The Costs and Benefits of Moving to the ICD-10 Code Sets
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Presence of ROS in Inflammatory Environment of Peri-Implantitis Tissue
Journal of Clinical Medicine Article Presence of ROS in Inflammatory Environment of Peri-Implantitis Tissue: In Vitro and In Vivo Human Evidence 1, 2, 2, 3 4 Eitan Mijiritsky y, Letizia Ferroni y, Chiara Gardin y, Oren Peleg , Alper Gultekin , Alper Saglanmak 4, Lucia Gemma Delogu 5, Dinko Mitrecic 6, Adriano Piattelli 7, 8, 2,9, , Marco Tatullo z and Barbara Zavan * z 1 Head and Neck Maxillofacial Surgery, Department of Otoryngology, Tel-Aviv Sourasky Medical Center, Sackler Faculty of Medicine, Tel-Aviv University, Weizmann street 6, 6423906 Tel-Aviv, Israel; [email protected] 2 Maria Cecilia Hospital, GVM Care & Research, Cotignola, 48033 Ravenna, Italy; [email protected] (L.F.); [email protected] (C.G.) 3 Department of Otolaryngology Head and Neck Surgery and Maxillofacial Surgery, Tel-Aviv Sourasky Medical Center, Sackler School of Medicine, Tel Aviv University, 701990 Tel-Aviv, Israel; [email protected] 4 Istanbul University, Faculty of Dentistry, Department of Oral Implantology, 34093 Istanbul, Turkey; [email protected] (A.G.); [email protected] (A.S.) 5 University of Padova, DpT Biomedical Sciences, 35133 Padova, Italy; [email protected] 6 School of Medicine, Croatian Institute for Brain Research, University of Zagreb, Šalata 12, 10 000 Zagreb, Croatia; [email protected] 7 Department of Medical, Oral, and Biotechnological Sciences, University of Chieti-Pescara, via dei Vestini 31, 66100 Chieti, Italy; [email protected] 8 Marrelli Health-Tecnologica Research Institute, Biomedical Section, Street E. Fermi, 88900 Crotone, Italy; [email protected] 9 Department of Medical Sciences, University of Ferrara, via Fossato di Mortara 70, 44123 Ferara, Italy * Correspondence: [email protected] Co-first author. -

Gyn Oncology Colposcopy I. Basic Science/Mechanisms of Disease A
Gyn Oncology Colposcopy I. Basic Science/Mechanisms of Disease A. Genetics 1. Describe the clinical relevance of viral oncogenes. 2. Describe the role of aneuploidy in the pathogenesis of neoplasia. 3. Describe the inheritance patterns for malignancies of the pelvic organs and breast. 4. Describe the cell replication cycle, and identify the phases of the cycle most sensitive to radiation and chemotherapy. 5. Describe the genetic basis for tumor immunotherapy. B. Physiology 1. Describe the ability of vital organ systems to tolerate cancer therapy. 2. Describe the changes in cellular physiology that result from injury due to radiation and chemotherapy. 3. Describe the metabolic changes that occur in patients with a malignancy of the pelvic organs or breast. C. Embroyology 1. Describe the embryology of gonadal migration and its role in the pathogenesis of epithelial cell tumors. 2. Describe the pathogenesis of gonadal tumors in patients with gonadal dysgenesis. 3. Describe the embryologic precursors of ovarian germ cell tumors. D. Anatomy 1. Describe the gross histologic anatomy of the pelvic organs and breast. 2. Describe the vascular, lymphatic, and nerve supply to each of the pelvic organs. 3. Describe the anatomic relationship between the reproductive organs and other viscera, such as bladder, ureters, and bowel. 4. Describe the likely changes in the anatomic relationships of the pelvic and abdominal viscera created by surgical or radiation treatment for malignancy. E. Pharmacology 1. List major chemotherapeutic agents used for treatment of malignancies of the reproductive organs and breast. 2. Describe the principal adverse effects of the major chemotherapeutic agents. 3. Describe the medications of most value in treatment of complications resulting from chemotherapy and irradiation, such as: a. -

Physiology of Female Sexual Function and Dysfunction
International Journal of Impotence Research (2005) 17, S44–S51 & 2005 Nature Publishing Group All rights reserved 0955-9930/05 $30.00 www.nature.com/ijir Physiology of female sexual function and dysfunction JR Berman1* 1Director Female Urology and Female Sexual Medicine, Rodeo Drive Women’s Health Center, Beverly Hills, California, USA Female sexual dysfunction is age-related, progressive, and highly prevalent, affecting 30–50% of American women. While there are emotional and relational elements to female sexual function and response, female sexual dysfunction can occur secondary to medical problems and have an organic basis. This paper addresses anatomy and physiology of normal female sexual function as well as the pathophysiology of female sexual dysfunction. Although the female sexual response is inherently difficult to evaluate in the clinical setting, a variety of instruments have been developed for assessing subjective measures of sexual arousal and function. Objective measurements used in conjunction with the subjective assessment help diagnose potential physiologic/organic abnormal- ities. Therapeutic options for the treatment of female sexual dysfunction, including hormonal, and pharmacological, are also addressed. International Journal of Impotence Research (2005) 17, S44–S51. doi:10.1038/sj.ijir.3901428 Keywords: female sexual dysfunction; anatomy; physiology; pathophysiology; evaluation; treatment Incidence of female sexual dysfunction updated the definitions and classifications based upon current research and clinical practice. -
Overview of Biomaterials and Their Use in Medical Devices
© 2003 ASM International. All Rights Reserved. www.asminternational.org Handbook of Materials for Medical Devices (#06974G) CHAPTER 1 Overview of Biomaterials and Their Use in Medical Devices A BIOMATERIAL, as defined in this hand- shapes, have relatively low cost, and be readily book, is any synthetic material that is used to available. replace or restore function to a body tissue and Figure 1 lists the various material require- is continuously or intermittently in contact with ments that must be met for successful total joint body fluids (Ref 1). This definition is somewhat replacement. The ideal material or material restrictive, because it excludes materials used combination should exhibit the following prop- for devices such as surgical or dental instru- erties: ments. Although these instruments are exposed A biocompatible chemical composition to to body fluids, they do not replace or augment • avoid adverse tissue reactions the function of human tissue. It should be noted, Excellent resistance to degradation (e.g., cor- however, that materials for surgical instru- • rosion resistance for metals or resistance to ments, particularly stainless steels, are reviewed biological degradation in polymers) briefly in Chapter 3, “Metallic Materials,” in Acceptable strength to sustain cyclic loading this handbook. Similarly, stainless steels and • endured by the joint shape memory alloys used for dental/endodon- A low modulus to minimize bone resorption tic instruments are discussed in Chapter 10, • High wear resistance to minimize wear- “Biomaterials for Dental Applications.” • debris generation Also excluded from the aforementioned defi- nition are materials that are used for external prostheses, such as artificial limbs or devices Uses for Biomaterials (Ref 3) such as hearing aids. -

Anterior Reconstruction Techniques for Cervical Spine Deformity
Neurospine 2020;17(3):534-542. Neurospine https://doi.org/10.14245/ns.2040380.190 pISSN 2586-6583 eISSN 2586-6591 Review Article Anterior Reconstruction Techniques Corresponding Author for Cervical Spine Deformity Samuel K. Cho 1,2 1 1 1 https://orcid.org/0000-0001-7511-2486 Murray Echt , Christopher Mikhail , Steven J. Girdler , Samuel K. Cho 1Department of Orthopedics, Icahn School of Medicine at Mount Sinai, New York, NY, USA Department of Orthopaedics, Icahn 2 Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, School of Medicine at Mount Sinai, 425 NY, USA West 59th Street, 5th Floor, New York, NY, USA E-mail: [email protected] Cervical spine deformity is an uncommon yet severely debilitating condition marked by its heterogeneity. Anterior reconstruction techniques represent a familiar approach with a range Received: June 24, 2020 of invasiveness and correction potential—including global or focal realignment in the sagit- Revised: August 5, 2020 tal and coronal planes. Meticulous preoperative planning is required to improve or prevent Accepted: August 17, 2020 neurologic deterioration and obtain satisfactory global spinal harmony. The ability to per- form anterior only reconstruction requires mobility of the opposite column to achieve cor- rection, unless a combined approach is planned. Anterior cervical discectomy and fusion has limited focal correction, but when applied over multiple levels there is a cumulative ef- fect with a correction of approximately 6° per level. Partial or complete corpectomy has the ability to correct sagittal deformity as well as decompress the spinal canal when there is an- terior compression behind the vertebral body. -
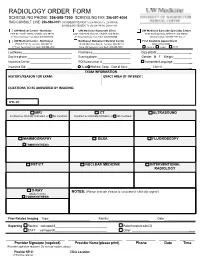
Radiology Order Form
RADIOLOGY ORDER FORM SCHEDULING PHONE: 206-598-7200 SCHEDULING FAX: 206-597-4004 RAD CONSULT LINE: 206-598-0101 UW RADIOLOGY RECORDS: Tel: 206-598-6206 Fax: 206-598-7690 NW RADIOLOGY RECORDS: Tel: 206-668-1748 Fax: 206-688-1398 UW Medical Center - Montlake UW Medicine Roosevelt Clinic UW Medicine Eastside Specialty Center 1959 NE Pacific Street, Seattle, WA 98195 4245 Roosevelt Way NE, Seattle, WA 98105 3100 Northup Way, Bellevue, WA 98004 2nd Floor Radiology Front Desk: 206-598-6200 2nd Floor Radiology Front Desk: 206-598-6868 ESC Front Desk: 425-646-7777 Opt. 2 UW Medical Center - Northwest Northwest Outpatient Medical Center First Available Appointment 1550 N 115th St, Seattle, WA 98133 10330 Meridian Ave N, Seattle, WA 98133 (ANY LOCATION) 2nd Floor Radiology Front Desk: 206-668-1302 Suite 130 Radiology Front Desk: 206-668-6050 Routine Urgent STAT Last Name: First Name: Date of Birth: _ Daytime phone: Evening phone: Gender: M F Weight:___________ Insurance Carrier: RQI/Authorization #: Interpreter/Language: __ Insurance ID#: Auto Workers’ Comp Date of Injury: ______ Claim # __ EXAM INFORMATION HISTORY/REASON FOR EXAM: EXACT AREA OF INTEREST: EXAM INFORMATION QUESTIONS TO BE ANSWERED BY IMAGING: ICD-10: MRI CT ULTRASOUND Contrast as clinically indicated, or No Contrast Contrast as clinically indicated, or No Contrast MAMMOGRAPHY DEXA FLUOROSCOPY TOMOSYNTHESIS PET/CT NUCLEAR MEDICINE INTERVENTIONAL RADIOLOGY X-RAY NOTES: (Please indicate if exam is considered “clinically urgent”) (Walk-In Only) TOMOSYNTHESIS Prior Related Imaging Type:_________________________ Facility:_________________________ Date:___________________ Reporting Routine call report # Patient to return with CD STAT call report # Other: __________ ________________________ ______________________ ____________ _______ ______ Provider Signature (required) Provider Name (please print) Phone Date Time (Provider signature required. -

RADIOGRAPHY to Prepare Individuals to Become Registered Radiologic Technologists
RADIOGRAPHY To prepare individuals to become Registered Radiologic Technologists. THE WORKFORCE CAPITAL This two-year, advanced medical program trains students in radiography. Radiography uses radiation to produce images of tissues, organs, bones and vessels of the body. The radiographer is an essential member of the health care team who works in a variety of settings. Responsibili- ties include accurately positioning the patient, producing quality diagnostic images, maintaining equipment and keeping computerized records. This certificate program of specialized training focuses on each of these responsibilities. Graduates are eligible to apply for the national credential examination to become a registered technologist in radiography, RT(R). Contact Student Services for current tuition rates and enrollment information. 580.242.2750 Mission, Goals, and Student Learning Outcomes Program Effectiveness Data Radiography Program Guidelines (Policies and Procedures) “The programs at Autry prepare you for the workforce with no extra training needed after graduation.” – Kenedy S. autrytech.edu ENDLESS POSSIBILITIES 1201 West Willow | Enid, Oklahoma, 73703 | 580.242.2750 | autrytech.edu COURSE LENGTH Twenty-four-month daytime program î August-July î Monday-Friday Academic hours: 8:15am-3:45pm Clinical hours: Eight-hour shifts between 7am-5pm with some ADMISSION PROCEDURES evening assignments required Applicants should contact Student Services at Autry Technology Center to request an information/application packet. Applicants who have a completed application on file and who have met entrance requirements will be considered for the program. Meeting ADULT IN-DISTRICT COSTS the requirements does not guarantee admission to the program. Qualified applicants will be contacted for an interview, and class Year One: $2732 (Additional cost of books and supplies approx: $1820) selection will be determined by the admissions committee. -

Spinal Interventional Pain Management and Lumbar Spine Surgery
Spinal Interventional Pain Management and Lumbar Spine Surgery Policy Number: Original Effective Date: MM.06.024 01/01/2014 Line(s) of Business: Current Effective Date: HMO; PPO; QUEST Integration 12/15/2017 Section: Surgery; Medicine Place(s) of Service: Office; Outpatient; Inpatient I. Description The following spinal interventional pain management and lumbar spine surgery procedures require precertification through Magellan Hawaii, formally known as National Imaging Associates, Inc. (NIA): A. Spinal Epidural Injections B. Paravertebral Facet Joint Denervation (radiofrequency neurolysis) C. Paravertebral Facet Joint Injections or Blocks D. Sacroiliac joint injections E. Lumbar Spinal Fusion Surgery II. Administrative Guidelines A. The ordering physician can obtain precertification or consult with Magellan Hawaii by accessing their website at http://www.radmd.com/ or by calling 1 (866) 306-9729, from 6 a.m. to 6 p.m., weekdays, Hawaii Time. Refer to the e-library for instructions on navigating the radmd.com website (RadMD Get Started) and requesting precertification/checking the status of a request (RadMD QuickStart). B. For access to the latest clinical guidelines used for precertification, go to www.radmd.com and click on the link entitled View Clinical Guidelines. C. For interventional pain management procedures (epidural injections, facet joint denervation neurolysis, facet joint injections and sacroiliac joint injections), if more than one procedure is planned, a separate precertification number must be obtained for each procedure planned. D. For spinal surgeries (lumbar fusions, lumbar decompressions, and lumbar microdiscectomy), one precertification number should be obtained for the most invasive surgery to be performed. E. Precertification requirements for injection procedures apply only to office and outpatient services (POS 11, 22, or 24). -

Automated Percutaneous and Endoscopic Discectomy
Corporate Medical Policy Automated Percutaneous and Endoscopic Discectomy File Name: percutaneous_discectomy Origination: 9/1991 Last CAP Review: 5/2021 Next CAP Review: 5/2022 Last Review: 5/2021 Description of Procedure or Service Surgical management of herniated intervertebral discs most commonly involves discectomy or microdiscectomy, performed manually through an open incision. Automated percutaneous discectomy involves placement of a probe within the intervertebral disc under image guidance with aspiration of disc material using a suction cutting device. Removal of disc herniations under endoscopic visualization is also being investigated. Endoscopic discectomy involves the percutaneous placement of a working channel under image guidance, followed by visualization of the working space and instruments through an endoscope, and aspiration of disc material. Back pain or radiculopathy related to herniated discs is an extremely common condition and a frequent cause of chronic disability. Although many cases of acute low back pain and radiculopathy will resolve with conservative care, a surgical decompression is often considered when the pain is unimproved after several months and is clearly neuropathic in origin, resulting from irritation of the nerve roots. Open surgical treatment typically consists of discectomy, in which the extruding disc material is excised. When performed with an operating microscope the procedure is known as microdiscectomy. Minimally invasive options have also been researched, in which some portion of the disc is removed or ablated, although these techniques are not precisely targeted at the offending extruding disc material. Ablative techniques include laser discectomy and radiofrequency (RF) decompression. In addition, intradiscal electrothermal annuloplasty is another minimally invasive approach to low back pain. -

Information for Patients Having a Sigmoid Colectomy
Patient information – Pre-operative Assessment Clinic Information for patients having a sigmoid colectomy This leaflet will explain what will happen when you come to the hospital for your operation. It is important that you understand what to expect and feel able to take an active role in your treatment. Your surgeon will have already discussed your treatment with you and will give advice about what to do when you get home. What is a sigmoid colectomy? This operation involves removing the sigmoid colon, which lies on the left side of your abdominal cavity (tummy). We would then normally join the remaining left colon to the top of the rectum (the ‘storage’ organ of the bowel). The lines on the attached diagram show the piece of bowel being removed. This operation is done with you asleep (general anaesthetic). The operation not only removes the bowel containing the tumour but also removes the draining lymph glands from this part of the bowel. This is sent to the pathologists who will then analyse each bit of the bowel and the lymph glands in detail under the microscope. This operation can often be completed in a ‘keyhole’ manner, which means less trauma to the abdominal muscles, as the biggest wound is the one to remove the bowel from the abdomen. Sometimes, this is not possible, in which case the same operation is done through a bigger incision in the abdominal wall – this is called an ‘open’ operation. It does take longer to recover with an open operation but, if it is necessary, it is the safest thing to do. -

Controversies and Complications in Pelvic Reconstructive Surgery (Didactic)
Controversies and Complications in Pelvic Reconstructive Surgery (Didactic) PROGRAM CHAIR Andrew I. Sokol, MD Cheryl B. Iglesia, MD Charles R. Rardin, MD Sponsored by AAGL Advancing Minimally Invasive Gynecology Worldwide Professional Education Information Target Audience Educational activities are developed to meet the needs of surgical gynecologists in practice and in training, as well as, other allied healthcare professionals in the field of gynecology. Accreditation AAGL is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. The AAGL designates this live activity for a maximum of 3.75 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. DISCLOSURE OF RELEVANT FINANCIAL RELATIONSHIPS As a provider accredited by the Accreditation Council for Continuing Medical Education, AAGL must ensure balance, independence, and objectivity in all CME activities to promote improvements in health care and not proprietary interests of a commercial interest. The provider controls all decisions related to identification of CME needs, determination of educational objectives, selection and presentation of content, selection of all persons and organizations that will be in a position to control the content, selection of educational methods, and evaluation of the activity. Course chairs, planning committee members, presenters, authors, moderators, panel members, and others in a position to control the content of this activity are required to disclose relevant financial relationships with commercial interests related to the subject matter of this educational activity. Learners are able to assess the potential for commercial bias in information when complete disclosure, resolution of conflicts of interest, and acknowledgment of commercial support are provided prior to the activity. -

Gender Reassignment Surgery Policy Number: PG0311 ADVANTAGE | ELITE | HMO Last Review: 07/01/2021
Gender Reassignment Surgery Policy Number: PG0311 ADVANTAGE | ELITE | HMO Last Review: 07/01/2021 INDIVIDUAL MARKETPLACE | PROMEDICA MEDICARE PLAN | PPO GUIDELINES This policy does not certify benefits or authorization of benefits, which is designated by each individual policyholder terms, conditions, exclusions and limitations contract. It does not constitute a contract or guarantee regarding coverage or reimbursement/payment. Self-Insured group specific policy will supersede this general policy when group supplementary plan document or individual plan decision directs otherwise. Paramount applies coding edits to all medical claims through coding logic software to evaluate the accuracy and adherence to accepted national standards. This medical policy is solely for guiding medical necessity and explaining correct procedure reporting used to assist in making coverage decisions and administering benefits. SCOPE X Professional X Facility DESCRIPTION Transgender is a broad term that can be used to describe people whose gender identity is different from the gender they were thought to be when they were born. Gender dysphoria (GD) or gender identity disorder is defined as evidence of a strong and persistent cross-gender identification, which is the desire to be, or the insistence that one is of the other gender. Persons with this disorder experience a sense of discomfort and inappropriateness regarding their anatomic or genetic sexual characteristics. Individuals with GD have persistent feelings of gender discomfort and inappropriateness of their anatomical sex, strong and ongoing cross-gender identification, and a desire to live and be accepted as a member of the opposite sex. Gender Dysphoria (GD) is defined by the Diagnostic and Statistical Manual of Mental Disorders - Fifth Edition, DSM-5™ as a condition characterized by the "distress that may accompany the incongruence between one’s experienced or expressed gender and one’s assigned gender" also known as “natal gender”, which is the individual’s sex determined at birth.