Traveler Information
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Artemether-Lumefantrine (Six-Dose Regimen) for Treating Uncomplicated Falciparum Malaria (Review)
Artemether-lumefantrine (six-dose regimen) for treating uncomplicated falciparum malaria (Review) Omari AAA, Gamble CL, Garner P This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2009, Issue 1 http://www.thecochranelibrary.com Artemether-lumefantrine (six-dose regimen) for treating uncomplicated falciparum malaria (Review) Copyright © 2009 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 BACKGROUND .................................... 2 OBJECTIVES ..................................... 3 METHODS ...................................... 3 RESULTS....................................... 5 DISCUSSION ..................................... 9 AUTHORS’CONCLUSIONS . 9 ACKNOWLEDGEMENTS . 10 REFERENCES ..................................... 10 CHARACTERISTICSOFSTUDIES . 13 DATAANDANALYSES. 20 Analysis 1.1. Comparison 1 Artemether-lumefantrine vs amodiaquine, Outcome 1 Total failure by day 28. 22 Analysis 1.2. Comparison 1 Artemether-lumefantrine vs amodiaquine, Outcome 2 Total failure by day 14. 23 Analysis 1.3. Comparison 1 Artemether-lumefantrine vs amodiaquine, Outcome 3 Gametocyte carriage on day 14. 23 Analysis 2.1. Comparison 2 Artemether-lumefantrine vs chloroquine plus sulfadoxine-pyrimethamine, Outcome 1 Total failurebyday28. ................................ 24 Analysis 2.2. Comparison 2 Artemether-lumefantrine -
Quinoline-Based Hybrid Compounds with Antimalarial Activity
molecules Review Quinoline-Based Hybrid Compounds with Antimalarial Activity Xhamla Nqoro, Naki Tobeka and Blessing A. Aderibigbe * Department of Chemistry, University of Fort Hare, Alice Campus, Alice 5700, Eastern Cape, South Africa; [email protected] (X.N.); [email protected] (N.T.) * Correspondence: [email protected] Received: 7 November 2017; Accepted: 11 December 2017; Published: 19 December 2017 Abstract: The application of quinoline-based compounds for the treatment of malaria infections is hampered by drug resistance. Drug resistance has led to the combination of quinolines with other classes of antimalarials resulting in enhanced therapeutic outcomes. However, the combination of antimalarials is limited by drug-drug interactions. In order to overcome the aforementioned factors, several researchers have reported hybrid compounds prepared by reacting quinoline-based compounds with other compounds via selected functionalities. This review will focus on the currently reported quinoline-based hybrid compounds and their preclinical studies. Keywords: 4-aminoquinoline; 8-aminoquinoline; malaria; infectious disease; hybrid compound 1. Introduction Malaria is a parasitic infectious disease that is a threat to approximately half of the world’s population. This parasitic disease is transmitted to humans by a female Anopheles mosquito when it takes a blood meal. Pregnant women and young children in the sub-tropical regions are more prone to malaria infection. In 2015, 214 million infections were reported, with approximately 438,000 deaths and the African region accounted for 90% of the deaths [1–3]. Malaria is caused by five parasites of the genus Plasmodium, but the majority of deaths are caused by Plasmodium falciparum and Plasmodium vivax [1,4–6]. -

Information for the User Riamet® 20 Mg/120 Mg Tablets Artemether And
Package leaflet: Information for the user Riamet® 20 mg/120 mg tablets artemether and lumefantrine Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor or pharmacist. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. (See section 4). What is in this leaflet 1. What Riamet is and what it is used for 2. What you need to know before you take Riamet 3. How to take Riamet 4. Possible side effects 5. How to store Riamet 6. Contents of the pack and other information 1. What Riamet is and what it is used for Riamet contains two substances called artemether and lumefantrine. They belong to a group of medicines called anti-malarials. Riamet is only used for the treatment of acute uncomplicated malaria infections caused by a parasite called “Plasmodium falciparum”. This parasite is a tiny organism made up of one cell that is found inside red blood cells. Riamet is used to treat adults, children and infants of 5 kg body weight and above. Riamet is not used to prevent malaria or to treat severe malaria (where it has affected the brain, lungs or kidneys). -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Artemether-Lumefantrine Compared to Atovaquone-Proguanil As a Treatment for Uncomplicated Plasmodium Falciparum Malaria in Travelers
Am. J. Trop. Med. Hyg., 92(1), 2015, pp. 13–17 doi:10.4269/ajtmh.14-0249 Copyright © 2015 by The American Society of Tropical Medicine and Hygiene Artemether-Lumefantrine Compared to Atovaquone-Proguanil as a Treatment for Uncomplicated Plasmodium falciparum Malaria in Travelers Shirly Grynberg, Tamar Lachish, Eran Kopel, Eyal Meltzer, and Eli Schwartz* The Center of Geographic Medicine and Tropical Diseases, Sheba Medical Center, Tel Hashomer, Israel; The Infectious Diseases Unit, Shaare-Zedek Medical Center, Jerusalem, Israel; The Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel Abstract. Atovaquone-proguanil (AP) and artemether-lumefantrine (AL) are both treatments for uncomplicated Plasmodium falciparum malaria, but comparative clinical trials are lacking. We performed a retrospective analysis, comparing treatment failure and fever clearance time in non-immune travelers with uncomplicated P. falciparum malaria, treated with AP or AL. Sixty-nine patients were included during 2001–2013: 44 in the AP group and 25 in the AL group. Treatment failure was observed in 6 of 44 (13.6%) and 1 of 25 (4.0%) patients in the AP and AL groups, respectively. Six treatment failures were observed in travelers from West Africa. Fever clearance time was 44 ± 23 h in AL group versus 77 ± 28 h in AP group, (P < 0.001). Hospitalization time was significantly shorter in the AL group; 3.8 + 1.3 versus 5.1 + 2.8 days in the AP group (P = 0.04) In conclusion, travelers with uncomplicated P. falciparum malaria recover faster on AL than on AP. The AL should probably be the drug of choice for this population. -

Resistance to Antimalarial Drugs: Molecular, Pharmacologic, and Clinical Considerations
0031-3998/09/6505-0064R Vol. 65, No. 5, Pt 2, 2009 PEDIATRIC RESEARCH Printed in U.S.A. Copyright © 2009 International Pediatric Research Foundation, Inc. Resistance to Antimalarial Drugs: Molecular, Pharmacologic, and Clinical Considerations MARK A. TRAVASSOS AND MIRIAM K. LAUFER Center for Vaccine Development, University of Maryland School of Medicine, Baltimore, Maryland 21201 ABSTRACT: One of the greatest obstacles to the control of hematin, a toxic byproduct of Hb degradation, in the Plasmo- malaria has been the spread of resistance to drugs used on a large dium parasite’s food vacuole. Although it is no longer recom- scale. This review provides an update of the current understanding mended for the treatment of P. falciparum, it is the drug of of the molecular basis for antimalarial drug resistance. Parasite choice to treat P. vivax and P. ovale, less severe forms of intrinsic resistance is just one component that determines the in vivo efficacy of a drug. Human immune responses and pharmaco- malaria that can cause recurrent infections. logic properties play important roles in determining the clinical With the spread of chloroquine resistance, many countries outcome of treatment. The emergence and spread of resistance adopted SP as the first-line antimalarial treatment. SP is com- also results from an interplay of these factors. Current efforts to posed of two drugs that act on sequential enzymes in the folate characterize and deter resistance to new combination therapy are synthesis pathway. When both drugs are used together, they act also discussed. (Pediatr Res 65: 64R–70R, 2009) synergistically. Although SP is a coformulation of two drugs, it is not considered combination therapy because the mechanisms of ne of the greatest obstacles to the control of malaria has action are closely linked. -

(Artemether / Lumefantrine 20Mg/120 Mg) Tablets
SUMMARY OF PRODUCT CHARACTERISTICS Page 1 of 13 1. NAME OF THE MEDICINAL PRODUCT Lumartem (Artemether / Lumefantrine 20mg/120 mg) Tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains: 20 mg artemether and 120 mg lumefantrine. For a full list of excipients see section 6.1. 3. PHARMACEUTICAL FORM Yellow coloured, circular, uncoated, flat faced, bevelled edged, matt finished tablets with a break line on one side and plain on the other side. The scoreline is only to facilitate breaking for ease of swallowing and not to divide into equal doses. 4. CLINICAL PARTICULARS 4.1 Therapeutic indication Artemether 20 mg and Lumefantrine 120 mg Tablets is indicated for the treatment of uncomplicated cases of malaria due to Plasmodium falciparum in adults, children and infants of 5 kg and above. The most recent official guidelines on the appropriate use of antimalarial agents and local information on the prevalence of resistance to antimalarial drugs must be taken into consideration for deciding on the appropriateness of therapy with Artemether 20 mg and Lumefantrine 120 mg Tablets. Official guidance will normally include WHO (http://whqlibdoc.who.int/publications/2010/9789241547925_eng.pdf) and local health authorities’ guidelines (see also sections 4.4 and 5.1). 4.2 Posology and method of administration Tablets for oral administration. Page 2 of 13 Number of Artemether 20 mg and Lumefantrine 120 mg Tablets for treatment according to weight bands st nd rd Weight range 1 day of 2 day of 3 day treatment treatment of treatment ≥ 5kg -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

10 Artemether-Lumefantrine for The
PEDIATRIC PHARMACOTHERAPY A Monthly Newsletter for Health Care Professionals from the University of Virginia Children’s Hospital Volume 16 Number 10 October 2010 Artemether-Lumefantrine for the Treatment of Malaria in Infants and Children Marcia L. Buck, Pharm.D., FCCP, FPPAG alaria remains a significant medical break-down, to non-toxic hemozoin. M burden in many parts of the world. It is Accumulation of heme and free radicals results in responsible for approximately 1 million deaths parasite death.1-5 per year, mostly in infants and children. The availability of artemisinin-based compounds, Artemether, like other artemisinin-derived derived from the Chinese plant Artemisia annua, compounds, acts quickly to rapidly reduce the during the past decade has introduced a new era parasite burden, while lumefantrine serves as a in the treatment of this disease. Effective and longer-acting agent to eliminate remaining well tolerated, these drugs appear to offer parasites. The combination is effective in strains substantial benefits over traditional agents such known to be resistant to traditional antimalarials as chloroquine or sulfadoxine-pyrimethamine. such as chloroquine, and can be used for Artemisinin-based combination therapies (ACT) infections acquired in areas known to have are recommended as first-line therapy for malaria parasites that are multidrug-resistant.1-5 by the World Health Organization (WHO) and have been accepted as a mainstay of treatment in Pharmacokinetics more than 70 countries.1-3 Both artemether and lumefantrine are well absorbed after oral administration. Peak plasma A combination of artemether and lumefantrine artemether concentrations typically occur within recently became the first ACT to be made 2 hours after administration and peak available in the United States. -

Malaria Treatment
TREATMENT OF MALARIA IN ADULT AND PEDIATRIC PATIENTS WHO recommendations are to treat uncomplicated malaria from all species with artemisinin-based combination therapy (such as Coartem™) based on safety and effectiveness of the drug, as well as to help streamline treatment recommendations for malaria. CDC and WHO treatment guidelines now concur with recommendations for Coartem™ as first line agent with known chloroquine resistance or species not identified. The CDC currently recommends chloroquine- containing regimens as first line therapy for chloroquine-susceptible species of malaria, which differs from WHO recommendations. We have elected to streamline institutional recommendations to be in line with WHO recommendations when there is discrepancy, given local drug availability and that Coartem™ clears parasitemia faster than chloroquine. Definitions Uncomplicated malaria: Persons with a positive blood smear OR history of recent possible exposure and no other recognized pathology who do not meet severe criteria Severe malaria: Persons with a positive blood smear OR history of recent possible exposure and no other recognized pathology who have one or more of the following clinical criteria: Parasitemia of >5% Renal failure Disseminated intravascular Jaundice Impaired Pulmonary edema coagulation Repeated generalized consciousness/coma Acute respiratory distress Spontaneous bleeding convulsions Severe normocytic syndrome Acidosis anemia Circulatory shock Hemoglobinuria Chloroquine sensitivity: P. falciparum acquired in Central America (west of the Panama Canal), Haiti, and Dominican Republic All P. malariae, P. knowlesi, and P. ovale All P. vivax EXCEPT infections acquired in Papua New Guinea or Indonesia Uncomplicated malaria P. falciparum or not identified P. malariae or P. knowlesi P. vivax or P. ovale chloroquine sensitive P. -
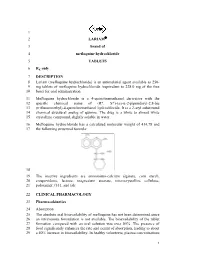
1 2 LARIAM 3 Brand of 4 Mefloquine Hydrochloride 5 TABLETS 6 Rx Only
1 2 LARIAM® 3 brand of 4 mefloquine hydrochloride 5 TABLETS 6 Rx only 7 DESCRIPTION 8 Lariam (mefloquine hydrochloride) is an antimalarial agent available as 250 9 mg tablets of mefloquine hydrochloride (equivalent to 228.0 mg of the free 10 base) for oral administration. 11 Mefloquine hydrochloride is a 4-quinolinemethanol derivative with the 12 specific chemical name of (R*, S*)-(±)-α-2-piperidinyl-2,8-bis 13 (trifluoromethyl)-4-quinolinemethanol hydrochloride. It is a 2-aryl substituted 14 chemical structural analog of quinine. The drug is a white to almost white 15 crystalline compound, slightly soluble in water. 16 Mefloquine hydrochloride has a calculated molecular weight of 414.78 and 17 the following structural formula: 18 19 The inactive ingredients are ammonium-calcium alginate, corn starch, 20 crospovidone, lactose, magnesium stearate, microcrystalline cellulose, 21 poloxamer #331, and talc. 22 CLINICAL PHARMACOLOGY 23 Pharmacokinetics 24 Absorption 25 The absolute oral bioavailability of mefloquine has not been determined since 26 an intravenous formulation is not available. The bioavailability of the tablet 27 formation compared with an oral solution was over 85%. The presence of 28 food significantly enhances the rate and extent of absorption, leading to about 29 a 40% increase in bioavailability. In healthy volunteers, plasma concentrations 1 LARIAM® (mefloquine hydrochloride) 30 peak 6 to 24 hours (median, about 17 hours) after a single dose of Lariam. In a 31 similar group of volunteers, maximum plasma concentrations in μg/L are 32 roughly equivalent to the dose in milligrams (for example, a single 1000 mg 33 dose produces a maximum concentration of about 1000 μg/L). -

Selection for Mefloquine Resistance in Plasmodium Falciparum Is Linked To
Proc. Nati. Acad. Sci. USA Vol. 91, pp. 1143-1147, February 1994 Medical Sciences Selection for mefloquine resistance in Plasmodium falciparum is linked to amplification of the pfmdrl gene and cross-resistance to halofantrine and quinine (drug reistance/malaria/P-glycoprotein/chloroquine) ALAN F. COWMAN*, DENISE GALATIS, AND JENNIFER K. THOMPSON The Walter and Eliza Hall Institute of Medical Research, Melbourne 3050, Australia Communicated by Gustav J. V. Nossal, October 11, 1993 (received for review September 8, 1993) ABSTRACT Two chloroquine-resistant cloned isolates of concomitant with the increase in chloroquine resistance was Plasmodiumfalciparum were subjected to mefloquine selection a decrease in the level of mefloquine resistance. In another to test if this resulted in alterations in chloroquine sensitivity study, selection for mefloquine resistance in the W2 isolate of and amplification ofthepfmdrl gene. The mefloquine-resistant P. falciparum showed a decrease in chloroquine resistance lines derived by this selection were shown to have amplified and (8) and amplification of the pfmdrl gene (4). All these results overexpressed the pfmdrl gene and its protein product (Pghl). suggested an inverse relationship between chloroquine and Macrorestriction maps of chromosome 5, where pfindrl is mefloquine resistance and a direct link with the level of Pghl encoded, showed that this chromosome has increased in size in expression. In this study we have selected two cloned lines response to mefloquine selection, indicating the presence of a of P. falciparum for increased mefloquine resistance and gene(s) in this area of the genome that confers a selective show that this has resulted in increased expression of the advantage in the presence ofmefloquine.