The Practice Standards for Medical Imaging and Radiation Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RADIOGRAPHY to Prepare Individuals to Become Registered Radiologic Technologists
RADIOGRAPHY To prepare individuals to become Registered Radiologic Technologists. THE WORKFORCE CAPITAL This two-year, advanced medical program trains students in radiography. Radiography uses radiation to produce images of tissues, organs, bones and vessels of the body. The radiographer is an essential member of the health care team who works in a variety of settings. Responsibili- ties include accurately positioning the patient, producing quality diagnostic images, maintaining equipment and keeping computerized records. This certificate program of specialized training focuses on each of these responsibilities. Graduates are eligible to apply for the national credential examination to become a registered technologist in radiography, RT(R). Contact Student Services for current tuition rates and enrollment information. 580.242.2750 Mission, Goals, and Student Learning Outcomes Program Effectiveness Data Radiography Program Guidelines (Policies and Procedures) “The programs at Autry prepare you for the workforce with no extra training needed after graduation.” – Kenedy S. autrytech.edu ENDLESS POSSIBILITIES 1201 West Willow | Enid, Oklahoma, 73703 | 580.242.2750 | autrytech.edu COURSE LENGTH Twenty-four-month daytime program î August-July î Monday-Friday Academic hours: 8:15am-3:45pm Clinical hours: Eight-hour shifts between 7am-5pm with some ADMISSION PROCEDURES evening assignments required Applicants should contact Student Services at Autry Technology Center to request an information/application packet. Applicants who have a completed application on file and who have met entrance requirements will be considered for the program. Meeting ADULT IN-DISTRICT COSTS the requirements does not guarantee admission to the program. Qualified applicants will be contacted for an interview, and class Year One: $2732 (Additional cost of books and supplies approx: $1820) selection will be determined by the admissions committee. -

ACR–SPR-STR Practice Parameter for the Performance of Chest Radiography
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2017 (Resolution 2)* ACR–SPR–STR PRACTICE PARAMETER FOR THE PERFORMANCE OF CHEST RADIOGRAPHY PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

MRC Review of Positron Emission Tomography (PET) Within the Medical Imaging Research Landscape
MRC Review of Positron Emission Tomography (PET) within The Medical Imaging Research Landscape August 2017 Content 1 Introduction 3 2 The medical imaging research landscape in the UK 4 2.1 Magnetic resonance imaging (MRI) 4 2.2 PET, including PET-MRI 6 2.3 Magnetoencephalography 7 3 Scientific uses and demand for PET imaging 8 3.1 Clinical practice 8 3.2 Research use of PET 8 3.3 Demand for PET 10 4 Bottlenecks 11 4.1 Cost 11 4.2 Radiochemistry requirements 12 4.3 Capacity 13 4.4 Analysis and modelling 13 5 Future Opportunities 14 5.1 Mitigating the high costs 14 5.2 Capacity building 14 5.3 Better Networking 15 6 Discussion and conclusions 16 Appendix 1 Experts consulted in the review 17 Appendix 2 Interests of other funders 18 Appendix 3 Usage and cost of PET in research 21 Appendix 4 Summary of facilities and capabilities across UK PET centres of excellence 23 2 1. Introduction This report aims to provide a review of Positron Emission Tomography (PET) within the medical imaging research landscape and a high level strategic review of the UK’s capabilities and needs in this area. The review was conducted by face-to-face and telephone interviews with 35 stakeholders from UK centres of excellence, international experts, industry and other funders (list at appendix 1). Data were also collected on facilities, resources and numbers of scans conducted across the centres of excellence using a questionnaire. The review has focused predominantly on PET imaging, but given MRC’s significant recent investment in other imaging modalities (7T Magnetic Resonance Imaging (MRI), hyperpolarised MRI) through the Clinical Research Infrastructure (CRI) Initiative, these are also considered more briefly. -
Having an Aortic Arch-Angiogram
Information for patients Having an Aortic Arch-Angiogram Sheffield Teaching Hospitals Other names: Aortic arch-angiogram, arch-angiogram, arch-aortogram. You have been given this leaflet because you need a procedure known as an Aortic Arch-Angiogram. This leaflet explains more about Aortic Arch-Angiograms, and answers some of the most frequently asked questions. If, after reading this leaflet, you have any questions or concerns, you should write them down and discuss them at your next appointment with the consultant, doctor or specialist nurse. It is important that you understand the procedure, along with the potential benefits and risks before you agree to it. Where will my hospital appointments take place? This will depend on which specialist doctor you are seen by. You could be seen by a Neurologist, a Stroke Physician, a Vascular Surgeon or a Radiologist. Most of the appointments will be at either the Northern General or Royal Hallamshire Hospitals. However, you may also be seen at one of the outreach clinics at Rotherham or Barnsley District Hospitals. 2 What is an aortic arch-angiogram? An aortic arch-angiogram is an x-ray test that enables us to diagnose a problem (most commonly a narrowing or a blockage) in the arteries supplying your head, neck and arms. Arteries do not usually show up on x-rays, so the images are obtained by introducing a long, thin, flexible tube (a catheter) into an artery, usually at the top of your leg. Then, a special x-ray dye (contrast medium) is injected through it, into the circulation. The blood flow carries the dye along, highlighting the arteries, and x-ray pictures are taken. -

Estimation of the Collective Effective Dose to the Population from Medical X-Ray Examinations in Finland
Estimation of the collective effective dose to the population from medical x-ray examinations in Finland Petra Tenkanen-Rautakoskia, Hannu Järvinena, Ritva Blya aRadiation and Nuclear Safety Authority (STUK), PL 14, 00880 Helsinki, Finland Abstract. The collective effective dose to the population from all x-ray examinations in Finland in 2005 was estimated. The numbers of x-ray examinations were collected by a questionnaire to the health care units (response rate 100 %). The effective doses in plain radiography were calculated using a Monte Carlo based program (PCXMC), as average values for selected health care units. For computed tomography (CT), weighted dose length product (DLPw) in a standard phantom was measured for routine CT protocols of four body regions, for 80 % of CT scanners including all types. The effective doses were calculated from DPLw values using published conversion factors. For contrast-enhanced radiology and interventional radiology, the effective dose was estimated mainly by using published DAP values and conversion factors for given body regions. About 733 examinations per 1000 inhabitants (excluding dental) were made in 2005, slightly less than in 2000. The proportions of plain radiography, computed tomography, contrast-enhanced radiography and interventional procedures were about 92, 7, 1 and 1 %, respectively. From 2000, the frequencies (number of examinations per 1000 inhabitants) of plain radiography and contrast-enhanced radiography have decreased about 8 and 33 %, respectively, while the frequencies of CT and interventional radiology have increased about 28 and 38 %, respectively. The population dose from all x-ray examinations is about 0,43 mSv per person (in 1997 0,5 mSv). -
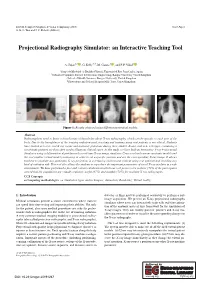
Projectional Radiography Simulator: an Interactive Teaching Tool
EG UK Computer Graphics & Visual Computing (2019) Short Paper G. K. L. Tam and J. C. Roberts (Editors) Projectional Radiography Simulator: an Interactive Teaching Tool A. Sujar1,2 , G. Kelly3,4, M. García1 , and F. P. Vidal2 1Grupo de Modelado y Realidad Virtual, Universidad Rey Juan Carlos, Spain 2School of Computer Science & Electronic Engineering, Bangor University United Kingdom 3School of Health Sciences, Bangor University, United Kingdom 4Shrewsbury and Telford Hospital NHS Trust, United Kingdom Figure 1: Results obtained using different anatomical models. Abstract Radiographers need to know a broad range of knowledge about X-ray radiography, which can be specific to each part of the body. Due to the harmfulness of the ionising radiation used, teaching and training using real patients is not ethical. Students have limited access to real X-ray rooms and anatomic phantoms during their studies. Books, and now web apps, containing a set of static pictures are then often used to illustrate clinical cases. In this study, we have built an Interactive X-ray Projectional Simulator using a deformation algorithm with a real-time X-ray image simulator. Users can load various anatomic models and the tool enables virtual model positioning in order to set a specific position and see the corresponding X-ray image. It allows teachers to simulate any particular X-ray projection in a lecturing environment without using real patients and avoiding any kind of radiation risk. This tool also allows the students to reproduce the important parameters of a real X-ray machine in a safe environment. We have performed a face and content validation in which our tool proves to be realistic (72% of the participants agreed that the simulations are visually realistic), useful (67%) and suitable (78%) for teaching X-ray radiography. -

Diagnostic Radiography Is the Production of High Quality Images for the Purpose of Diagnosis of Injury Or Disease
A Career in Medical Imaging What is Diagnostic Radiography / Medical Imaging? Diagnostic Radiography is the production of high quality images for the purpose of diagnosis of injury or disease. It is a pivotal aspect of medicine and a patient's diagnosis and ultimate treatment is often dependent on the images produced. Diagnostic Radiography uses both ionising and non-ionising radiation in the imaging process. The equipment used is at the high end of technology and computerisation within medicine. What does a Diagnostic Radiographer / Medical Imaging Technologist do? A Diagnostic Radiographer/Medical Imaging Technologist is a key member of the health care team. They are responsible for producing high quality medical images that assist medical specialists and practitioners to describe, diagnose, monitor and treat a patient’s injury or illness. Much of the medical equipment used to gain the images is highly technical and involves state of the art computerisation. A Diagnostic Radiographer/Medical Imaging Technologist needs to have the scientific and technological background to understand and use the equipment within a modern Radiology department as well as compassion and strong interpersonal skills. They need to be able to demonstrate care and understanding and have a genuine interest in a patient's welfare. The Diagnostic Radiographer/Medical Imaging Technologist will also need to be able to explain to the patient the need for the preparation and post examination care as well as the procedure to be undertaken. The Diagnostic Radiographer/Medical Imaging Technologist is able to work in a highly advanced technical profession that requires excellent people skills. It is an exciting and rewarding profession to embark on and great opportunities await the graduate. -

The Role of the GI Radiographer: a UK Perspective Nightingale, J and Hogg, P
The role of the GI radiographer: A UK perspective Nightingale, J and Hogg, P Title The role of the GI radiographer: A UK perspective Authors Nightingale, J and Hogg, P Type Article URL This version is available at: http://usir.salford.ac.uk/id/eprint/12543/ Published Date 2007 USIR is a digital collection of the research output of the University of Salford. Where copyright permits, full text material held in the repository is made freely available online and can be read, downloaded and copied for non-commercial private study or research purposes. Please check the manuscript for any further copyright restrictions. For more information, including our policy and submission procedure, please contact the Repository Team at: [email protected]. ...................................................................................................... PEER REVIEW The Role of the GI Radiographer: A United Kingdom Perspective JULIE NIGHTINGALE, M.Sc. PETER HOGG, M.Phil. Context Since the 1990s radiographers in the United Kingdom have expanded their role in gastrointestinal (GI) radiology, first by performing double-contrast barium enema (DCBE) examinations independently and later by interpreting and reporting the results of these exams. Objective This article will trace the evolution of GI radiographers in the United Kingdom, evaluate their success and explore how the U.K. experience could apply to American radiologist assistants. Methods The authors surveyed the professional literature to determine the historical context in which GI radiographers emerged and assess how their performance on DCBE exams compares with radiologists’ performance. Results DCBE exams performed by GI radiographers have been shown to be efficient, cost effective and safe. In addition, GI radiographers have helped reduce waiting and turnaround times for DCBE exams. -

Mammography Services Quality Assurance: Baseline Standards for Latin America and the Caribbean
MAMMOGRAPHY SERVICES QUALITY ASSURANCE: BASELINE STANDARDS FOR LATIN AMERICA AND THE CARIBBEAN MAMMOGRAPHY SERVICES QUALITY ASSURANCE: BASELINE STANDARDS FOR LATIN AMERICA AND THE CARIBBEAN Washington, D.C., 2016 Original versión in Spanish: Garantía de calidad de los servicios de mamografía; Normas básicas para América Latina y el Caribe ISBN: 978-92-75-31926-0 PAHO HQ Library Cataloguing-in-Publication Data ********************************************************************************* Pan American Health Organization Mammography Services Quality Assurance: Baseline Standards for Latin America and the Caribbean. Washington, D.C. : PAHO, 2016. 1. Mammography – standards. 2. Mammography – methods. 3. Human Resources. 4. Equipment and Supplies. 5. Health Care Quality, Access, and Evaluation. 6. Americas. I. Title. ISBN: 978-92-75-11926-6 (NLM Classification: WP 815) © Pan American Health Organization, 2016 All rights reserved. Publications of the Pan American Health Organization (PAHO) are available on the PAHO website (www.paho.org). Requests for permission to reproduce or translate PAHO publications should be addressed to the Publications Program through the PAHO website (www.paho.org/permissions). Publications of the Pan American Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights are reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the Pan American Health Organization concerning the status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. -

Download Article (PDF)
Current Directions in Biomedical Engineering 2015; 1:257–260 Thomas Homann*, Axel Boese, Sylvia Glaßer, Martin Skalej, and Oliver Beuing Intravascular optical coherence tomography (OCT) as an additional tool for the assessment of stent structures Abstract: Evaluation of the vascular stent position, shape cases an additional imaging of the implants by OCT would and correct expansion has a high relevance in therapy be benecial. In our study, we determined the ability of and diagnosis. Hence, the wall apposition in vessel areas OCT to image structural information of dierent vascular with diering diameters and the appearance of torsions or stents in a phantom study. structural defects of the implant body caused by catheter based device dropping are of special interest. Neurovascu- lar implants like braided ow diverter and laser cut stents 2 Materials and methods consist of metal struts and wires with diameters of about 40 µm. Depending on the implants material composition, A plastic model with bores of dierent diameters for the in- visibility is poor with conventional 2D X-ray uoroscopic take of 3 vascular implants was manufactured (see Figure and radiographic imaging. The metal structures of the im- 1). The model has a geometrical extend of 80 mm×50 mm× plants also lead to artifacts in 3D X-ray images and can 15 mm and a straight course of the bores. A translucent hamper the assessment of the device position. We inves- plastic material was selected for a low absorption of near tigated intravascular optical coherence tomography (OCT) infrared light generated by the OCT system. Objects of in- as a new imaging tool for the evaluation of the vascular vestigation were 3 vascular stents with dierent geometri- stent position, its shape and its correct expansion for 3 dif- cal and structural properties (see Table 1). -

X-Ray (Radiography) - Bone Bone X-Ray Uses a Very Small Dose of Ionizing Radiation to Produce Pictures of Any Bone in the Body
X-ray (Radiography) - Bone Bone x-ray uses a very small dose of ionizing radiation to produce pictures of any bone in the body. It is commonly used to diagnose fractured bones or joint dislocation. Bone x-rays are the fastest and easiest way for your doctor to view and assess bone fractures, injuries and joint abnormalities. This exam requires little to no special preparation. Tell your doctor and the technologist if there is any possibility you are pregnant. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. What is Bone X-ray (Radiography)? An x-ray exam helps doctors diagnose and treat medical conditions. It exposes you to a small dose of ionizing radiation to produce pictures of the inside of the body. X-rays are the oldest and most often used form of medical imaging. A bone x-ray makes images of any bone in the body, including the hand, wrist, arm, elbow, shoulder, spine, pelvis, hip, thigh, knee, leg (shin), ankle or foot. What are some common uses of the procedure? A bone x-ray is used to: diagnose fractured bones or joint dislocation. demonstrate proper alignment and stabilization of bony fragments following treatment of a fracture. guide orthopedic surgery, such as spine repair/fusion, joint replacement and fracture reductions. look for injury, infection, arthritis, abnormal bone growths and bony changes seen in metabolic conditions. assist in the detection and diagnosis of bone cancer. locate foreign objects in soft tissues around or in bones. How should I prepare? Most bone x-rays require no special preparation. -

The ASRT Practice Standards for Medical Imaging and Radiation Therapy
The ASRT Practice Standards for Medical Imaging and Radiation Therapy Sonography ©2019 American Society of Radiologic Technologists. All rights reserved. Reprinting all or part of this document is prohibited without advance written permission of the ASRT. Send reprint requests to the ASRT Publications Department, 15000 Central Ave. SE, Albuquerque, NM 87123-3909. Effective June 23, 2019 Table of Contents Preface .......................................................................................................................................................... 1 Format ....................................................................................................................................................... 1 Introduction .................................................................................................................................................. 3 Definition .................................................................................................................................................. 3 Education and Certification ...................................................................................................................... 5 Medical Imaging and Radiation Therapy Scope of Practice .......................................................................... 6 Standards ...................................................................................................................................................... 8 Standard One – Assessment ....................................................................................................................