Development of Mefloquine As an Antimalarial Drug* UNDP/WORLD BANK/WHO UPDATE
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Quinoline-Based Hybrid Compounds with Antimalarial Activity
molecules Review Quinoline-Based Hybrid Compounds with Antimalarial Activity Xhamla Nqoro, Naki Tobeka and Blessing A. Aderibigbe * Department of Chemistry, University of Fort Hare, Alice Campus, Alice 5700, Eastern Cape, South Africa; [email protected] (X.N.); [email protected] (N.T.) * Correspondence: [email protected] Received: 7 November 2017; Accepted: 11 December 2017; Published: 19 December 2017 Abstract: The application of quinoline-based compounds for the treatment of malaria infections is hampered by drug resistance. Drug resistance has led to the combination of quinolines with other classes of antimalarials resulting in enhanced therapeutic outcomes. However, the combination of antimalarials is limited by drug-drug interactions. In order to overcome the aforementioned factors, several researchers have reported hybrid compounds prepared by reacting quinoline-based compounds with other compounds via selected functionalities. This review will focus on the currently reported quinoline-based hybrid compounds and their preclinical studies. Keywords: 4-aminoquinoline; 8-aminoquinoline; malaria; infectious disease; hybrid compound 1. Introduction Malaria is a parasitic infectious disease that is a threat to approximately half of the world’s population. This parasitic disease is transmitted to humans by a female Anopheles mosquito when it takes a blood meal. Pregnant women and young children in the sub-tropical regions are more prone to malaria infection. In 2015, 214 million infections were reported, with approximately 438,000 deaths and the African region accounted for 90% of the deaths [1–3]. Malaria is caused by five parasites of the genus Plasmodium, but the majority of deaths are caused by Plasmodium falciparum and Plasmodium vivax [1,4–6]. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

(Artemether / Lumefantrine 20Mg/120 Mg) Tablets
SUMMARY OF PRODUCT CHARACTERISTICS Page 1 of 13 1. NAME OF THE MEDICINAL PRODUCT Lumartem (Artemether / Lumefantrine 20mg/120 mg) Tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains: 20 mg artemether and 120 mg lumefantrine. For a full list of excipients see section 6.1. 3. PHARMACEUTICAL FORM Yellow coloured, circular, uncoated, flat faced, bevelled edged, matt finished tablets with a break line on one side and plain on the other side. The scoreline is only to facilitate breaking for ease of swallowing and not to divide into equal doses. 4. CLINICAL PARTICULARS 4.1 Therapeutic indication Artemether 20 mg and Lumefantrine 120 mg Tablets is indicated for the treatment of uncomplicated cases of malaria due to Plasmodium falciparum in adults, children and infants of 5 kg and above. The most recent official guidelines on the appropriate use of antimalarial agents and local information on the prevalence of resistance to antimalarial drugs must be taken into consideration for deciding on the appropriateness of therapy with Artemether 20 mg and Lumefantrine 120 mg Tablets. Official guidance will normally include WHO (http://whqlibdoc.who.int/publications/2010/9789241547925_eng.pdf) and local health authorities’ guidelines (see also sections 4.4 and 5.1). 4.2 Posology and method of administration Tablets for oral administration. Page 2 of 13 Number of Artemether 20 mg and Lumefantrine 120 mg Tablets for treatment according to weight bands st nd rd Weight range 1 day of 2 day of 3 day treatment treatment of treatment ≥ 5kg -

Traveler Information
Traveler Information QUICK LINKS MALARIA—TRAVELER INFORMATION • Shoreland's Recommendations for Malaria Prevention • What's New • General Information • Symptoms • Disease Risk • Preventive Therapy • Timing of Antimalarial Drugs • Antimalarial Drugs • Pregnancy • Breastfeeding • Infants and Children • When to Seek Medical Attention • Self-Treatment of Presumptive Malaria Traveler Information MALARIA SHORELAND'S RECOMMENDATIONS FOR MALARIA PREVENTION Atovaquone/proguanil (Malarone), doxycycline, chloroquine, and mefloquine are equally effective antimalarial drugs when taken as instructed, as long as there is no resistance to the drug at the destination. In areas of chloroquine-resistant P. falciparum malaria, mefloquine, atovaquone/proguanil, and doxycycline are equally effective drug options. In areas of mefloquine resistance, either doxycycline or atovaquone/proguanil can be used. Another drug, primaquine, can be used in special cases but is not a first-choice drug for prevention. For short-term travelers (less than 2-3 weeks), atovaquone/proguanil may be preferable because travelers can stop taking the drug just 7 days after leaving the malarious area. Longer courses of atovaquone/proguanil appear safe but are more costly than mefloquine or doxycycline. For long-term travelers, mefloquine is preferable—if it is tolerated—due to lower cost and once-weekly doses (rather than daily doses). WHAT'S NEW The FDA has added a warning to the packaging label for mefloquine, stating that it can cause serious neurological and psychiatric side effects. These reactions can persist for months, years, or permanently, even after discontinuation of mefloquine. Use of either atovaquone/proguanil (Malarone) or co-artemether (combination artemether-lumefantrine; called Coartem in the U.S. and Riamet in Europe) is preferred for standby emergency treatment, if this strategy is chosen by the traveler. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -
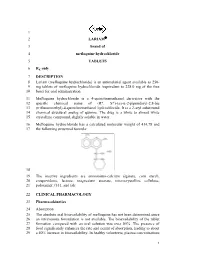
1 2 LARIAM 3 Brand of 4 Mefloquine Hydrochloride 5 TABLETS 6 Rx Only
1 2 LARIAM® 3 brand of 4 mefloquine hydrochloride 5 TABLETS 6 Rx only 7 DESCRIPTION 8 Lariam (mefloquine hydrochloride) is an antimalarial agent available as 250 9 mg tablets of mefloquine hydrochloride (equivalent to 228.0 mg of the free 10 base) for oral administration. 11 Mefloquine hydrochloride is a 4-quinolinemethanol derivative with the 12 specific chemical name of (R*, S*)-(±)-α-2-piperidinyl-2,8-bis 13 (trifluoromethyl)-4-quinolinemethanol hydrochloride. It is a 2-aryl substituted 14 chemical structural analog of quinine. The drug is a white to almost white 15 crystalline compound, slightly soluble in water. 16 Mefloquine hydrochloride has a calculated molecular weight of 414.78 and 17 the following structural formula: 18 19 The inactive ingredients are ammonium-calcium alginate, corn starch, 20 crospovidone, lactose, magnesium stearate, microcrystalline cellulose, 21 poloxamer #331, and talc. 22 CLINICAL PHARMACOLOGY 23 Pharmacokinetics 24 Absorption 25 The absolute oral bioavailability of mefloquine has not been determined since 26 an intravenous formulation is not available. The bioavailability of the tablet 27 formation compared with an oral solution was over 85%. The presence of 28 food significantly enhances the rate and extent of absorption, leading to about 29 a 40% increase in bioavailability. In healthy volunteers, plasma concentrations 1 LARIAM® (mefloquine hydrochloride) 30 peak 6 to 24 hours (median, about 17 hours) after a single dose of Lariam. In a 31 similar group of volunteers, maximum plasma concentrations in μg/L are 32 roughly equivalent to the dose in milligrams (for example, a single 1000 mg 33 dose produces a maximum concentration of about 1000 μg/L). -

Selection for Mefloquine Resistance in Plasmodium Falciparum Is Linked To
Proc. Nati. Acad. Sci. USA Vol. 91, pp. 1143-1147, February 1994 Medical Sciences Selection for mefloquine resistance in Plasmodium falciparum is linked to amplification of the pfmdrl gene and cross-resistance to halofantrine and quinine (drug reistance/malaria/P-glycoprotein/chloroquine) ALAN F. COWMAN*, DENISE GALATIS, AND JENNIFER K. THOMPSON The Walter and Eliza Hall Institute of Medical Research, Melbourne 3050, Australia Communicated by Gustav J. V. Nossal, October 11, 1993 (received for review September 8, 1993) ABSTRACT Two chloroquine-resistant cloned isolates of concomitant with the increase in chloroquine resistance was Plasmodiumfalciparum were subjected to mefloquine selection a decrease in the level of mefloquine resistance. In another to test if this resulted in alterations in chloroquine sensitivity study, selection for mefloquine resistance in the W2 isolate of and amplification ofthepfmdrl gene. The mefloquine-resistant P. falciparum showed a decrease in chloroquine resistance lines derived by this selection were shown to have amplified and (8) and amplification of the pfmdrl gene (4). All these results overexpressed the pfmdrl gene and its protein product (Pghl). suggested an inverse relationship between chloroquine and Macrorestriction maps of chromosome 5, where pfindrl is mefloquine resistance and a direct link with the level of Pghl encoded, showed that this chromosome has increased in size in expression. In this study we have selected two cloned lines response to mefloquine selection, indicating the presence of a of P. falciparum for increased mefloquine resistance and gene(s) in this area of the genome that confers a selective show that this has resulted in increased expression of the advantage in the presence ofmefloquine. -

Guidelines for Treatment of Malaria in the United States 1 (Based on Drugs Currently Available for Use in the United States — October 1, 2019)
Guidelines for Treatment of Malaria in the United States 1 (Based on drugs currently available for use in the United States — October 1, 2019) CDC Malaria Hotline: (770) 488-7788 or (855) 856-4713 (toll free) Monday–Friday, 9 am to 5 pm EST; (770) 488-7100 after hours, weekends, and holidays Clinical Diagnosis/ Drug Susceptibility (Based on Recommended Regimen and Adult Dose1 Recommended Regimen and Pediatric Dose1 Plasmodium Species Region Infection Was Acquired) Pediatric dose should NEVER exceed adult dose Uncomplicated malaria/ Chloroquine resistance or unknown A. Artemether-lumefantrine (Coartem™)3,4 P. falciparum, or resistance2 Tablet=20mg artemether/ 120 mg lumefantrine species not identified All malarious regions except those specified A 3-day treatment schedule with a total of 6 oral doses is recommended for both adult and pediatric patients based on as chloroquine sensitive listed in the box weight. The patient should receive the initial dose, followed by the second dose 8 hours later, then 1 dose bid for the If “species not identified” below following 2 days. Dosing as follows: is later diagnosed as P. 5–<15 kg: 1 tablet per dose vivax or P. ovale, please 15–<25 kg: 2 tablets per dose see P. vivax and P. ovale 25–<35 kg: 3 tablets per dose (below) re: treatment with ≥35 kg: 4 tablets per dose primaquine or tafenoquine B. Atovaquone-proguanil (Malarone™)4,5 B. Atovaquone-proguanil (Malarone™)4,5 Adult tablet= 250 mg atovaquone/ 100 mg proguanil Adult tab=250 mg atovaquone/ 100 mg proguanil 4 adult tabs po qd x 3 days Peds tab=62.5 mg atovaquone/ 25 mg proguanil 5–<8 kg: 2 peds tabs po qd x 3 days 8–<10 kg: 3 peds tabs po qd x 3 days 10–<20 kg: 1 adult tab po qd x 3 days 20–<30 kg: 2 adult tabs po qd x 3 days 30–<40 kg: 3 adult tabs po qd x 3 days ≥40 kg: 4 adult tabs po qd x 3 days C. -

Malaria Chemotherapy & Drug Resistance
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike License. Your use of this material constitutes acceptance of that license and the conditions of use of materials on this site. Copyright 2006, The Johns Hopkins University and David Sullivan. All rights reserved. Use of these materials permitted only in accordance with license rights granted. Materials provided “AS IS”; no representations or warranties provided. User assumes all responsibility for use, and all liability related thereto, and must independently review all materials for accuracy and efficacy. May contain materials owned by others. User is responsible for obtaining permissions for use from third parties as needed. Malaria Chemotherapy and Drug Resistance David Sullivan, MD Eradication Attempts •Hookworm1909-1924: Sanitation and drug treatment; no reduction in 15 yrs. • Yellow Fever 1915-1930s: Mosquito control; discovery of natural reservoir in jungle animals ceased efforts. •Yaws1940-1960: Mass screening and penicillin; continued spread after best efforts. •Malaria1955-1975: DDT & chloroquine; $2 billion spent; insecticide resistance & African failure of DDT ceased efforts. • Smallpox 1967-1977: Successful vaccine heat stable and 99% effective as single dose; no hidden carriers. • Dracunculiasis 1986-?: 3.5 million to 100,000; Sudan - 605 of current cases; Nigeria increase; surveillance and water control • Polio 1985-?: Gone from western hemisphere; problematic in Congo, Sudan, and Afghanistan; vaccination- and surveillance- based control. If Not Eradication, Then Control! "At this time one must question the wisdom of even contemplating another eradication effort until the two eradication programs now in progress have been successfully concluded, until the lessons from those programs have been digested and until the savings from polio eradication have begun to be realized. -

Therapeutic Properties and Serum Iron in T. Brucei Infected Rats Treated with Amodiaquine and Mefloquine
An international journal published by the BIOKEMISTRI 17(2):115-121 (Dec 2005) Available online at http://www.bioline.org.br/bk. Abstracted online at www.ajol.info/journals/biokem N ig erian S oc iety for E x perim ental B iolog y Printed in Nigeria Therapeutic properties and serum iron in T. brucei infected rats treated with amodiaquine and mefloquine Justine T. EKANEM*, Faoziyat A. SULAIMAN and Oluyomi ADEYEMI Trypanosomosis Research Unit, Department of Biochemistry, University of Ilorin, Ilorin, Nigeria Received 28 December 2004 MS/No BKM/2004/039, © 2005 Nigerian Society for Experimental Biology. All rights reserved. --------------------------------------------------------------------------------------------------------------------------------------- Abstract Serum iron was monitored in Trypanosoma brucei-infected rats treated with Amodiaquine and mefloquine antimalarials as the infection progressed. The chemotherapeutic properties of the drugs against African sleeping sickness were also assessed. Results show gradual reduction in the levels of serum iron in the infected but treated rats as the infection progressed. Results also show that reduction in serum iron level is more pronounced in amodiaquine treated but uninfected rats than the mefloquine treated rats. Serum level in infected but not treated rats increased steadily from the day of infection. For prophylactic treatments of infected rat, amodiaquine extended the lifespan of the rats for 14 days while mefloquine extended it for 7 days. For early stage treatment, amodiaquine and mefloquine extended life span for 7 and 4 days respectively while late stage treatment the extensions were 2 and 1 day respectively. Results suggest that these antimalarials especially amodiaquine could be useful in the clinical management of African sleeping sickness and that this may be through reduction of blood iron level, a situation that can inhibit ribonucleotide reductase of the proliferating parasites. -

Treatment of Malaria in the United States a Systematic Review
CLINICAL REVIEW CLINICIAN’S CORNER Treatment of Malaria in the United States A Systematic Review Kevin S. Griffith, MD, MPH Context Many US clinicians and laboratory personnel are unfamiliar with the diag- Linda S. Lewis, DVM, MPVM nosis and treatment of malaria. Sonja Mali, MPH Objectives To examine the evidence base for management of uncomplicated and severe malaria and to provide clinicians with practical recommendations for the diag- Monica E. Parise, MD nosis and treatment of malaria in the United States. VEN THOUGH ENDEMIC MALARIA Evidence Acquisition Systematic MEDLINE search from 1966 to 2006 using the has been eliminated from the search term malaria (with the subheadings congenital, diagnosis, drug therapy, epi- United States, it remains a lead- demiology, and therapy). Additional references were obtained from searching the bib- ing infectious disease world- liographies of pertinent articles and by reviewing articles suggested by experts in the Ewide. As a consequence, every year in treatment of malaria in North America. the United States an average 1200 cases Evidence Synthesis Important measures to reduce morbidity and mortality from of malaria are reported, almost all im- malaria in the United States include the following: obtaining a travel history, consid- ported, resulting in up to 13 deaths per ering malaria in the differential diagnosis of fever based on the travel history, and year.1 The unfamiliarity of US clini- prompt and accurate diagnosis and treatment. Chloroquine remains the treatment cians and laboratory personnel with ma- of choice for Plasmodium falciparum acquired in areas without chloroquine- resistant strains. In areas with chloroquine resistance, a combination of atovaquone laria and drug resistance patterns has and proguanil or quinine plus tetracycline or doxycycline or clindamycin are the best contributed to delays in diagnosis and treatment options. -

Common Study Protocol for Observational Database Studies WP5 – Analytic Database Studies
Arrhythmogenic potential of drugs FP7-HEALTH-241679 http://www.aritmo-project.org/ Common Study Protocol for Observational Database Studies WP5 – Analytic Database Studies V 1.3 Draft Lead beneficiary: EMC Date: 03/01/2010 Nature: Report Dissemination level: D5.2 Report on Common Study Protocol for Observational Database Studies WP5: Conduct of Additional Observational Security: Studies. Author(s): Gianluca Trifiro’ (EMC), Giampiero Version: v1.1– 2/85 Mazzaglia (F-SIMG) Draft TABLE OF CONTENTS DOCUMENT INFOOMATION AND HISTORY ...........................................................................4 DEFINITIONS .................................................... ERRORE. IL SEGNALIBRO NON È DEFINITO. ABBREVIATIONS ......................................................................................................................6 1. BACKGROUND .................................................................................................................7 2. STUDY OBJECTIVES................................ ERRORE. IL SEGNALIBRO NON È DEFINITO. 3. METHODS ..........................................................................................................................8 3.1.STUDY DESIGN ....................................................................................................................8 3.2.DATA SOURCES ..................................................................................................................9 3.2.1. IPCI Database .....................................................................................................9