected for a low absorption of near tigated intravascular optical coherence tomography (OCT) infrared light generated by the OCT system. Objects of in- as a new imaging tool for the evaluation of the vascular vestigation were 3 vascular stents with dierent geometri- stent position, its shape and its correct expansion for 3 dif- cal and structural properties (see Table 1). -
Individual and Collective Dose Limits and Radionuclide Release Limits
UNITED STATES NUCLEAR REGULATORY COMMISSION ADVISORY COMMITTEE ON NUCLEAR WASTE WASHINGTON, D.C. 20555 April 29, 1991 r' Mr. Robert M. Bernero, Director Office of Nuclear Material Safety and Safeguards u.s. Nuclear Regulatory Commission Washington, DC 20555 Dear Mr. Bernero: SUBJECT: INDIVIDUAL AND COLLECTIVE DOSE LIMITS AND RADIONUCLIDE RELEASE LIMITS The Advisory Committee . on Nuclear waste has been developing comments, thoughts, and suggestions relative to individual and collective dose limits and radionuclide release limits. Since we understand that your staff is reviewing these same topics, we wanted to share our thoughts with you. In formulating these comments, we have had discussions with a number of people, including members of the NRC staff and Committee consultants. The Committee also had the benefit of the documents listed. Basic Definitions As a basic philosophy, individual dose limits are used to place restrictions on the risk to individual members of the public due to operations at a nuclear facility. If the limits have been properly established and compliance is observed, a regulatory agency can be confident that the associated risk to individual members of the pUblic is acceptable. Because the determination of the dose to individual members of the pUblic is difficult, the International Commission on Radiological Protection (ICRP) has developed the concept of the "critical group" and recommends that it be used in assessing doses resulting from environmental releases. As defined by the ICRP, a critical group is a relatively homogeneous group of people whose location and living habits are such that they receive the highest doses as a result of radio nuclide releases. -

X-Ray (Radiography) - Bone Bone X-Ray Uses a Very Small Dose of Ionizing Radiation to Produce Pictures of Any Bone in the Body
X-ray (Radiography) - Bone Bone x-ray uses a very small dose of ionizing radiation to produce pictures of any bone in the body. It is commonly used to diagnose fractured bones or joint dislocation. Bone x-rays are the fastest and easiest way for your doctor to view and assess bone fractures, injuries and joint abnormalities. This exam requires little to no special preparation. Tell your doctor and the technologist if there is any possibility you are pregnant. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. What is Bone X-ray (Radiography)? An x-ray exam helps doctors diagnose and treat medical conditions. It exposes you to a small dose of ionizing radiation to produce pictures of the inside of the body. X-rays are the oldest and most often used form of medical imaging. A bone x-ray makes images of any bone in the body, including the hand, wrist, arm, elbow, shoulder, spine, pelvis, hip, thigh, knee, leg (shin), ankle or foot. What are some common uses of the procedure? A bone x-ray is used to: diagnose fractured bones or joint dislocation. demonstrate proper alignment and stabilization of bony fragments following treatment of a fracture. guide orthopedic surgery, such as spine repair/fusion, joint replacement and fracture reductions. look for injury, infection, arthritis, abnormal bone growths and bony changes seen in metabolic conditions. assist in the detection and diagnosis of bone cancer. locate foreign objects in soft tissues around or in bones. How should I prepare? Most bone x-rays require no special preparation. -

The ASRT Practice Standards for Medical Imaging and Radiation Therapy
The ASRT Practice Standards for Medical Imaging and Radiation Therapy Sonography ©2019 American Society of Radiologic Technologists. All rights reserved. Reprinting all or part of this document is prohibited without advance written permission of the ASRT. Send reprint requests to the ASRT Publications Department, 15000 Central Ave. SE, Albuquerque, NM 87123-3909. Effective June 23, 2019 Table of Contents Preface .......................................................................................................................................................... 1 Format ....................................................................................................................................................... 1 Introduction .................................................................................................................................................. 3 Definition .................................................................................................................................................. 3 Education and Certification ...................................................................................................................... 5 Medical Imaging and Radiation Therapy Scope of Practice .......................................................................... 6 Standards ...................................................................................................................................................... 8 Standard One – Assessment .................................................................................................................... -

Radiography Program
Radiography Program Program Description The Radiography (X-ray) Program at Tulsa Community College is designed to prepare students with the knowledge and skills to function as medical radiographers. The program is nationally accredited by the Joint Review Committee on Education in Radiologic Technology. Medical Radiographers/Radiologic Technologists are the medical personnel who perform diagnostic imaging examinations. Radiographers use x-rays to produce black and white images of anatomy. These images are captured on film, computer or videotape. Radiographers are educated in anatomy, patient positioning, examination techniques, equipment protocols, radiation safety, radiation protection and basic patient care. Radiographers often specialize in areas of CT, MRI, Mammography, Cardiovascular Technology, Quality Control, Management and Education. Radiographers work closely with radiologists, physicians who interpret medical images to either diagnose or rule out disease or injury. Program Information Degree Awarded: Associate Degree in Applied Science The Radiography (X-ray) Program admits a new class each year beginning in June (summer term). The number of students admitted to the class is determined by the number of clinical training sites available to place students, which is usually between 30-35 students. Radiography is a two-year (six-semester) program consisting of 48 credit hours of Radiography courses (didactic and clinical) and 22 hours of related general education courses. Lecture and clinical courses run concurrently throughout the two years. Upon completion of the program, graduates receive an Associate in Applied Science (AAS) degree, and are eligible to apply for examination by the American Registry of Radiologic Technologists (ARRT) in Radiography (R). Clinical education classes consist of eight-hour shifts for two to three days per week in the assigned clinical education center. -

THE TERMOGRAPHIC ANALYSIS of the WELDING by TIG M.Sc., Eng
SCIENTIFIC PROCEEDINGS XI INTERNATIONAL CONGRESS "MACHINES, TECHNOLОGIES, MATERIALS" 2014 ISSN 1310-3946 THE TERMOGRAPHIC ANALYSIS OF THE WELDING BY TIG M.Sc., Eng. Maś K., M.Sc. Woźny M., PhD. Marchewka M. , PhD. Płoch D. and Prof. Dr.Sheregii E.M. Centre for Microelectronics and Nanotechnology, University of Rzeszow, Poland [email protected] Abstract: Thermography measurements allow to detect the defects that may appear on a joint at welding of components. Energy pulse generated by a xenon lamp with adequate power in a short period of time is sufficient for thermal excitation and enables to register the temperature distribution using the thermography high resolution camera FLIR SC7000. The impulse with 6kJ energy and 6ms time generate sufficient power to measure the temperature distribution on the surface of the weld tested. During cooling the temperature of the area with defect changes more slowly than in the areas without defects, because of to the less intense heat dissipation. This allows the registration of defects in welds "on-line" at the production process. Material used for analysis detection of defects in the welded joints is Inconel 718, stainless steel 410 and stainless steel 321. The peak energy which flow throw the samples with defects in the welded joints its completely or partially blocked. It cause different temperature distribution on the surface in the places where the connection discontinuity take place. Keywords: THERMOGRAPHY, DEFECTS, WELDING, NDT 1. Introduction therefore, X-rays and gamma rays can be used to show discontinuities and inclusions within the opaque material. The Welded joints and padding layers are subjected to control permanent film record of the internal conditions will show the basic processes through the use of non-destructive testing methods to information by which the weld reliability and credibility could be ensure a high quality semi-finished and finished products [1-3]. -

Interim Guidelines for Hospital Response to Mass Casualties from a Radiological Incident December 2003
Interim Guidelines for Hospital Response to Mass Casualties from a Radiological Incident December 2003 Prepared by James M. Smith, Ph.D. Marie A. Spano, M.S. Division of Environmental Hazards and Health Effects, National Center for Environmental Health Summary On September 11, 2001, U.S. symbols of economic growth and military prowess were attacked and thousands of innocent lives were lost. These tragic events exposed our nation’s vulnerability to attack and heightened our awareness of potential threats. Further examination of the capabilities of foreign nations indicate that terrorist groups worldwide have access to information on the development of radiological weapons and the potential to acquire the raw materials necessary to build such weapons. The looming threat of attack has highlighted the vital role that public health agencies play in our nation’s response to terrorist incidents. Such agencies are responsible for detecting what agent was used (chemical, biological, radiological), event surveillance, distribution of necessary medical supplies, assistance with emergency medical response, and treatment guidance. In the event of a terrorist attack involving nuclear or radiological agents, it is one of CDC’s missions to insure that our nation is well prepared to respond. In an effort to fulfill this goal, CDC, in collaboration with representatives of local and state health and radiation protection departments and many medical and radiological professional organizations, has identified practical strategies that hospitals can refer -

Diagnostic Radiology Physics Diagnostic This Publication Provides a Comprehensive Review of Topics Relevant to Diagnostic Radiology Physics
A Handbook for Teachers and Students A Handbook for Teachers Diagnostic Diagnostic This publication provides a comprehensive review of topics relevant to diagnostic radiology physics. It is intended to provide the basis for the education of medical physicists in the field of diagnostic radiology. Bringing together the work of 41 authors and reviewers from 12 countries, the handbook covers a broad range of topics including radiation physics, dosimetry and Radiology instrumentation, image quality and image perception, imaging modality specific topics, recent advances in digital techniques, and radiation biology and protection. It is not designed to replace the large number of textbooks available on many aspects of diagnostic radiology physics, but is expected Radiology Physics Physics to fill a gap in the teaching material for medical radiation physics in imaging, providing in a single manageable volume the broadest coverage of topics currently available. The handbook has been endorsed by several international professional bodies and will be of value to those preparing for their certification A Handbook for as medical physicists, radiologists and diagnostic radiographers. Teachers and Students D.R. Dance S. Christofides A.D.A. Maidment I.D. McLean K.H. Ng Technical Editors International Atomic Energy Agency Vienna ISBN 978–92–0–131010–1 1 @ DIAGNOSTIC RADIOLOGY PHYSICS: A HANDBOOK FOR TEACHERS AND STUDENTS The following States are Members of the International Atomic Energy Agency: AFGHANISTAN GHANA OMAN ALBANIA GREECE PAKISTAN ALGERIA GUATEMALA