X-Ray (Radiography) - Bone Bone X-Ray Uses a Very Small Dose of Ionizing Radiation to Produce Pictures of Any Bone in the Body
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chest X-Rays | | How to Prepare and What to Expect |
UW MEDICINE | PATIENT EDUCATION | Chest X-rays | | How to prepare and what to expect | This handout explains how chest X-rays work, how to prepare, what to expect, and how to get your results. What is a chest X-ray? An X-ray (radiology exam) is a medical test that produces images (pictures) of a part of a body. These images help doctors diagnose health conditions. Doctors use chest X-rays to assess the lungs, heart, and chest wall. This exam can help diagnose pneumonia, heart failure, emphysema, lung cancer, and other medical problems. How does the exam work? An X-ray machine is like a camera. But, it uses X-rays instead of light to create images. When the machine is turned on, X-rays pass through the part of the body that is being studied. Your doctor will view the X-ray images on a computer screen. How do I prepare? • You do not need to prepare in any special way for chest X-rays. • Women: Tell your doctor or X-ray technologist if there is any chance that you may be pregnant. How is the exam done? • First, we will ask you to: – Change into a hospital gown – Remove jewelry, glasses, Talk with your referring provider about and any metal objects the results of your chest X-ray exam. that could show up on the pictures _____________________________________________________________________________________________ Page 1 of 2 | Chest X-rays UWMC Imaging Services | Box 357115 1959 N.E. Pacific St., Seattle, WA 98195 | 206.598.6200 • For most chest X-rays, you will stand with your chest pressed to the X-ray machine, with your hands on your hips and your shoulders pushed forward. -
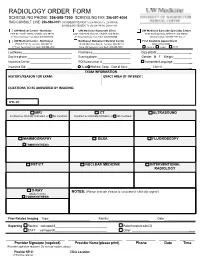
Radiology Order Form
RADIOLOGY ORDER FORM SCHEDULING PHONE: 206-598-7200 SCHEDULING FAX: 206-597-4004 RAD CONSULT LINE: 206-598-0101 UW RADIOLOGY RECORDS: Tel: 206-598-6206 Fax: 206-598-7690 NW RADIOLOGY RECORDS: Tel: 206-668-1748 Fax: 206-688-1398 UW Medical Center - Montlake UW Medicine Roosevelt Clinic UW Medicine Eastside Specialty Center 1959 NE Pacific Street, Seattle, WA 98195 4245 Roosevelt Way NE, Seattle, WA 98105 3100 Northup Way, Bellevue, WA 98004 2nd Floor Radiology Front Desk: 206-598-6200 2nd Floor Radiology Front Desk: 206-598-6868 ESC Front Desk: 425-646-7777 Opt. 2 UW Medical Center - Northwest Northwest Outpatient Medical Center First Available Appointment 1550 N 115th St, Seattle, WA 98133 10330 Meridian Ave N, Seattle, WA 98133 (ANY LOCATION) 2nd Floor Radiology Front Desk: 206-668-1302 Suite 130 Radiology Front Desk: 206-668-6050 Routine Urgent STAT Last Name: First Name: Date of Birth: _ Daytime phone: Evening phone: Gender: M F Weight:___________ Insurance Carrier: RQI/Authorization #: Interpreter/Language: __ Insurance ID#: Auto Workers’ Comp Date of Injury: ______ Claim # __ EXAM INFORMATION HISTORY/REASON FOR EXAM: EXACT AREA OF INTEREST: EXAM INFORMATION QUESTIONS TO BE ANSWERED BY IMAGING: ICD-10: MRI CT ULTRASOUND Contrast as clinically indicated, or No Contrast Contrast as clinically indicated, or No Contrast MAMMOGRAPHY DEXA FLUOROSCOPY TOMOSYNTHESIS PET/CT NUCLEAR MEDICINE INTERVENTIONAL RADIOLOGY X-RAY NOTES: (Please indicate if exam is considered “clinically urgent”) (Walk-In Only) TOMOSYNTHESIS Prior Related Imaging Type:_________________________ Facility:_________________________ Date:___________________ Reporting Routine call report # Patient to return with CD STAT call report # Other: __________ ________________________ ______________________ ____________ _______ ______ Provider Signature (required) Provider Name (please print) Phone Date Time (Provider signature required. -

RADIOGRAPHY to Prepare Individuals to Become Registered Radiologic Technologists
RADIOGRAPHY To prepare individuals to become Registered Radiologic Technologists. THE WORKFORCE CAPITAL This two-year, advanced medical program trains students in radiography. Radiography uses radiation to produce images of tissues, organs, bones and vessels of the body. The radiographer is an essential member of the health care team who works in a variety of settings. Responsibili- ties include accurately positioning the patient, producing quality diagnostic images, maintaining equipment and keeping computerized records. This certificate program of specialized training focuses on each of these responsibilities. Graduates are eligible to apply for the national credential examination to become a registered technologist in radiography, RT(R). Contact Student Services for current tuition rates and enrollment information. 580.242.2750 Mission, Goals, and Student Learning Outcomes Program Effectiveness Data Radiography Program Guidelines (Policies and Procedures) “The programs at Autry prepare you for the workforce with no extra training needed after graduation.” – Kenedy S. autrytech.edu ENDLESS POSSIBILITIES 1201 West Willow | Enid, Oklahoma, 73703 | 580.242.2750 | autrytech.edu COURSE LENGTH Twenty-four-month daytime program î August-July î Monday-Friday Academic hours: 8:15am-3:45pm Clinical hours: Eight-hour shifts between 7am-5pm with some ADMISSION PROCEDURES evening assignments required Applicants should contact Student Services at Autry Technology Center to request an information/application packet. Applicants who have a completed application on file and who have met entrance requirements will be considered for the program. Meeting ADULT IN-DISTRICT COSTS the requirements does not guarantee admission to the program. Qualified applicants will be contacted for an interview, and class Year One: $2732 (Additional cost of books and supplies approx: $1820) selection will be determined by the admissions committee. -

Acr–Nasci–Sir–Spr Practice Parameter for the Performance and Interpretation of Body Computed Tomography Angiography (Cta)
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2021 (Resolution 47)* ACR–NASCI–SIR–SPR PRACTICE PARAMETER FOR THE PERFORMANCE AND INTERPRETATION OF BODY COMPUTED TOMOGRAPHY ANGIOGRAPHY (CTA) PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

ACR–SPR-STR Practice Parameter for the Performance of Chest Radiography
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2017 (Resolution 2)* ACR–SPR–STR PRACTICE PARAMETER FOR THE PERFORMANCE OF CHEST RADIOGRAPHY PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

Estimation of the Collective Effective Dose to the Population from Medical X-Ray Examinations in Finland
Estimation of the collective effective dose to the population from medical x-ray examinations in Finland Petra Tenkanen-Rautakoskia, Hannu Järvinena, Ritva Blya aRadiation and Nuclear Safety Authority (STUK), PL 14, 00880 Helsinki, Finland Abstract. The collective effective dose to the population from all x-ray examinations in Finland in 2005 was estimated. The numbers of x-ray examinations were collected by a questionnaire to the health care units (response rate 100 %). The effective doses in plain radiography were calculated using a Monte Carlo based program (PCXMC), as average values for selected health care units. For computed tomography (CT), weighted dose length product (DLPw) in a standard phantom was measured for routine CT protocols of four body regions, for 80 % of CT scanners including all types. The effective doses were calculated from DPLw values using published conversion factors. For contrast-enhanced radiology and interventional radiology, the effective dose was estimated mainly by using published DAP values and conversion factors for given body regions. About 733 examinations per 1000 inhabitants (excluding dental) were made in 2005, slightly less than in 2000. The proportions of plain radiography, computed tomography, contrast-enhanced radiography and interventional procedures were about 92, 7, 1 and 1 %, respectively. From 2000, the frequencies (number of examinations per 1000 inhabitants) of plain radiography and contrast-enhanced radiography have decreased about 8 and 33 %, respectively, while the frequencies of CT and interventional radiology have increased about 28 and 38 %, respectively. The population dose from all x-ray examinations is about 0,43 mSv per person (in 1997 0,5 mSv). -

2019 Radiology Cpt Codes
2019 RADIOLOGY CPT CODES BONE DENSITOMETRY 1 Bone Density/DEXA 77080 CT 1 CT Abd & Pelvis W/ Contrast 74177 1 CT Enterography W/ Contrast 74177 1 CT Max/Facial W/O Contrast 70486 # CT Sinus Complete W/O Contrast 70486 1 CT Abd & Pelvis W W/O Contrast 74178 1 CT Extremity Lower W/ Contrast 73701 1 CT Neck W/ Contrast 70491 # CT Sinus Limited W/O Contrast 76380 1 CT Abd & Pelvis W/O Contrast 74176 1 CT Extremity Lower W/O Contrast 73700 1 CT Neck W/O Contrast 70490 # CT Spine Cervical W/ Contrast 72126 1 CT Abd W/ Contrast 74160 1 CT Extremity Upper W/ Contrast 73201 1 CT Orbit/ IAC W/ Contrast 70481 # CT Spine Cervical W/O Contrast 72125 1 CT Abd W/O Contrast 74150 1 CT Extremity Upper W/O Contrast 73200 1 CT Orbit/ IAC W/O Contrast 70480 # CT Spine Lumbar W/ Contrast 72132 1 CT Abd W W/O Contrast 74170 1 CT Head W/ Contrast 70460 1 CT Orbit/ IAC W W/O Contrast 70482 # CT Spine Lumbar W/O Contrast 72131 1 CT Chest W/ Contrast 71260 1 CT Head W/O Contrast 70450 1 CT Pelvis W/ Contrast 72193 # CT Spine Thoracic W/ Contrast 72129 1 CT Chest W/O Contrast 71250 1 CT Head W W/O Contrast 70470 1 CT Pelvis W/O Contrast 72192 # CT Spine Thoracic W/O Contrast 72128 1 CT Chest W W/O Contrast 71270 1 CT Max/Facial W/ Contrast 70487 1 CT Pelvis W W/O Contrast 72194 # CT Stone Protocol W/O Contrast 74176 CTA 1 Cardiac Calcium Score only 75571 1 CT Angiogram Abd & Pelvis W W/O Contrast 74174 1 CT Angiogram Head W W/O Contrast 70496 # CT / CTA Heart W Contrast 75574 1 CT Angiogram Abdomen W W/O Contrast 74175 1 CT Angiogram Chest W W/O Contrast 71275 -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -
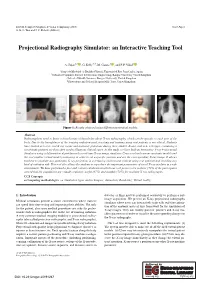
Projectional Radiography Simulator: an Interactive Teaching Tool
EG UK Computer Graphics & Visual Computing (2019) Short Paper G. K. L. Tam and J. C. Roberts (Editors) Projectional Radiography Simulator: an Interactive Teaching Tool A. Sujar1,2 , G. Kelly3,4, M. García1 , and F. P. Vidal2 1Grupo de Modelado y Realidad Virtual, Universidad Rey Juan Carlos, Spain 2School of Computer Science & Electronic Engineering, Bangor University United Kingdom 3School of Health Sciences, Bangor University, United Kingdom 4Shrewsbury and Telford Hospital NHS Trust, United Kingdom Figure 1: Results obtained using different anatomical models. Abstract Radiographers need to know a broad range of knowledge about X-ray radiography, which can be specific to each part of the body. Due to the harmfulness of the ionising radiation used, teaching and training using real patients is not ethical. Students have limited access to real X-ray rooms and anatomic phantoms during their studies. Books, and now web apps, containing a set of static pictures are then often used to illustrate clinical cases. In this study, we have built an Interactive X-ray Projectional Simulator using a deformation algorithm with a real-time X-ray image simulator. Users can load various anatomic models and the tool enables virtual model positioning in order to set a specific position and see the corresponding X-ray image. It allows teachers to simulate any particular X-ray projection in a lecturing environment without using real patients and avoiding any kind of radiation risk. This tool also allows the students to reproduce the important parameters of a real X-ray machine in a safe environment. We have performed a face and content validation in which our tool proves to be realistic (72% of the participants agreed that the simulations are visually realistic), useful (67%) and suitable (78%) for teaching X-ray radiography. -

The Overuse of Diagnostic Imaging and the Choosing Wisely Initiative Vijay M
***ONLINE FIRST: This version will differ from the print version*** Annals of Internal Medicine Ideas and Opinions The Overuse of Diagnostic Imaging and the Choosing Wisely Initiative Vijay M. Rao, MD, and David C. Levin, MD ealth care in America costs too much. There are many common screening and diagnostic tests that they believed Hreasons for this, but an important one is the overuse were overused. The final list contained 37 tests, 18 of of diagnostic tests—including but not limited to imaging which were imaging studies—13 commonly performed by studies. radiologists and 5 commonly performed by cardiologists. A report by Iglehart (1) indicated that, between 2000 In an accompanying editorial, Laine (10) cited an estimate and 2007, use of imaging studies grew faster than that of that up to 5% of the country’s gross national product is any other physician service in the Medicare population. spent on tests and procedures that do not improve patient Another report by the influential group America’s Health outcomes. Considerable overlap exists between the ACP’s Insurance Plans (2) claimed that 20% to 50% of all “high- 18 imaging tests and the 16 in the Table. tech” imaging provides no useful information and may be This suggests a widespread perception among many unnecessary. Reports like these have led to cost concerns branches of medicine that imaging is overused. We agree among key federal agencies like the Congressional Budget that all 16 of the tests shown in the Table are overused. Office, Government Accountability Office, and Medicare We hope that all physicians who order imaging tests will Payment Advisory Commission (3, 4), and steps have been reflect on the Choosing Wisely lists and adjust their order- taken in recent years to reduce reimbursements for imaging ing patterns accordingly. -

What Is Diagnostic Medical Sonography?
WHAT IS DIAGNOSTIC MEDICAL SONOGRAPHY? Diagnostic Medical Sonography is a medical imaging modality that uses sound waves to identify and evaluate soft tissue structures in the human body for disease and pathology. WHAT DOES A DIAGNOSTIC MEDICAL SONOGRAPHER DO? The diagnostic medical sonographer is a healthcare professional who performs diagnostic ultrasound examinations under a physician's supervision. To perform imaging evaluations on patients in the clinical setting, sonographers are required to integrate medical knowledge of anatomy and physiology, pathology, and ultrasound physics. Among the parts of the body most commonly evaluated with sonography are the heart and blood vessels, abdominal organs, superficial structures, pelvic organs and the developing fetus. Sonographers have extensive, direct patient contact that may include performing some invasive procedures. They must be able to interact compassionately and effectively with people who range from healthy to critically ill. The professional responsibilities include, but are not limited, to: • obtaining and recording an accurate patient history • performing diagnostic procedures and obtaining diagnostic images • analyzing technical information • using independent judgment in recognizing the need to extend the scope of the procedure according to the diagnostic findings • providing an oral or written summary of the technical findings to the physician for medical diagnosis • providing quality patient care • collaborating with physicians and other members of the health care team. Sonographers must also be knowledgeable about and limit the risk from possible exposure to blood and body fluids. Many sonographers also assist in electronic and clerical scheduling, record keeping, and computerized image archiving. Sonographers may also have managerial or supervisory responsibilities. Students and sonographers must comply with the ethical behavior expected of a healthcare professional. -

Download Article (PDF)
Current Directions in Biomedical Engineering 2015; 1:257–260 Thomas Homann*, Axel Boese, Sylvia Glaßer, Martin Skalej, and Oliver Beuing Intravascular optical coherence tomography (OCT) as an additional tool for the assessment of stent structures Abstract: Evaluation of the vascular stent position, shape cases an additional imaging of the implants by OCT would and correct expansion has a high relevance in therapy be benecial. In our study, we determined the ability of and diagnosis. Hence, the wall apposition in vessel areas OCT to image structural information of dierent vascular with diering diameters and the appearance of torsions or stents in a phantom study. structural defects of the implant body caused by catheter based device dropping are of special interest. Neurovascu- lar implants like braided ow diverter and laser cut stents 2 Materials and methods consist of metal struts and wires with diameters of about 40 µm. Depending on the implants material composition, A plastic model with bores of dierent diameters for the in- visibility is poor with conventional 2D X-ray uoroscopic take of 3 vascular implants was manufactured (see Figure and radiographic imaging. The metal structures of the im- 1). The model has a geometrical extend of 80 mm×50 mm× plants also lead to artifacts in 3D X-ray images and can 15 mm and a straight course of the bores. A translucent hamper the assessment of the device position. We inves- plastic material was selected for a low absorption of near tigated intravascular optical coherence tomography (OCT) infrared light generated by the OCT system. Objects of in- as a new imaging tool for the evaluation of the vascular vestigation were 3 vascular stents with dierent geometri- stent position, its shape and its correct expansion for 3 dif- cal and structural properties (see Table 1).